When the frequency of the disease in the region of surveys conducted among children of primary and secondary school age exceeds 5%, goiter is considered endemic. Diffuse euthyroid goiter is a pathology of the young part of the population and it develops before the age of 20 in more than 50% of cases, while affecting women 2-3 times more often than men, especially during periods of increased body need for iodine - during puberty , bearing a child and breastfeeding him.
Diffuse nontoxic goiter predominantly develops against the background of iodine deficiency, when the thyroid gland undergoes compensatory hyperplasia to compensate for the deficiency of thyroid hormones.
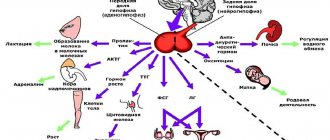
The growth of thyroid tissue is directly influenced by autocrine factors that stimulate thyrocytes: fibroblast, epidermal and transforming growth factors.
In addition to an insufficient amount of iodine in the diet, DEZ is provoked by taking specific medications, smoking tobacco, the presence of a long-term stressful condition and an infectious disease, poor nutrition with a deficiency of vital microelements responsible for iodine metabolism, as well as congenital defects of certain enzymes, age, gender and predisposition to the disease patient.
Treatment of thyroiditis
Mild subacute thyroiditis goes away on its own within 2-6 months. The fundamental principle of treatment is symptomatic therapy - that is, the elimination of external manifestations that cause discomfort to the patient. The drugs of choice are glucocorticoids and non-steroidal anti-inflammatory drugs. In the case of transient hypothyroidism and subacute thyroiditis, HRT is indicated.
The attending physician is faced with the task of reducing pain, relieving symptoms, as well as preventing possible relapses of the disease.
Reasons for development
Euthyroidism can be considered one of the most insidious diseases of the thyroid gland. It cannot be diagnosed immediately, hormone levels are always normal, and more dangerous diseases have already begun to develop.
The main causes of thyroid euthyroidism include the following:
- processes in the body associated with improper functioning of the immune system;
- unfavorable environment;
- heredity;
- thyroid diseases associated with the inflammatory process.
Prognosis for thyroiditis
The prognosis for thyroiditis depends on the severity of the pathology, the accuracy of diagnosis and timely treatment. Advanced cases, with goiter of large and enormous sizes, are now practically never encountered due to the availability of diagnostic and treatment methods. Most patients with acute, subacute and autoimmune thyroiditis (Hashimoto's disease) have a favorable prognosis.
With Riedel's thyroiditis, the prognosis depends on the success of treatment and the presence of damage to other organs. Deaths in patients receiving treatment are extremely rare.
Diet and other aspects of nutrition
If it has been established that the cause of euthyroidism is hidden in iodine deficiency, then you can try to cope with the problem with the help of diet.
The menu should include products such as:
- Sea fish: hake, pollock, haddock, capelin, cod.
- Shrimps.
- Squid.
- Feijoa.
- Sea kale.
- Persimmon.
- Liver.
- Spinach.
- Eggs.
Most iodine can be obtained from fish, algae and seafood.
When a person develops obesity against the background of euthyroidism, it is necessary to adjust the diet so that it contributes to weight loss.
The following foods and drinks are excluded from the menu:
- Flour dishes.
- Fatty food.
- Smoked meats.
- Fast food.
- Alcohol.
- Confectionery and other sweets.
A person should eat food that is a source of fiber. Salads should be prepared from fresh vegetables. Be sure to supplement the diet with bran, cereals, and nuts. Among the cereals, oatmeal and buckwheat are considered especially healthy.
Autoimmune thyroiditis - symptoms and treatment
Therapy for autoimmune thyroiditis of the thyroid gland is nonspecific. When the phase of thyrotoxicosis develops, the use of symptomatic therapy is sufficient. When hypothyroidism develops, the main option for drug therapy is the administration of thyroid hormones. Now in the pharmacy chain of the Russian Federation it is possible to purchase only Levothyroxine sodium tablets (L-thyroxine and Euthyrox). The use of tableted preparations of thyroid hormones neutralizes the clinical picture of hypothyroidism and, in the hypertrophic form of autoimmune thyroiditis, causes a decrease in the volume of the thyroid gland to acceptable values.
