Pulmonary fibrosis - a process in which tissue grows - it gradually replaces alveolar tissue. The disease is dangerous because the patient suffers from respiratory failure, and the level of oxygen deficiency can shift to critical. The tissue that makes up the lungs loses volume, natural elasticity and stretchability. The compaction prevents normal gas exchange, and the patient experiences difficulty breathing due to the fact that oxygen and carbon dioxide cannot fully penetrate the walls of the alveoli. As a result, the lungs gradually lose their ability to function normally. How exactly the disease progresses largely depends on the location of the compaction, as well as on the causes that provoked the disease.
Lung tissue fibrosis can occur in one or both lungs. Therefore, there are several types of pathology: unilateral or bilateral. Also, the pathology can be focal or total. In the first case, a relatively small area of the lung suffers, in the second, the pathological process affects the entire organ.
Causes of the disease
Fibrosis can occur due to various reasons, for example:
- Diseases associated with the respiratory system. As a rule, they occur in a chronic form: bronchitis, pneumonia, tuberculosis, etc.
- Connective tissue pathologies.
- The presence of external factors such as unfavorable environmental conditions, hazardous production.
- Long-term treatment with certain medications.
- Vasculitis.
The prognosis of the disease is unfavorable, and if measures are not taken, progression is observed, leading to pneumosclerosis and cirrhosis of the lungs. This significantly affects life expectancy and also reduces its quality.
Description
Pulmonary fibrosis is a process characterized by the replacement of lung tissue with fibrous (scar) tissue, which is accompanied by impaired respiratory function.
Thanks to the work of our lungs, the blood is saturated with oxygen necessary for energy consumption, as well as the release of carbon dioxide, which is formed as a by-product during the life of cells. The development of pulmonary fibrosis leads to a decrease in the volume of normally functioning lung tissue, and as a result, breathing efficiency decreases.
Replacement of pulmonary connective tissue can occur in one lung or in both at the same time. Depending on this, unilateral and bilateral fibrosis are distinguished. In addition, pulmonary fibrosis is divided into focal, in which a small area of lung tissue is affected, and total, in which the pathological process spreads to almost the entire lung.
The reasons for the development of pulmonary fibrosis are varied:
- diseases of the respiratory system (chronic bronchitis with broncho-obstructive syndrome, pneumonia, tuberculosis, chronic obstructive pulmonary disease);
- connective tissue diseases (rheumatoid arthritis, systemic lupus erythematosus, systemic scleroderma);
- exposure to production factors that negatively affect the respiratory system. For example, with prolonged inhalation of silicate dust in production, silicosis occurs. Occupational diseases also include asbestosis, which occurs due to inhalation of asbestos dust;
- long-term use of certain medications (antiarrhythmic drugs, drugs used to treat malignant tumors);
- the presence of vasculitis (a disease accompanied by inflammation of the walls of blood vessels);
- idiopathic or primary pulmonary fibrosis, the exact cause of which has not been established.
The prognosis of the disease is relatively unfavorable; progression of the pathological process leads to the development of pneumosclerosis and then cirrhosis of the lungs, which significantly reduces a person’s quality of life and can lead to disability. In addition, this condition leads to such serious complications as chronic respiratory failure, pulmonary hypertension, and chronic heart failure. Therefore, it is extremely important to contact a specialist as early as possible, who, in turn, will prescribe the necessary range of diagnostic procedures and necessary treatment.
Symptoms of pulmonary fibrosis
At the first stage, the symptoms of pulmonary fibrosis include general malaise, decreased productivity, and fatigue. The skin turns pale, sometimes a bluish tint appears - this symptom often occurs on the fingers of the lower and upper extremities, above the upper lip. The patient suffers from insomnia, or, on the contrary, constantly wants to sleep. Shortness of breath also occurs, which occurs even in a calm state. Some patients experience rapid weight loss. Moreover, there is a risk of developing a dry cough, during which a small amount of sputum is released.
