Depakine is a derivative of valproic acid, a component of the plant Valeriana officinalis
.
More than 100 years ago, valproic acid was synthesized for technical purposes, namely as a solvent. As happened in its time with phenobarbital, its antiepileptic effect was discovered by accident. Research conducted in 1962 at Laboratoire Berthier in Grenoble led to a patent on the antiepileptic properties of valproic acid. The Berthier laboratory then transferred the rights to its development and distribution, which subsequently formed the basis.
Throughout use, the drug becomes more and more convenient to use and more effective: from conventional tablets and liquid forms for children, tablets with a special coating with slow release (Depakine Enteric, Depakine-Chrono) to granule forms made using new technologies, conveniently packaged 100, 250, 500 and 1000 mg, tasteless and odorless and allow you to take it once a day (Depakine Chronosphere); liquid forms are available in solution and syrup.
The mechanism of action of depakine is primarily an increase in inhibitory GABAergic mediation due to inhibition of enzymes involved in the degradation of valproic acid, GABA transaminase and aldehyde reductase, as well as activation of the synthesis of GABA from glutamic acid by activating glutamic acid decarboxylase. There are other mechanisms: blockade of T-type Ca2+ channels, in particular neurons of the nonspecific nuclei of the thalamus. This explains the effect of depakine on one of its targets—absence, which is realized by blockade of corticothalamic reverberation of spike-wave activity with a frequency of 3 Hz. There are two types of postsynaptic receptors - GABA-A and GABA-B. GABA-A postsynaptic receptors mediate fast synaptic transmission that mediates inhibition. Their activation opens chloride channels, causing hyperpolarization. There are presynaptic and postsynaptic GABA-B receptors. Presynaptic modulate the release of a number of transmitters, including glutamate. Postsynaptic receptors are coupled to the G-protein coupled receptor. Their function is to open potassium channels and close calcium channels. The opening of potassium channels causes hyperpolarization, a mechanism for inhibiting epileptic activity. The action through an intermediary, the G protein, takes a slightly longer time, but this mechanism is the main one in the formation of a slow post-spike wave in absence forms of epilepsy [1], as well as in the cessation of spike-wave discharges [2]. Thus, depakine has a multicomponent mechanism of action.
Since the 80s of the last century, convulex began to be used in our clinic, and in 1990-1992. Depakine was tested. The results of clinical studies of depakine made it possible to formulate the position that, from the point of view of its effect on epileptic seizures, depakine is an ideal antiepileptic drug, since it meets the requirement to be, on the one hand, focused on a specific target, and on the other hand, to have a broad range of action [3]. It has been established that it is able to have an effect on all types of epileptic seizures, and at the same time, its main target is absence seizures and primary generalized convulsive seizures, where its effectiveness reaches 70%. It has also been shown that the target of valproate is idiopathic epilepsy with all forms of seizures - convulsive, absence, myoclonic. Another target of valproate action is epileptic encephalopathies, including the most severe “catastrophic” forms of childhood epilepsies, including attack-free variants of epileptic encephalopathy, as well as some so-called benign partial epilepsies of childhood.
Currently, depakine occupies the place that previously belonged to phenobarbital. There are two main drugs on the Russian market - Depakine and Konvulex, which are the disodium salt of valproic acid and contain a small amount of valproic acid itself, as well as a number of generics. In the United States, the preferred form contains equal amounts of valproic acid and its sodium salt—divalproex.
The therapeutic level of depakine in the blood is quite wide - 50-140 mcg/ml. When treated with valproate, unlike other antiepileptic drugs (AEDs), doses can be rapidly increased if necessary. Peak concentration in the blood is reached after 1-2 hours, for slow-release forms - after 4-8 hours, half-life is 9 hours, in children - up to 2 months.
Depakine is approved for use from 6 months of age (doses in children 60 mg or more).
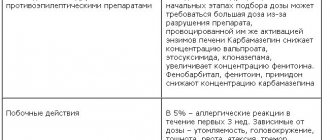
Valproates slow down the action of microsomal liver enzymes, and therefore can increase the level of enzyme-inducing AEDs in the blood. Concomitant use with carbamazepine leads to a decrease in the level of valproate and an increase in the level of carbamazepine; when valproate is combined with lamotrigine, the level of the latter can double or more.
