COVID-19✓ Safe
Pneumofibrosis affects both men and women and begins as a result of various inflammations or degenerative processes.
Since many of you have already encountered this term when reading computed tomography of the lungs, doctors’ reports and from the media.
Today, a massive examination of the respiratory system using CT (computed tomography) is being carried out as a necessary measure to diagnose lung damage caused by the COVID-19 virus, which has never been carried out.
And therefore, many patients have questions: “Is this scary?”, “Nothing hurts me,” “What to do about it?”, “Why treat?” and so on.
This study allows us, doctors, to immediately navigate the diagnosis and tactics of patient management, determine the need for emergency or planned treatment, additional examination, and rehabilitation.
And therefore, you should not neglect the results and recommendations, especially if it concerns planned activities, namely rehabilitation after pneumonia.
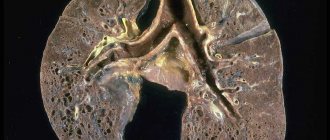
So, Pneumofibrosis is a disease due to which the lung tissue is replaced with connective tissue. Belongs to the group of pneumosclerotic pathologies. This disease rarely occurs on its own, more often against the background of existing ailments in the human body. It affects both men and women and begins as a result of various inflammations or degenerative processes.
Causes of pneumofibrosis
Often, pneumofibrosis occurs as a result of hypoxia of the lung tissue, which leads to the activation of fibroblasts that produce collagen, which becomes the initial stage of connective tissue development.
It is also possible to identify the main reasons that provoke pathological processes in the lungs: disruption of the process of ventilation of the lungs, the outflow of secretions from the bronchi and blood and lymph drainage.
Normally, lung tissue is elastic, which ensures the normal functioning of the body's respiratory system. The greater the elasticity, the more the body puts effort into stretching the tissue, which leads to high intrapulmonary pressure. The pressure inside the lungs acts on the inner wall of the alveoli and opens it when air is inhaled. When pulmonary fibrosis begins, most of the alveoli are affected, as a result, the elasticity in the lungs decreases, and the body requires less force to stretch. In this case, low intrapulmonary pressure does not open all the alveoli and some of them fall out of the general respiratory system, which is why the body receives less oxygen and the ventilation process of the lungs is disrupted.
Inflammatory processes in the bronchi disrupt the outflow of secretions that accumulate in them, which becomes a favorable environment for the proliferation of pathogenic microflora.
Disruption of blood and lymph flow occurs due to compression of blood vessels in the lungs, stagnant processes in the vessels adjacent to the lung. Blood stagnation usually occurs due to inflammatory processes and spasms. At the site of stagnation, connective tissue begins to form, which over time replaces the adjacent alveoli.
In other words, the development of pulmonary fibrosis is influenced primarily by the primary disease in the lungs (focus of inflammation), which provokes the replacement of lung tissue with connective tissue.
In each case, depending on the factor that provoked the pathological process, the connective tissue develops differently: in case of impaired ventilation of the lungs, the appearance of connective tissue in the lungs becomes the root cause of pneumofibrosis, in stagnant processes it is a consequence.
As the disease progresses, the lung tissue falls out of the respiratory system, which leads to the development of respiratory failure and disruption of gas exchange processes between vessels, tissues, and alveoli.
Medicines
- Bronchodilators: Atrovent , Ipratropium-native , Ipratropium Air , Spiriva , Tiotropium-native , Ultibro Breezhaler .
- Mucolytics: Acetylcysteine , Eucabal , Bronchomucin , Fluditec , Ambrol , Ermucin , Lazolvan .
- Glucocorticoids: Prednisolone .
- Antitumor drugs (cystatics): Cyclophosphamide .
Symptoms of pneumofibrosis
- Apathy
- Chest pain
- Fast fatiguability
- Cough
- Dyspnea
- Changes in body temperature
- Weight loss
- Enlarged veins in the neck
- Whistling sound in the lungs
- Blueness of the skin
- Weakness
- Dry cough
Pneumofibrosis manifests itself locally or diffusely. Most often, a diffuse form of the disease is detected, since local lesions of the lung tissue usually do not have pronounced symptoms.
The main symptom indicating a pathological process is shortness of breath, which in the initial stages occurs due to physical fatigue. And then it begins to bother me even in a calm state.
