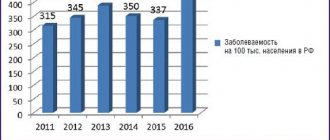
According to statistics, bacterial pneumonia affects an average of about 1000 patients per 100 thousand population. This form of the disease occurs especially often in older people, over 75 years of age, or those who suffer from chronic pathologies. ALENA PARETSKAYA
Pathophysiologist,immunologist, WHO expertELENA ZARYANOVACandidate of Medical Sciences, pulmonologist of the highest category,somnologist "SM-Clinic"
Bacterial pneumonia is a common complication in patients treated in hospitals and clinics. In recent years, there has been an increase in severe forms that lead to death.
Causes of bacterial pneumonia in adults
Bacterial pneumonia is most often caused by bacteria, which are considered part of the microflora of the respiratory tract.
These microorganisms belong to the category of opportunistic pathogens. If the body is healthy, not weakened, the immune system is working properly, bacteria do not harm in any way. But during stress, operations, exacerbation of chronic diseases, severe acute respiratory viral infections, bacteria can become dangerous. There are two types of bacterial pneumonia - community-acquired and nosocomial. They vary greatly in the type of bacteria that causes inflammation.
In community-acquired pneumonia, the inflammatory process is usually provoked by pneumococcus, Haemophilus influenzae or streptococcus.
Nosocomial pneumonia is caused by particularly aggressive bacteria that are resistant to many antibiotics. These pathogens usually live in clinics - Staphylococcus aureus, Pseudomonas aeruginosa, Enterobacteriaceae and some others. Often such pneumonia occurs in people who undergo mechanical ventilation.
If patients suffer from immunodeficiency, pneumonia can be caused by Legionella, Mycoplasma, Pneumococcus, Haemophilus influenzae and Pneumocystis.
Bacteria penetrate into the lungs from the air, with the blood flow from inflammatory foci in the body or with the lymph flow, directly, with chest wounds. Risk factors that increase the likelihood of pneumonia are:
- frequent ARVI and influenza;
- bad habits (they weaken the immune system);
- constant stress and overwork;
- deficiency of vitamins and minerals;
- age over 65 - 70 years;
- living in areas with air pollution.
Pneumonia is likely in people with COPD, heart problems, diabetics, against the background of sinusitis, after operations and injuries.
Expert opinion
More than 1 million cases of pneumonia are diagnosed annually on our planet.
Moreover, almost 8.5% of them are fatal. Of course, the vast majority of such adverse outcomes occur in groups at risk for pneumonia: children under 5 years of age and elderly people over 65 years of age. However, even if you are young and healthy, neglecting pneumonia is extremely dangerous. At the first manifestations of this disease, you should immediately consult a doctor and under no circumstances self-medicate. Pulmonologists at SM-Clinic will make a diagnosis as quickly as possible, determine what exactly caused pneumonia and prescribe the necessary therapy. It will include modern highly effective drugs and techniques, and will be built in accordance with the clinical recommendations of the Russian Respiratory Society and the Interregional Association for Clinical Microbiology and Antimicrobial Chemotherapy, approved by the Ministry of Health of the Russian Federation and WHO recommendations.
Savina Maria Yuryevna, pulmonologist at SM-Clinic in Ryazan
Symptoms of bacterial pneumonia in adults
In many ways, the symptoms of pneumonia depend on what bacteria is causing them. The more aggressive the microbe, the more severe the manifestations. The most typical manifestations of bacterial pneumonia:
- a sharp increase in temperature, which is poorly controlled by antipyretic drugs;
- severe sweating, chills;
- a cough that is wet from the first days, with copious sputum (has a greenish or rusty color);
- chest pain, especially when breathing deeply;
- severe weakness with malaise;
- headache, aches in muscles and joints;
- pale, sallow skin color;
- low blood pressure, rapid pulse;
- frequent breathing, shortness of breath, wheezing when breathing.
If pneumonia is not treated, respiratory and heart failure, toxicosis and even death can develop. It is extremely rare to have atypical bacterial pneumonia, which has very few symptoms, they are mild, but the lungs are affected to a significant extent.
List of scientific literature used:
- Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. International Journal of Antimicrobial Agents. March, 2020, 55 (3): 105924.
- Marchello CS, Ebell MH, Dale AP, Harvill ET, Shen Y., Whalen CC Signs and Symptoms That Rule out Community-Acquired Pneumonia in Outpatient Adults: A Systematic Review and Meta-Analysis.” Journal of the American Board of Family Medicine. April, 2022, 32 (2): 234–247.
- Metlay JP, Waterer GW, Long AC, Anzueto A, Brozek J, Crothers K, et al. Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. American Journal of Respiratory and Critical Care Medicine. October, 2022, 200(7): e45–e67.
- Pneumonia. Mayo Clinic Staff. Patient Care & Health Information. Mayo Clinic. Last reviewed: August, 2, 2022.
- Who Is at Risk for Pneumonia? US Department of Health & Human Services. The National Heart, Lung, and Blood Institute. Last reviewed: March 3, 2016.
