Chronic hepatitis is a very common disease: it affects at least 5% of the population of our planet. The concept of chronic hepatitis unites a whole group of liver diseases. They can be caused by different reasons and have different clinical signs, but they last for at least six months without any improvement.
Among the forms of chronic hepatitis are:
- persistent (this is a benign, inactive form);
- chronic active (close to acute hepatitis in its manifestations);
- chronic cholestatic.
Symptoms of chronic hepatitis
In the first case, chronic hepatitis manifests itself weakly, its symptoms are loss of appetite, heaviness and pressure in the right hypochondrium, caused by an increase in the size of the liver and its moderate hardening, and dyspepsia. Chronic active hepatitis is accompanied by a wider range of symptoms: weakness and fatigue; Some foods are not tolerated by patients (for example, fats); dyspepsia, the appearance of spider veins and nosebleeds, which are caused by deterioration of blood clotting; skin itching and increased body temperature, while not only the liver, but also the spleen enlarges. With lupoid hepatitis, as one of the forms of manifestation of chronic active hepatitis, there are furunculosis, lymphadenopathy, hormonal disorders, fever, abdominal pain, etc.
Skin itching, jaundice, lightening of stool and dark urine, soft nodular formations on the skin accompany chronic cholestatic hepatitis.
Hepatitis is an inflammation of the liver. If the inflammatory process lasts less than 6 months, hepatitis is acute; if it lasts more than 6 months, it is chronic.
Hepatitis can be caused by various factors. There are infectious and non-infectious hepatitis. Among infectious diseases, the most common are viral ones, but there are hepatitis caused by bacteria and parasites. Non-infectious ones can be caused by toxic substances, including alcohol, diseases of other organs and systems of the body. Chronic alcoholism is one of the main causes of non-infectious hepatitis: approximately 20% of patients suffering from alcoholism for 5-6 years develop alcoholic liver damage.
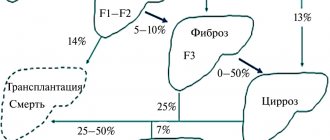
As a rule, acute hepatitis ends in complete recovery. Sometimes the disease becomes chronic, which can last for months or years, and in some cases leads to cirrhosis or liver cancer.
Synonyms Russian
Non-infectious hepatitis, alcoholic hepatitis, non-alcoholic steatohepatitis, fatty hepatosis, drug-induced hepatitis, toxic hepatitis, toxic-allergic hepatitis, idiopathic hepatitis, autoimmune hepatitis, reactive hepatitis, chronic persistent hepatitis, chronic active hepatitis, necrotizing hepatitis, lobular hepatitis, neonatal hepatitis, acute hepatitis, chronic hepatitis.
English synonyms
Acutehepatitis, chronichepatitis, nonviral hepatitis, noninfectious hepatitis, non-alcoholic hepatitis, non-alcoholic steatohepatitis, NASH, toxic hepatitis, autoimmune hepatitis, neonatal hepatitis, d-induced hepatitis, alcoholic hepatitis.
Symptoms
In the initial stages, hepatitis may occur unnoticed. The first signs of the disease are usually nonspecific. The intensity of symptoms depends on the cause of hepatitis, the activity and duration of the pathological process. The main symptoms of hepatitis are:
- weakness, malaise;
- yellowness of the skin, sclera;
- pain in muscles and joints;
- loss of appetite;
- nausea, vomiting, heaviness in the stomach;
- fever.
General information about the disease
The liver is one of the most important human organs. It is located in the upper right part of the abdominal cavity, bordered by the diaphragm, right kidney, intestinal loops, stomach and consists of two main lobes (right and left), which are formed by thousands of lobules. The lobules consist of hepatocytes - cells responsible for performing the main functions of the liver. The liver is supplied by the hepatic artery, which carries oxygen-rich blood, and the portal vein, which carries blood from the gastrointestinal tract. The outflow of blood is carried out through the hepatic vein. There is also a complex system of bile ducts through which the synthesized bile enters the gallbladder, where it accumulates, and into the intestines.