If a patient has manifest hypothyroidism (an increase in the level of thyroid-stimulating hormone and a decrease in the concentration of free T4), it is necessary to use levothyroxine sodium in the treatment at an average dose of 1.6 - 1.8 mcg/kg of the patient’s body weight. An indicator of the correctness of the prescribed treatment will be the confident retention of thyroid-stimulating hormone in the patient’s blood within the reference values.
When a patient is diagnosed with subclinical hypothyroidism (increased TSH concentration in combination with unchanged free T4 concentration), it is necessary:
- After 3–6 months, carry out a second hormonal examination to confirm the presence of changes in thyroid function;
- When an increase in thyroid-stimulating hormone levels is detected in a patient during pregnancy, even with preserved free T4 concentrations, prescribe levothyroxine sodium at the full calculated replacement dose immediately;
- Treatment with levothyroxine sodium is necessary for persistent subclinical hypothyroidism (an increase in the concentration of thyroid-stimulating hormone in the blood above 10 mU/l, and also in situations of at least twice the determination of the concentration of thyroid-stimulating hormone between 5 - 10 mU/l), but if these patients are over 55 years old and have they have cardiovascular pathologies, treatment with sodium levothyroxine is prescribed only if the drug is well tolerated and in the absence of information about decompensation of these diseases while taking thyroxine;
- An indicator of the sufficiency of treatment for subclinical hypothyroidism is the stable maintenance of TSH levels within the reference values in the blood.
If women, before planning pregnancy, have antibodies to thyroid tissue and/or ultrasound signs of autoimmune thyroiditis, it is necessary to determine the hormonal function of the thyroid gland (thyroid-stimulating hormone concentration and free T4 concentration) and be sure to determine the level of hormones in each trimester of pregnancy.[8]
If autoimmune thyroiditis is diagnosed, but changes in the functioning of the thyroid gland are not detected, the use of sodium levothyroxine is not indicated.[9] It is sometimes possible in exceptional situations of an impressive increase in the volume of the thyroid gland, provoked by autoimmune thyroiditis, and the decision is made for each patient individually.[10]
Physiological amounts of potassium iodite (approximately 200 mcg/day) cannot provoke the formation of hypothyroidism and do not have a negative effect on thyroid function in previously developed hypothyroidism caused by autoimmune thyroiditis.
Nutrition for autoimmune thyroiditis
There are no products that affect the course of autoimmune thyroiditis. Gluten or lactose are not related to hypothyroidism due to AIT. Therefore, dietary recommendations for people with autoimmune thyroiditis are the same as for everyone else: a varied, balanced diet with sufficient water intake.
Are there traditional methods of treatment?
Autoimmune thyroiditis is treated only with medications prescribed by an endocrinologist. The lack of adequate therapy can lead to dangerous complications: impaired reproductive function, severe memory loss (even dementia), anemia and coma, which occurs with a severe deficiency of thyroid hormones.
Symptoms
Autoimmune thyroiditis itself does not pose a risk to the body’s vital functions. Complications can be dangerous if treatment is completely missed. Since hypothyroidism is considered the main consequence of AIT, the symptoms of the disease are similar to its development.
Note! The first three stages may not have pronounced external symptoms. The clinical picture is determined mainly during a diagnostic examination.
The following symptoms are characteristic of autoimmune thyroiditis:
- apathy and depression (occurs in people exposed to emotional influence);
- memory impairment (a person may forget some events, but not of significant importance);
- absent-mindedness (the patient is unable to concentrate his attention on something specific for a long time);
- general impotence accompanied by drowsiness;
- loss of desire to eat (leads to weight loss, in rare cases it goes into a critical phase);
- problems with heart rhythm (expressed as slowing of the heart muscles);
- periodic feeling of chilliness in both the upper and lower extremities;
- decreased capacity for physical activity (associated with general weakening of the body);
- reactions are inhibited (slowdown even applies to reflex reactions);
- decreased sexual desire (changes in hormonal levels affect libido);
- the condition of the nail plates, hair and skin worsens (deviation is observed due to general disorders);
- menstrual irregularities (expressed in disruptions of menstruation and changes in the nature of discharge);
- swelling in the face (patients experience abnormalities in the functioning of the kidneys and urinary system, which leads to the accumulation of fluid in the body);
- disturbance of facial expressions (characterized by inflammation of neuromuscular tissues);
During the development of the disease, the symptoms of the inflammatory process can change from an active phase to a subside.