- Pneumonia. News bulletin. World Health Organization. July 25, 2022.
- Chuchalin A.G., Sinopalnikov A.I., Kozlov R.S., Avdeev S.N., Tyurin I.E., Rudnov V.A., Rachina S.A., Fesenko O.V. Russian Respiratory Society (RRO). Interregional Association for Clinical Microbiology and Antimicrobial Chemotherapy (IACMAC). Clinical guidelines for the diagnosis, treatment and prevention of severe community-acquired pneumonia in adults. Pulmonology. 2014, (4): 13-48.
Diagnostics
The doctor focuses on the patient’s complaints and the data that he sees and hears. If the doctor listens to the chest with a phonendoscope, he will hear typical wheezing, changes in breathing and so-called crepitus (the noise of a lung affected by inflammation). Bacterial pneumonia can be confirmed by:
- blood tests indicating severe inflammation (leukocytosis, changes in protein levels, clotting);
- X-ray of the chest with areas of darkness where the lung is affected;
- CT scan of the lungs, if the diagnosis is not clear on a regular x-ray;
- culture of sputum for flora with identification of a specific bacteria (or several) and determination of sensitivity to antibiotics;
- saturation (oxygen saturation in the blood) less than 95%.
Additionally, if the case is complex, the doctor may order other tests.
Prevention
Vaccination against influenza and flu helps reduce the risk of infection. Preventive measures are strongly recommended for people at risk:
- Anyone should receive further treatment. The choice of drugs, especially potent ones, is determined by the doctor.
- Avoiding contact with people with acute respiratory infections will help reduce the risk of infection.
- Nutrition should be complete. During periods of exacerbation of colds, it is strongly recommended to include more fruits and vegetables in the diet and start taking multivitamins.
- To protect yourself from hypothermia and getting wet, and to reduce the body’s reaction to temperature changes, hardening and using a contrast shower will help.
- Exercise and breathing exercises promote healthy lung function.
- A living or work space in which a lot of time is spent requires regular wet cleaning and ventilation.
Failure to comply with the work and rest regime greatly depletes the body physically and mentally. The appearance of colds cannot be ignored, much less endured on your feet; in case of complications, treating the consequences will be much more difficult.
Modern methods of treatment
Bacterial pneumonia in mild and moderate cases can be treated at home, under the supervision of a doctor.
In severe forms - in the clinic, intensive care ward and resuscitation room. Bed rest, a light diet, and plenty of fluid intake (or intravenous administration) are indicated. The main treatment is antibiotics: the doctor selects them based on test data. Most often, penicillins, cephalosporins or macrolides are used. If these are separate forms of pneumonia, more narrowly targeted drugs are selected. Medicines are taken orally or by intramuscular injection for up to 14 days; in severe cases they are administered intravenously.
Treatment is complemented by:
- antipyretic drugs, anti-inflammatory drugs (Nurofen, Nise, Ibuklin, Rinza, Panadol);
- short course hormonal drugs;
- droppers with protein, saline solutions, vitamins and glucose;
- oxygen therapy;
- drugs for coughing up sputum (Bromhexine, ACC, Ambroxol, Fluimucil).
As the condition improves, the doctor adds breathing exercises, massages, physiotherapy, exercise therapy and subsequent rehabilitation in a sanatorium to the treatment.
Classification
- Community-acquired pneumonia is the most common type of disease.
- Nosocomial or hospital-acquired pneumonia. This form includes a disease that developed while the patient was in the hospital for more than 72 hours.
- Atypical pneumonia. A type of disease caused by atypical microflora (chlamydia, mycoplasma, legionella, etc.).
- Aspiration pneumonia is an infectious-toxic damage to the pulmonary parenchyma that develops as a result of the contents of the oral cavity, nasopharynx, and stomach entering the lower respiratory tract.
Depending on the etiology, pneumonia can be:
- viral;
- fungal;
- bacterial;
- mycoplasma;
- mixed.
Depending on the nature of the disease:
- acute;
- acute protracted;
- chronic;
- atypical.
Type of pneumonia by location
- left-handed;
- right-sided;
- unilateral: one lung is affected;
- bilateral: both lungs are affected;
Severity of the inflammatory process:
- light;
- moderate severity;
- heavy.
How not to miss the onset of the disease: the first signs
With the development of inflammatory processes in the lungs, the majority of patients (more than 40%) develop a fever. In the first 1-2 days it may not rise to high levels and remain at 37-37.3°. As bacterial colonies grow, the temperature increases, the patient's general condition worsens, and symptoms of intoxication appear. The temperature at this stage can reach 38.5-39° and is usually accompanied by the following symptoms:
- chills;
- lethargy;
- deterioration (or complete absence) of appetite;
- fever;
- headache;
- drowsiness.
Classification of pneumonia
The second symptom of pneumonia that appears at an early stage is cough. In the first days of the disease, it is hysterical, dry, and painful. There is no sputum production during this period. Cough torments the patient at any time of the day, intensifies at night, disrupting the quality of sleep. In some cases, it may be accompanied by shortness of breath, but such symptoms are usually typical for 3-4 days of illness.