If pulmonary fibrosis is left untreated , it provokes changes in the shape of the fingers - the phalanges thicken and become spherical, and the nail plate becomes triangular.
Severe lung damage and lack of supportive therapy can cause heart failure. The condition is called cor pulmonale, which is manifested by the following symptoms:
- The feet become swollen. Gradually the swelling spreads to the knees and thighs.
- There is progressive shortness of breath.
- The veins in the neck enlarge and pulsation is noticeable.
- The patient experiences pain or discomfort in the heart area.
Degrees of liver fibrosis
The severity of fibrosis in chronic liver disease reflects the long-term prognosis and, therefore, the need and urgency of treatment.
Liver fibrosis has 5 degrees (stages): F0, F1, F2, F3, F4 (cirrhosis). With viral hepatitis, for example, on average, it takes about 5 years from stage to stage. However, in later stages the rate of progression of fibrosis is higher. The rate of fibrosis development depends on the activity of the inflammatory process in the liver.
To determine the severity of fibrosis, there are various methods: biopsy, blood test, which measures biochemical markers of fibrosis formation ( FibroTest, FibroMax ). Currently, elastometry - direct ultrasound determination of the density of liver tissue using the Fibroscan device. The resulting density measurements at several points (10-20) in kiloPascals correspond to the degrees of fibrosis on the METAVIR scale from F0 - healthy liver, to F4 - cirrhosis.
A sufficient amount of scientific data has been obtained using this method and it has been proven that as the stage of fibrosis increases, the elasticity of the liver in kPa increases.
Legend:
- F 0-3 stages of fibrosis according to the METAVIR scale for chronic hepatitis,
- F 4 – cirrhosis of the liver,
- F 4+ URVP - cirrhosis of the liver with the presence of varicose veins of the esophagus,
- F 4+VRVP* - liver cirrhosis, portal hypertension, complicated by bleeding from varicose veins of the esophagus,
- HCC - hepatocellular carcinoma
Significance of differences p <0.05
Legend:
- F 0-3 stages of fibrosis according to the METAVIR scale for chronic hepatitis,
- F 4 – cirrhosis of the liver,
- F 4+ URVP - cirrhosis of the liver with the presence of varicose veins of the esophagus,
- F 4+VRVP* - liver cirrhosis, portal hypertension, complicated by bleeding from esophageal varices
The advantages of the method include simplicity, non-invasiveness, low cost, as well as clinical significance (prediction of complications of portal hypertension in liver cirrhosis, liver cancer formation). This determines broad indications for the method: initial examination, dynamics with and without treatment.
Limitations to the method are the presence of ascites, excess fatty tissue, and narrow intercostal spaces in the patient.
The results of Russian studies also confirmed high diagnostic accuracy (more than 80% for all groups) and reproducibility of the result by another operator.
The following elasticity thresholds are recommended for clinical use:
- 5.8 kPa to determine the boundary between stages F0 and F1 (METAVIR);
- 7.2 kPa to differentiate stages F1 and F2;
- 9.5 kPa – stages F2 and F3;
- 12.5 kPa to determine the boundary between severe fibrosis and cirrhosis of the liver - F4.
Factors influencing the diagnostic accuracy of elastometry:
- patient age >50 years,
- excess body weight,
- the presence of steatosis according to a morphological study of liver tissue.
Diagnostics
Diagnosis of pulmonary fibrosis is accompanied by anamnesis. The doctor pays attention to shortness of breath, which can appear both with and without exertion. The specialist also finds out whether the patient has diseases that provoke fibrosis, for example, bronchial asthma, chronic bronchitis.
After a conversation with a visitor to the office, the doctor conducts an examination. He pays attention to the skin, the presence of swelling, changes in the shape of the fingers and toes. Next, listen and tap the lungs.