In the last fourth stage, the patient may exhibit signs of:
- a sharp decrease in body weight;
- periodic hot flashes;
- increased sweating;
- deterioration of general condition in stuffy rooms;
- tremor of fingers;
- sudden and unexplained mood changes;
- increased heart rate;
- periodic attacks of arterial hypertension;
- inexplicable bouts of activity followed by impotence.
These signs complement the general symptoms.
If we consider the symptoms according to the forms of the disease, experts note that postpartum autoimmune thyroiditis appears in the fourth month after the birth of the child, and the last stage can occur as early as two months.
The chronic form is characterized by the appearance of symptoms only during exacerbations, while the cytokine-induced and asymptomatic form is often detected by chance, since signs of the disease practically do not appear.
Euthyroidism – what is it?
With euthyroidism, the functioning of the thyroid gland is disrupted, but hormone levels remain normal. The patient feels completely healthy, although this is not the case.
When analyzing hormone levels, the indicators are normal, the background of the gland is stable. This condition can persist for a long time, while pathological processes will not develop either. This is the danger, since the situation can change dramatically. This pathology provokes the appearance of nodular goiter, which is in a kind of “lethargic sleep” while the hormonal background is stable.
Medical studies have found that stable hormonal levels do not last long. And as soon as changes occur, the functioning of the thyroid gland worsens. Thyroid diseases are closely related to hormones: a significant decrease provokes hypothyroidism, an increase - hyperthyroidism.
Acute and subacute thyroiditis.
Typically develop after a viral or bacterial infection. Acute thyroiditis can be purulent or non-purulent. Acute purulent thyroiditis develops due to the presence of a focus of chronic infection, after suffering tonsillitis, periodontitis, pneumonia, etc.
The clinical picture begins acutely and is characteristic of the inflammatory process: swelling of the gland (enlargement and pain on palpation), severe pain radiating to the lower jaw, neck, increased body temperature, chills, severe asthenia.
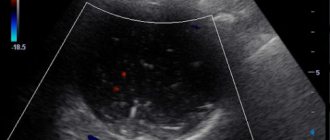
Laboratory examination reveals inflammatory changes in the general blood test (increased leukocyte levels, changes in the leukocyte formula, acceleration of ESR). When examining hormonal status, most often no changes are detected, but a picture of thyrotoxicosis is possible. An ultrasound of the thyroid gland reveals signs of inflammation and increased blood circulation in the gland.
Treatment: rest, antibiotic therapy, anti-inflammatory therapy with NSAIDs, identification and treatment of the source of infection.
Acute non-purulent thyroiditis is the result of trauma, hemorrhage into the gland, irradiation of the head and neck organs (post-radiation thyroiditis). It begins some time after exposure and is less acute. Treatment consists only of NSAIDs and sometimes glucocorticoids.
Subacute thyroiditis (De Quervain's thyroiditis) begins less acutely than acute thyroiditis. The cause is a viral infection. Women get sick more often.
The clinical picture is also characterized by signs of local inflammation, asthenia, pain, chills, fever to subfebrile, sometimes with signs of thyrotoxicosis. If treatment is started in a timely manner, the inflammation goes away quickly and without consequences.
Laboratory changes are characteristic of o.thyroiditis, but less pronounced.
Treatment: anti-inflammatory therapy with NSAIDs or glucocorticoids, symptomatic treatment of manifestations of thyrotoxicosis.
As a result of suffering from thyroiditis, hypothyroidism can develop, therefore, after acute and subacute thyroiditis, it is recommended to observe for 6 months with a study of hormonal status, antibody levels and ultrasound.