Often a person begins to be bothered by a severe cough, during which viscous sputum, sometimes with purulent impurities, is released from the bronchi. A visual examination can identify signs of cyanosis, which develops due to pulmonary hypoxia.
Often there is aching pain in the chest, weakness, and a person may lose weight for no reason.
With severe lesions, coughing causes pain in the chest.
In advanced stages, wheezing or “the sound of a plug rubbing” can be heard in the lungs.
If complications occur, blood may be produced when you cough and sputum.
In addition to the symptoms of pulmonary fibrosis, there are signs of the primary disease that provoked the pathology.
Pulmonary fibrosis after coronavirus
Pulmonary fibrosis after Covid is one of the complications that occurs after the virus. Penetrating into the body, it causes severe inflammation, which is why the immune system uses every opportunity to destroy the virus. However, this response triggers the release of inflammatory cytokines. It is the activity of these elements that makes it possible to determine the extent of lung damage. As part of the coronavirus, the alveoli and pulmonary vessels are affected.
After suffering from the virus, the lungs become less elastic, the damaged tissue is replaced by scar tissue and fibrosis forms. Despite the fact that the inflammation has been eliminated, breathing difficulties continue. If left untreated, fibrosis can progress.
With pulmonary fibrosis after coronavirus, the patient may complain of:
- Shortness of breath that appears even when talking.
- Headaches and dizziness.
- Dry cough.
- Weakness and feeling of fatigue.
- Low level of endurance and performance.
Diagnosis of pneumofibrosis
Pneumofibrosis is diagnosed based on symptoms and a thorough medical examination.
If pulmonary fibrosis is suspected, the patient is referred for consultation to a pulmonologist.
The main diagnostic tool for this pathology is x-ray, which will help establish the sclerotic nature of changes in lung tissue and distinguish pulmonary fibrosis from a tumor in the lungs.
If necessary, the doctor may prescribe a computed tomography, tomography, or radiography.
Procedures and operations
During any exercise, the heart and lungs work actively. Special breathing exercises are aimed at increasing the functionality of the lungs, reducing shortness of breath and increasing exercise tolerance. The complex should include exercises for training diaphragmatic breathing and exercises with forced exhalation. You can take breathing exercises according to the method of P. A. Buteyko as a basis. The duration of breathing exercises is 10 minutes, and you need to perform it 3-5 times during the day. The ideal option is individually selected gymnastics. If the condition of the respiratory system allows, you can engage in race walking.
Among the procedures, oxygen replacement therapy is indicated, which is carried out when the blood oxygen pressure decreases to less than 60 mm Hg. Art. In case of chronic respiratory failure, oxygen therapy is carried out at home for a long time (18 hours a day) in a low-flow (2-5 l/min) oxygen supply mode. In case of severe respiratory failure, helium-oxygen mixtures are used. Oxygen concentrators are used at home.
To remove circulating immune complexes from the blood (especially in bronchial asthma ), hemosorption .
Treatment of pneumofibrosis
If local lesions in the lungs are identified after inflammatory or destructive processes, or pneumofibrosis develops against the background of regularly occurring infectious processes, then the pulmonologist prescribes antibacterial therapy, anti-inflammatory drugs, as well as physiotherapeutic procedures that improve sputum discharge.
In our center, we have developed unique rehabilitation programs after pneumonia for the early prevention and treatment of pulmonary fibrosis.
These programs are compiled using modern placental preparations made in Russia and Japan.
Various options for rehabilitation programs have been developed, taking into account individual characteristics, the severity of residual effects, and concomitant diseases.
Therapy - if indicated
— Which patient can and should suspect that he or she has pulmonary fibrosis?
NK: It depends on the focus of the pulmonary lesion. A small focus of pneumofibrosis, of course, does not manifest itself clinically. If this is a more extensive damage to the lung tissue (from 25%), then a decrease in exercise tolerance, the development of shortness of breath, cough, and a decrease in oxygen saturation in the blood are possible. Then, of course, you can suspect a problem and perform a CT scan to confirm the diagnosis.
MK: When you stop at every flight of stairs while walking or climbing stairs, you feel like you’re not getting enough air
— At what stage is it better to use therapy against pulmonary fibrosis?