The doctor also prescribes a number of laboratory tests that will help establish an accurate diagnosis. This is a urine and blood test, biochemistry. Spirography is also prescribed, which allows you to determine the exact volume of the lungs and the speed at which the patient exhales air.
To visualize the disease, a chest x-ray is taken - as part of the study, it is possible to identify changes in the organ. If necessary, computed tomography and MRI are prescribed. If the patient is in serious condition, these techniques make it possible to quickly establish a diagnosis and begin treatment. In difficult cases, a biopsy is performed, which can confirm the presence of scar tissue.
Folk remedies
Photo: narodnimisredstvami.ru
First of all, measures should be taken to prevent the development of pulmonary fibrosis. In many cases, pulmonary fibrosis is caused by diseases of the respiratory system, in particular pneumonia, which can lead to the replacement of lung tissue with connective tissue in the absence of treatment, the patient’s self-cancellation of antibacterial therapy, or failure to follow doctor’s recommendations. Therefore, it is extremely important, when the first symptoms of the disease appear, not to neglect your condition, but to consult a specialist and strictly follow his instructions. In addition, diseases such as chronic bronchitis with the phenomenon of bronchial obstruction, bronchiectasis of the lungs, chronic obstructive pulmonary disease, with a long course of the process, can also lead to the development of fibrosis. Considering this, it is important to avoid factors whose impact on the body leads to an exacerbation of the process. For the same purpose, annual influenza vaccination is recommended. People who are forced to use antiarrhythmic drugs for a long time need to be attentive to the appearance of symptoms from the respiratory system. If they are detected, you should immediately seek help from a doctor, and it is strongly recommended not to forget about an annual chest x-ray examination.
Special attention should be paid to people working in industries with occupational hazards. Long-term inhalation of organic and inorganic dust leads to the development of lung diseases, ultimately leading to fibrosis. Therefore, you should not neglect safety precautions, in particular the use of special devices that protect the upper parts of the respiratory system.
Traditional medicine recipes help to some extent alleviate the general condition of a person suffering from pulmonary fibrosis. For example, a decoction of rose hips and elecampane root has an excellent effect. To prepare it, grind the listed components, then pour 4 tablespoons of dry raw materials with 4 glasses of water and put on low heat. After boiling, keep it on the fire for another 15 minutes. Then the resulting broth is poured into a thermos and infused for 3 hours, after which it is carefully filtered. It is recommended to take half a glass 3 times a day before meals. The course of treatment is from 1 to 2 months. It is important not to interrupt the course of treatment and always have a ready-made remedy on hand. The combination of rosehip and elecampane helps to liquefy mucus, thereby making it easier to separate. In addition, this decoction protects lung tissue from inflammatory processes.
A recipe using anise seed is also widely used. To prepare this product, you should first prepare 1 tablespoon of anise seeds, which are poured with 1 glass of cold water. The resulting mixture is placed on the fire and brought to a boil, after which it is immediately removed from the stove. It is recommended to use the resulting product half a glass once a day.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
SEARCH FOR TREATMENT AROUND THE WORLD WITH YELLMED
Pulmonary fibrosis after coronavirus
Pulmonary fibrosis after Covid is one of the complications that occurs after the virus. Penetrating into the body, it causes severe inflammation, which is why the immune system uses every opportunity to destroy the virus. However, this response triggers the release of inflammatory cytokines. It is the activity of these elements that makes it possible to determine the extent of lung damage. As part of the coronavirus, the alveoli and pulmonary vessels are affected.
After suffering from the virus, the lungs become less elastic, the damaged tissue is replaced by scar tissue and fibrosis forms. Despite the fact that the inflammation has been eliminated, breathing difficulties continue. If left untreated, fibrosis can progress.
With pulmonary fibrosis after coronavirus, the patient may complain of:
- Shortness of breath that appears even when talking.
- Headaches and dizziness.
- Dry cough.
- Weakness and feeling of fatigue.
- Low level of endurance and performance.