The liver performs a number of vital functions: synthesizes proteins (albumin, coagulation factors), cholesterol, enzymes, hormones, bile, cleanses the blood of excess hormones, metabolic products, toxins and microorganisms that enter the blood through the digestive system, participates in the metabolism of carbohydrates, vitamins, microelements.
Exposure to a number of factors can lead to liver damage and disruption of its function. With hepatitis, the liver tissue becomes inflamed, leukocytes accumulate in it, areas of necrosis (death) may appear, and a small amount of connective fibrous tissue appears. However, in general, unlike cirrhosis, the structure of the liver lobules is not disturbed. Inflammation is accompanied by stagnation of bile and dysfunction of hepatocytes.
Depending on the cause of occurrence, the following types of non-infectious hepatitis are distinguished.
- Alcoholic hepatitis. It is formed as a result of many years of alcohol abuse, which disrupts the metabolism in hepatocytes, leading to their destruction.
- Non-alcoholic steatohepatitis. This is a condition in which changes in the liver resemble alcoholic hepatitis, but are not associated with alcohol intake. Non-alcoholic steatohepatitis can be combined with metabolic diseases: obesity, diabetes. In some cases, it occurs in people without concomitant diseases and even in children.
- Drug-induced hepatitis. Taking a number of medications - antibiotics, anti-tuberculosis drugs, oral contraceptives - sometimes leads to hepatitis. The likelihood of toxic effects of drugs on the liver is determined by individual tolerance to the drugs.
- Toxic hepatitis. It can be caused by poisonous mushrooms, alcohol substitutes, arsenic compounds, toluene, benzene, lead and other substances that have a direct destructive effect on liver cells.
- Autoimmune hepatitis. With this disease, the immune system is disrupted, which begins to destroy its own, normal liver cells. The mechanism of development of autoimmune hepatitis is not fully understood.
- Metabolic hepatitis. Caused by hereditary metabolic diseases, such as hemochromatosis (increased absorption of iron in the intestine with its deposition in the tissues of the body) or Wilson's disease (a disorder of copper metabolism with its deposition in the liver and other organs).
- Reactive hepatitis. It can be formed as a result of exposure to toxins and metabolic products that enter the blood during diseases of other organs (stomach ulcers, pancreatitis, endocrine and autoimmune diseases).
- Primary biliary hepatitis. Associated with impaired patency of the bile ducts, impaired outflow of bile, which leads to damage to liver tissue.
Liver cells in hepatitis can be damaged not only as a result of direct exposure to toxic substances, but also due to the pathological activity of cells of the body's own immune system. As a result, the functioning of the liver is disrupted, which leads to the characteristic symptoms of hepatitis: the liver increases in size, there is a feeling of heaviness in the abdomen, the outflow of bile necessary for the digestion of fats slows down, which causes nausea, vomiting, flatulence, stool disorders (diarrhea or constipation ). Violation of protein (albumin) synthesis leads to a decrease in the osmotic pressure of the blood and the release of fluid into the tissue, which causes edema. A decrease in the number of clotting factors leads to increased bleeding. The purification of the blood from toxic substances is impaired, which is manifested by weakness, malaise, and fever. Yellowness of the skin and mucous membranes is caused by an increase in bilirubin levels. It is formed during the destruction of red blood cells, binds to glucuronic acid in the liver (direct, bound bilirubin is formed) and is excreted in the bile. With hepatitis, this process is disrupted and direct bilirubin enters the blood.
Who is at risk?
- Alcohol abusers.
- Obese people.
- Patients with chronic autoimmune and endocrine diseases.
- Patients who require long-term use of medications that have a toxic effect on the liver.
- Contact with high doses of toxic chemicals.