NK: If indicated. If, after studying pulmonary function, performing a CT scan, and excluding a predisposition to thrombus formation, there are indications that therapy is necessary, of course, it is carried out.
MK: Criteria for assessing the severity and damage to the bronchopulmonary system must be developed. And a single step-by-step approach, because after the examination some patients will be treated on an outpatient basis, some in a hospital, and some in a mixed manner.
There must be specific prevention of the release of hyaluronic acid into the bronchopulmonary apparatus. Drugs are prescribed that can inhibit its further release, so that new painful areas do not form in the lungs. And there are such drugs in Russia.
Studies have shown that the administration of an antifibrotic drug (for example, bovhyaluronidase azoximer) has an inhibitory effect, preventing the disease from spreading towards severe pulmonary fibrosis. This drug is prescribed for both the treatment and prevention of pulmonary fibrosis.
I am sure that in the next six months new Russian recommendations will appear that will show what methods and drugs can and should be prescribed for pulmonary fibrosis with a risk of its development. But while new techniques are being developed, we will not be able to abandon the patients: we will use what we know, which can have an impact on the restoration of lung tissue.
Prevention of pulmonary fibrosis
Pneumofibrosis often develops against the background of infectious and inflammatory diseases in the lungs, when inhaling toxic substances and polluted air (dust).
To prevent the disease, you should completely stop smoking, lead an active lifestyle, and promptly identify and treat diseases.
If your line of work requires you to work with toxic substances, dust and other pollutants, you must adhere to safety precautions and use respirators.
Classification of IBL
Currently, the classification developed in 2002 by the American Thoracic Society (ATS) and the European Respiratory Society (ERS) is adopted as the basis. According to this classification, there are interstitial lung diseases. With established etiology:
- Radiation, medicinal, toxic;
- Pneumomycoses associated with HIV infections
- Interstitial lung diseases against the background of collagenosis and pneumoconiosis;
- Interstitial lung diseases due to infections;
- Interstitial lung diseases against the background of allergic alveolitis.
Idiopathic interstitial pneumonia:
- Nonspecific, lymphoid, acute, desquamative, cryptogenic organizing;
- Idiopathic pulmonary fibrosis.
- Granulomatous: interstitial diseases against the background of sarcoidosis, exogenous allergic alveolitis, hemosiderosis.
Associated with other diseases:
- Pathology of the liver, intestines, kidneys;
- Hereditary diseases;
- Malignant neoplasms.
Other: associated with primary pulmonary amyloidosis, pulmonary proteinosis.
Pathologists distinguish the following types of fibrosis in interstitial lung diseases:
- Simple;
- Desquamative;
- Lymphocytic;
- Bronchiolitis obliterans with pneumonia;
- Giant cell.
Make an appointment
Prognosis of pneumofibrosis
Pneumofibrosis is always a consequence of the underlying disease and the prognosis in this case depends on the severity and complexity of the initial disease. With significant damage to the lung tissue, a decrease in lung volume occurs, which leads to respiratory failure and increased pressure in the pulmonary artery. Death, as a rule, occurs as a result of a new infection or the onset of the tuberculosis process.
Pneumofibrosis disrupts the structure and function of the lungs. Over time, the pathology leads to deformation of the bronchi, a decrease in volume and shrinkage of the lungs. All age categories are susceptible to the disease; most often, pneumofibrosis is diagnosed in men.
Not just the lungs
— Why is pulmonary fibrosis dangerous?
MK: The trouble is that not only the lungs suffer from lung disease. It is known that when oxygen supply is limited, if gas exchange does not occur, complications in the functioning of the cardiovascular and nervous systems subsequently arise. The heart begins to work harder: deformation appears, various pathologies are formed throughout the cardiovascular system, since lung damage does not occur separately from vascular damage. And then - increased pressure with possible hypertension, and blood clots may also break off.
Then a nervous rollback begins, because depression develops from a lack of oxygen, and people simply lose the desire to live. Memory fails: a person may be asked to leave work because labor productivity is falling. If left untreated, this condition may not be limited to 6 months or a year, but will persist forever.
The process of rehabilitation of such patients is a new direction, we must now develop and develop it. Psychologists, cardiologists, neurologists, and endocrinologists will have to work here.