Treatment
Photo: assets.copdnewstoday.com
Focal pulmonary fibrosis, which does not manifest itself clinically and does not cause discomfort to the patient, does not require treatment. Often, the focus of fibrosis is detected by chance during a preventive X-ray examination of the lungs. If it is detected, it is recommended to monitor the dynamics of the process and not delay contacting a specialist if symptoms from the respiratory system appear.
Total fibrosis requires the prescription of drugs with antifibrotic activity. The use of these drugs makes it possible to reduce the proliferation of fibrous tissue, which has a beneficial effect on the course of the disease.
In addition, we should not forget about the importance of specially designed physical training, which can improve lung function as much as possible, resulting in increased oxygen saturation in the blood.
Oxygen therapy (oxygen therapy) is used to eliminate oxygen deficiency. Oxygen is indispensable in the process of cellular respiration necessary for human life. With pulmonary fibrosis, blood oxygen saturation is significantly reduced. To compensate for this condition, courses of oxygen therapy are prescribed. However, it is also important to know that with frequent use of pure oxygen or inhalation mixtures with high oxygen concentrations, oxygen toxicity can develop. This condition is manifested by dry mouth, dry cough, chest pain, and in some cases there is a convulsive syndrome, which indicates hypertoxic damage to the brain. To prevent oxygen intoxication, it is important to strictly follow accepted standards and carefully monitor changes in the patient’s condition during an oxygen therapy session.
If the above treatment methods do not provide adequate effectiveness, the question of lung transplantation arises. There are certain indications for such a complex operation:
- significant decrease in vital capacity of the lungs;
- decrease in the diffusion capacity of the lungs by more than 2 times;
- respiratory failure in the stage of decompensation.
Such a solution to the problem in some situations is the only way to prolong a person’s life. According to statistics, most patients who have undergone lung transplantation have had their lives extended by 5 years or more. After such a complex operation, patients should periodically consult a therapist and pulmonologist. This is necessary to assess the general condition of the body and the functioning of the transplanted lungs.
Treatment of pulmonary fibrosis in Kaliningrad
If you are bothered by a cough, shortness of breath, wheezing, or need a preventive examination, make an appointment with us for a consultation. The Pulmonology Center is staffed by competent, responsible and caring paid pulmonologists.
We offer:
- personal approach to each patient;
- rapid laboratory diagnosis of lung diseases;
- safe therapy at any stage of treatment: treatment of COPD, asthma;
- recovery programs, including rehabilitation after coronavirus in Kaliningrad.
Make an appointment at the Pulmonology Center by phone 8 (4012) 971-961.
General information
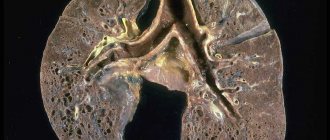
Fibrous changes in the lungs, what is it?
This is a pathological process of the formation of fibrous tissue (connective tissue) that replaces lung tissue, which leads to disruption of the elasticity of the lung and the function of gas exchange. With the formation of fibrous changes (synonymous with “pneumofibrosis”), elasticity is irreversibly lost. Fibrous changes in the lungs are the outcome of many diseases of the bronchopulmonary system, and also occur in other diseases. As pneumofibrosis progresses, a gradual restructuring of the lung tissue occurs - the structure of the acinus , sclerosis of the walls of the bronchioles develops, the capillary network becomes empty, and abnormal glandular structures are formed. These changes destroy and deform the lung tissue, and cyst-like expansions and fibrous fields are formed in this place. Areas of fibrosis can occur around the lymphatic vessels, in the interlobular septa, along the outflow of lymph from foci of former inflammation, in the tissue around the bronchi and blood vessels.
The further course of the disease and prognosis depend on the type of pulmonary fibrosis and the degree of its spread, since it determines the degree of impairment of respiratory function and gas exchange, as well as the severity of clinical manifestations. There are relatively favorable types of fibrotic changes and unfavorable ones. pulmonary hypertension quickly develop , which ultimately leads to a deterioration in the patient’s quality of life and a shortening of its duration.