Diagnostics
Manifestations of hepatitis depend on the immediate cause of liver damage. In some cases, hepatitis may have nonspecific symptoms or even be asymptomatic. A thorough interview and examination of the patient helps the doctor suspect hepatitis, but additional research is needed to make a final diagnosis.
Laboratory diagnostics
- General blood analysis. An increased level of white blood cells is a sign of the infectious nature of hepatitis.
- Prothrombin index. This is the ratio of the blood clotting time of a healthy person to the clotting time of a sick person. Prothrombin is a precursor of thrombin and is involved in blood clotting. The test is used to evaluate the rate of blood clotting. In the initial stages of hepatitis, the prothrombin index is normal; in severe cases of the disease it can be reduced.
- Fibrinogen. A blood clotting factor that is synthesized by liver cells. When liver tissue is damaged, fibrinogen is reduced.
- AST (aspartate aminotransferase), ALT (alanine aminotransferase). Liver enzymes that enter the bloodstream when liver tissue is damaged. With hepatitis, they may be increased.
- Gamma-glutamyl transpeptidase (gamma-GT). A liver enzyme, the amount of which increases with damage to the liver and bile ducts.
- Alkaline phosphatase. An enzyme that is found in all tissues of the body, but in the greatest quantities in bones, kidneys and liver. In case of hepatitis, it may be increased.
- Total bilirubin. Bilirubin in hepatitis is increased mainly due to the direct (bound) fraction.
- Total whey protein. With hepatitis, the level of total protein can be reduced by reducing the amount of albumin.
- Total cholesterol. This substance is synthesized in the liver and is an element of cell membranes, a precursor of bile acids and some hormones. In case of hepatitis, it may be lowered, which indicates a violation of the synthetic function of the liver.
- Tests for hepatitis B, C, D. The presence of hepatitis viruses in the body is determined as a possible cause of the disease.
- Ferritin, transferrin. Ferritin is a protein that binds iron in the liver, and transferrin is a protein that transports iron from the intestines to the liver. Their levels may be elevated in hemochromatosis.
- Copper, ceruloplasmin. The level of these substances is measured when Wilson's disease is suspected, in which the concentration of ceruloplasmin decreases and the concentration of copper increases.
- Screening study for the presence of narcotic, psychotropic and potent substances. Determination of compounds that could cause hepatitis.
Additional Research
- Ultrasound of the abdominal organs. Used to determine the size and structure of the liver. With hepatitis, the liver may be enlarged.
- X-ray, CT, MRI. Helps determine the size and structure of the liver, and exclude other liver diseases.
- Retrograde cholangiography. This is an x-ray examination, which is carried out after the injection of a contrast agent into the bile ducts, visible in the image. Used to assess the patency of the bile ducts.
- Liver biopsy. Taking a sample of liver tissue using a thin, hollow needle that is inserted through the skin of the abdominal wall after preliminary anesthesia. It is carried out under ultrasound control. Microscopy of the sample taken reveals inflammation of the liver tissue, accumulation of leukocytes, and a small amount of connective tissue while maintaining the structure of the liver lobules.
Treatment
Treatment of acute hepatitis is based, first of all, on stopping the impact of the pathological factor on the liver and is aimed at preventing the disease from becoming chronic. Most acute hepatitis is completely curable. Chronic hepatitis, depending on the cause and activity of the process, can last from 6 months to several years. A long course involves regular examinations, strict adherence to the doctor’s recommendations, changes in the patient’s lifestyle - this is necessary for the prevention of liver cirrhosis, liver failure, and liver cancer.
Prevention
- Quitting alcohol and drugs.
- Follow the instructions and recommendations of the doctor when taking medications.
- Use of protective equipment when working with toxic chemicals.
- Fighting excess weight.