The most common side effects during treatment with valproate are tremor, hair loss, weight gain, menstrual irregularities, polycystic ovary syndrome, and a high risk of teratogenic effects on the fetus. In addition, an unfavorable effect of valproate on the liver has been noted, so during the treatment process it is necessary to monitor the content and activity of liver enzymes in the blood. As a rule, these side effects are dose-dependent. We observed more rare side effects in 10.3% of cases when using conventional forms of Depakine. They were not dose-related and were usually resolved by switching patients to film-coated formulations of Depakine. We are talking about hyperammonemia, which explains cases of drowsiness, loss of appetite, vomiting, and, when combined with barbiturates, stupor. Hyperglycemia and aminoaciduria may also occur, and hyponatremia is possible. We observed a unique case of pontine myelosis as a consequence of uncontrollable hyponatremia during treatment with Depakine. Symptoms of stomach irritation (pain, nausea, etc.) are common, which in some cases can be avoided by using coated tablets.
The Pharmacovigilance Committee of the European Regulatory Agency (PRAC) [4] has drawn particular attention to the adverse effects of valproate in women of reproductive age. It was decided to inform all professionals and women with epilepsy - potential mothers, as well as girls (including puberty) about the increased risk of adverse effects of valproate on the fetus. In this case, we mean not only the risk of malformations (on average 10%), but also disorders in preschool age associated with walking, speech, memory and intellectual abilities. The use of valproate in women of childbearing age with these conditions should be carried out only if effective methods of contraception are used. The US Food and Drug Administration (FDA) classifies valproate as Category D (there is evidence of risk to the fetus, but the benefit may outweigh the risk) when used during pregnancy for epilepsy and mania in bipolar disorder; they are not suitable for the prevention of migraine during pregnancy (category X). According to the guidelines of the UK National Institute for Health and Clinical Excellence [5], a relatively safe dose of valproic acid during pregnancy is considered to be 800 mg/day. At the same time, in order to prevent fetal malformations, it is recommended to prescribe folic acid 5 mg/day.
Having 25 years of experience in the use of valproates (more than 3,000 patients of different sexes from 1 year to 74 years), we have reason to emphasize that the dose-dependence of adverse events is expressed to one degree or another in all AEDs, but for valproates, due to the sufficient severity of such phenomena, such as menstrual irregularities, weight gain, metabolic syndrome, it is especially significant.
But along with the noted unfavorable aspects of the action of valproates, it is necessary to note the advantages of their use in women: they do not reduce the concentration of hormones in the luteal phase of the menstrual cycle; during pregnancy, the increase in the volume of distribution is compensated by an increase in the free fraction in the blood; valproates are practically not excreted in breast milk.
We conducted a study of the health of more than 150 women with epilepsy of reproductive age taking various AEDs, including valproate. In 30% of women receiving valproic acid drugs (at a dose of more than 1200 mg/day), ovarian dysfunction was identified in the form of various menstrual cycle disorders, which was dose-dependent and reversible. Some patients had moderate functional hyperprolactinemia, hypoprogesteronemia, and slight hyperandrogenism, which required observation by a gynecologist-endocrinologist. But in not a single case were classic signs of polycystic ovary syndrome identified, and therefore it was concluded that this syndrome is not typical for women with epilepsy taking AEDs, and menstrual irregularities are reversible [6].
We have developed an algorithm for the use of valproate in women of childbearing age and pregnant women suffering from epilepsy, depending on various clinical situations, which is reflected in a number of publications [7, 8]. The corresponding recommendations of the Expert Council on the use of valproate in women with epilepsy were also published [9], using a contractual model in the relationship between a doctor and a patient - a woman of reproductive age, signing informed consent in light of the requirements of the UNESCO Universal Declaration of Bioethics and Human Rights.
T. Thomson et al. [10], considering PRAC restrictions on the use of valproate in women, also emphasize possible exceptions to the general rules, considering the characteristics of the course of epilepsy itself and the possibility of women having diseases that may make pregnancy impossible.
Valproates remain the most effective in some forms of epilepsy, for example, in its most common form, juvenile myoclonic epilepsy, and in some epileptic encephalopathies, in particular non-paroxysmal epileptic disorders with mental and behavioral disorders, they remain the first choice [11].
In practice, when treating with valproates, we always perform slow titration of doses, give preference to low doses, and if the therapeutic effect is insufficient, we combine valproates with levetiracetam, lamotrigine and other AEDs.
By the beginning of 2000, we analyzed the results of using Depakine and Depakine-Chrono as mono- and polytherapy in 137 patients with different forms of epilepsy. The advantage of depakine-chrono over its conventional form has been shown, primarily in the form of better tolerability. In particular, it was found that the Depakine Enteric form (coated tablets with release of the active substance in the intestine) usually does not cause adverse events.