Classification
According to prevalence and X-ray or CT signs:
- Local pulmonary fibrosis (limited). Local pulmonary fibrosis affects only part of the lung tissue, which becomes denser. The pictures clearly define the boundaries of the pathological process. Limited pulmonary fibrosis does not affect the elasticity of the entire lung and has almost no effect on respiratory function. It is asymptomatic and often does not bother patients. An example of limited fibrosis would be the outcome of macrofocal pneumonia. In chronic bronchiolitis, X-ray examination reveals, in addition to local pneumosclerosis , thickenings around the bronchi. With this disease, bilateral fibrotic changes in the lower sections are usually found.
- Diffuse. With this option, fibrosis diffusely covers the entire lung tissue and the spread of the process occurs much faster than with the local form. The lung tissue becomes denser, the structure is deformed and the volume of the lungs decreases. In this regard, respiratory function deteriorates significantly.
- Focal pulmonary fibrosis is the presence of several foci of different sizes and structures. They can be either limited (rounded) or diffuse (blurred, without clear boundaries). Focal pneumofibrosis is detected in silicosis, pneumoconiosis, at the location of granulomas of various origins.
- Linear pulmonary fibrosis. In what pathology does it occur and what does “linear pulmonary fibrosis” mean? This term is used to describe an X-ray examination or CT scan of the lungs if a tissue compaction is detected in the form of a cord of a linear shape (practically it is a scar that has a linear shape). This type of fibrosis forms after inflammatory diseases (primarily tuberculosis ), injuries, and surgical interventions. Linear pathology often appears on x-ray only several years after the illness. An area of linear fibrosis, which is associated with the root of the lungs, indicates a history of hilar pneumonia or a primary tuberculosis complex. In the chronic form of exogenous alveolitis, CT manifestations are: cellular and rough linear fibrosis. In idiopathic fibrosis, parenchymal damage is symmetrical, and depending on the stage, linear fibrosis, ground glass, bronchiectasis and honeycomb lung are very often observed.
- Peribronchovascular fibrosis is the presence of connective tissue along the bronchovascular bundle. At the same time, the lumen of the bronchi and blood vessels narrows, which causes ventilation and vascular disorders.
- Acinar (intralobular) - the process reflects the filling of acini and terminal bronchioles with connective tissue cells. With this form, pronounced perfusion-diffusion disorders are noted. This is how interstitial pneumonia appears on CT.
- “Honeycomb lung” is a complete loss of the normal structure of the lung. In the lung tissue there is an alternation of fields of fibrosis, emphysema and cysts, which resembles a honeycomb.
With the flow:
- Progressive.
- Not progressive.
Idiopathic pulmonary fibrosis is a special form/variant of chronic fibrosing interstitial pneumonia of unknown etiology, which steadily progresses and is a cause of mortality. It occurs predominantly in older people and affects only the lungs. The process is more often localized in the peripheral parts of the lungs and is manifested by interstitial inflammation of the alveoli with the formation of fibrosis around the alveolar ducts.
As mentioned above, the causes of the disease are unknown, but there are factors that aggravate idiopathic pulmonary fibrosis - smoking, inhalation of inorganic and organic dust, viral infection, diabetes mellitus . The disease most often occurs in patients over 50 years of age. The incidence of the disease increases with age and predominates after 60–70 years.
List of sources
- Ivanova A. S. Fibrosing processes / A. S. Ivanova, E. A. Yuryeva, V. V. Dlin. M.: Overlay, 2008. 196 p.
- Idiopathic fibrosing alveolitis / M. M. Ilkovich [et al.] // In the book: Disseminated lung diseases / Ed. M. M. Ilkovich. M.: GEOTAR-Media, 2011. pp. 24–84. 3.