Recommended tests
- General blood analysis
- Coagulogram No. 2 (prothrombin (according to Quick), INR, fibrinogen)
- Alanine aminotransferase (ALT)
- Aspartate aminotransferase (AST)
- Gamma-glutamyl transpeptidase (gamma-GT)
- Total alkaline phosphatase
- Total bilirubin
- Direct bilirubin
- Total protein in whey
- Serum albumin
- Total cholesterol
- Transferrin
- Ferritin
- Ceruloplasmin
- Copper in the blood
- HBsAg, hypersensitive
- Anti-HCV, antibodies
- Screening study for the presence of narcotic, psychotropic and potent substances
- Cytological examination of punctates, scrapings of other organs and tissues
Signs of chronic hepatitis
Chronic hepatitis is characterized by weakness and fatigue, and asthenic syndrome manifests itself. The patient's condition worsens significantly if liver cirrhosis develops. Then the signs of chronic hepatitis become jaundice (yellowness of the sclera, icteric skin tone, darkening of urine, discoloration of feces, etc.), the abdomen enlarges. Sometimes hepatic encephalopathy develops; when the brain is damaged, its activity is disrupted, and hallucinations may occur.
Signs of chronic hepatitis do not appear immediately in patients; the first stages of the disease can be asymptomatic, which makes it especially dangerous. Chronic hepatitis is often detected during examination in connection with other diseases.
Hepatitis B: carriage or disease leading to cirrhosis and cancer?
Hepatology, the study and development of new treatments for liver disease, has made incredible progress over the past two decades. Methods for accurate virological assessment of the activity of hepatitis C and B viruses in the human body, which are the most common causes of chronic hepatitis, cirrhosis, and liver cancer, have been developed and implemented. So-called “non-invasive” methods have been developed and are widely used, that is, without the use of liver biopsy, diagnosing the degree of liver damage, or establishing the stage of cirrhosis. Even more impressive progress has been made in the treatment of these diseases. We have discussed the problem of hepatitis C many times. One has only to add that a new era is opening in the treatment of hepatitis C - drugs with a direct antiviral effect have been developed and are already beginning to be used, thanks to which it is believed that within a decade it will be possible to achieve one hundred percent effectiveness of treatment. In this article we will talk about hepatitis B and new advances in its treatment.
What to do if you are diagnosed with HBsAg?
Unfortunately, hepatologists are often faced with underestimation on the part of the patient, as well as doctors of other specialties, of the seriousness of HBsAg detected over many years. A patient who is diagnosed with HBsAg for the first time must undergo an examination, which will make it possible to make a correct diagnosis - to distinguish between inactive carriage of HBsAg and active chronic hepatitis B that requires treatment. To do this, the hepatologist will suggest that you do a number of studies: - a study of a biochemical blood test, - a study of the viral load using quantitative PCR (polymerase chain reaction) - a study for the presence of another protein (or antigen) of the hepatitis B virus, which characterizes the high infectiousness of the patient, — HBeAg — study for the presence of a companion virus of hepatitis B - delta virus — study of alpha-fetoprotein (tumor marker of a liver tumor) — ultrasound examination of the liver — fibroelastography to clarify the stage of liver fibrosis (other studies are possible according to indications)
The hepatitis B virus is 100 times more contagious than HIV (human immunodeficiency virus).
Despite the widespread introduction of vaccination against hepatitis B, the prevalence of the disease remains high. In different regions of Russia, the prevalence of carriage of the virus ranges from 1.5% to 11.5%. As with hepatitis C, the source of infection is the blood of an infected person. The routes of infection are similar: the use of non-sterile needles, instruments for various medical and non-medical (piercing, tattoos, manicure/pedicure) manipulations, the use of personal hygiene items of an infected person in everyday life (razor, scissors, toothbrush, etc.), unprotected sexual contact, transmission of the virus from an infected mother to her child. The hepatitis B virus is more stable in the external environment and more contagious than the hepatitis C viruses and human immunodeficiency viruses. Therefore, the natural routes of transmission of the B virus (sexual transmission and mother-to-child transmission) are more significant for this virus.