- Avdeev SN. Idiopathic pulmonary fibrosis: modern approaches to therapy. Practical Pulmonology 2015;1 22–31.
- Tsvetkova O.A., Voronkova O.O. Modern approach to the treatment of patients with idiopathic pulmonary fibrosis. Clinical Med 2017;95:281–5. 31.
- Aisanov Z.R., Kokosov A.N., Ovcharenko S.I., Khmelkova N.G., Tsoi A.N., Chuchalin A.G., Shmelev E.I. Chronic lung diseases. Federal program. RMJ, 2001; No. 1: p. 9 – 33.
Pathogenesis
The final sections of the respiratory tract consist of bronchioles (terminal and respiratory), acini and lobules. Terminal bronchioles are air-conducting, and respiratory bronchioles are involved in gas exchange, since they are connected to the alveoli through pores. The acini is the structure of the lung where gas exchange occurs and includes several respiratory bronchioles. The acini (from 3 to 24) are united into pulmonary lobules. The framework of the lobule includes interlobular septa, periarterial, peribronchial connective tissue, connective tissue of the alveolar and acini septa.
Connective tissue consists of collagen, reticular and elastin fibers. Interweavings of collagen and elastin fibers are present around the bronchi and in the alveolar walls, which determines the elastic properties of the lungs. Collagen provides rigidity to the intrapulmonary framework.
Connective tissue cells (smooth muscle and fibroblasts) synthesize elastin and collagen. Its primary role is to maintain the tone of the terminal sections of the respiratory tract. At the same time, connective tissue cells also synthesize enzymes (proteases) responsible for the destruction of elastin and collagen . The enzyme and antienzyme systems are in equilibrium under normal conditions. Under conditions of infectious inflammation, they continue to have an elastolytic (destructive) effect due to the high production of elastase (an enzyme that destroys elastic fibers, elastin, collagen). This causes the destruction of the normal connective tissue matrix, the destruction of the alveolar walls and the formation of common cavities. Excessive production of elastase or the absence of enzymes for its destruction is observed in a number of lung diseases ( COPD , emphysema , cystic fibrosis ).
In parallel, during inflammatory processes, there is an activation of fibroblasts that produce collagen. As a result, there is an enhanced process of development of connective tissue in the lung parenchyma and the formation of fibrosis. The development of fibrotic changes is preceded by edema and infiltration of the lung tissue. When the alveolar membrane is destroyed, intra-alveolar fibrosis develops at this site - growths of connective tissue spread into the alveoli. Then the connective tissue around the arteries and bronchi is involved in the pathological process.
Currently, a more acceptable theory of the pathogenesis of silicosis and other pneumoconioses is the immunological one, which states that the development of these occupational diseases is impossible without phagocytosis of dust particles by alveolar macrophages. The rate of their death depends on the fibrogenic aggressiveness of the dust and is proportional to it. The death of alveolar macrophages is a mandatory step in the formation of a silicotic nodule. The formation of a nodule is possible under the condition of repeated phagocytosis of dust. The resulting pro-inflammatory mediators ( cytokines ) provoke the accumulation of inflammatory cells in the septa of the alveoli, and oxygen radicals, damaging lung tissue, cause the death of macrophages.
Proteolytic enzymes (metalloproteinase and elastase) are released from destroyed macrophages and destroy lung tissue. The inflammatory phase is accompanied by recovery processes in which growth factors stimulate the formation of cells, epithelium and new vessels in damaged tissues. Uncontrolled epithelization processes lead to the development of fibrosis. Growth factors play one of the key roles in fibrogenesis . Their stimulating effect on the proliferation of fibroblasts and the destruction of collagen and fibronectin (high molecular weight protein of connective tissue) has been proven. In idiopathic fibrosis, fibrosis predominates with mild inflammatory changes. The main mechanism for the progression of pneumofibrosis is constant damage to the alveolar epithelium with impaired regeneration and excessive deposition of connective tissue due to the activation of fibroblasts.