Data were analyzed regarding 79 patients who, in accordance with the provisions of modern biomedical ethics on informed consent, after being informed about the different dosage forms of Depakine, were given the opportunity to make their own choice and justify it. Taking depakine chronosphere was recommended once a day with dinner. The choice of this particular drug in the vast majority of patients was justified by two circumstances: the employment of patients (people with irregular working hours, combining study with work), as well as taking into account periods of sleep (from previous experience, patients knew that the highest dose/concentration of AEDs is ensured by taking the drug at hours preceding attacks). In isolated cases, patients were simply attracted by the ease of use. As for retention, after a year and a half it was 90%. This may be due to the fact that the doses of the drug in question, as a rule, did not exceed 1000 mg, since depakine was usually prescribed in combination with other AEDs, most often lamotrigine or trileptal. By 2008, the results of treatment with depakine in 1000 patients were analyzed, of which 166 with idiopathic epilepsy, 69 patients with epileptic encephalopathy, 721 with symptomatic and cryptogenic epilepsy and 50 with unidentified forms, mainly myoclonic (in addition to juvenile myoclinic epilepsy). The results of treatment of patients with idiopathic epilepsy are presented in table. 1.
Table 1. Distribution of patients with different forms of idiopathic epilepsy according to treatment results Note. JME - juvenile myoclonic epilepsy, DAE - childhood absence epilepsy, JAE - juvenile absence epilepsy, EGTCPP - generalized epilepsy with tonic-clonic seizures of awakening. When interpreting the data presented in it, one should only keep in mind that idiopathic partial epilepsy is a “self-limiting”, i.e., age-limited benign form of the disease.
As for patients with symptomatic/cryptogenic epilepsy, valproate alone was effective in 42% of patients, and as a combination therapy, where depakine was added to carbamazepine, in another 16%. This information corresponds to the findings of R. Mohanaraj and M. Brodie [12], which indicate good results from the use of valproate as monotherapy for local epilepsy (42% of patients), as well as the data of P. Kwan, M. Brodie [13], which in In such cases, when using a second AED when the first one is ineffective, the goal is achieved in 13% of cases.
We noted a therapeutic response in only 12 patients, 7 of whom were children of the first or second year of life (the age at which the development of excitatory glutamatergic receptors greatly advances the development of inhibitory GABAergic receptors). In 90% of cases it was symptomatic partial epilepsy.
Although the issue of the use of valproates in symptomatic (partial, focal) epilepsy is still debated, it can be noted that the proportion of incurable patients has been consistently decreasing and has reached a minimum in the “valproic era”.
To date, the array of our observations amounts to more than 1600 cases of the use of valproate in the ambulance service, in the clinic, hospital and intensive care units, and the array of the Department of Neurology of the Moscow State Medical and Dental University is more than 5000 patients. Valproates have shown themselves to be the first choice for epileptic encephalopathy type II and idiopathic epilepsy, for convulsive and non-convulsive status epilepticus (along with benzodiazepines) and have become an important component of combination therapy for both generalized and partial (focal) epilepsy due to their high efficiency, good portability and accessibility. In case of symptomatic partial epilepsy in epilepsy monotherapy, according to the criterion of effectiveness/tolerability, valproates are not inferior to modern AEDs and the preference in such cases for levetiracetam, lamotrigine, topiramate occurs solely due to the limitation of their use in women of childbearing age.
In the process of a comprehensive study of the effects of valproate (Depakine), their effect on memory, attention and anxiety levels was studied in 40 patients with cryptogenic and symptomatic epilepsy. An improvement in all studied cognitive indicators was noted [14, 15]. In addition, it was found that depakine also has an anxiolytic effect.
A number of foreign and domestic studies were specifically aimed at comparing the effectiveness of valproate and other AEDs. Thus, in 2004, a large open randomized trial, SANAD, was completed in the UK [16], which aimed to compare the effectiveness of treatment of generalized seizures with valproic acid, lamotrigine and topiramate. In terms of time to drug discontinuation due to treatment failure, valproate was significantly superior to topiramate, although there was no difference with lamotrigine. In patients with idiopathic generalized epilepsy, valproate was significantly more effective than both other agents. Valproate was significantly superior to lamotrigine for 12-month remission, and superior to topiramate only in the generalized idiopathic epilepsy subgroup. Also noteworthy is the COMET study [17]: a 52-week, open-label, randomized comparative study of the effectiveness of levetiracetam, carbamazepine (controlled release of the active substance) and sodium volproate in patients with newly diagnosed partial epilepsy. There was only one evaluation criterion - the time before refusing treatment for any reason. It was concluded that the effectiveness of treatment with levetiracetam was no greater than that of carbamazepine and sodium valproate.
As noted above, currently one of the main problems in the treatment of epilepsy is its symptomatic pharmacoresistant form. At the same time, it is believed [13, 18, 19] that after ineffective monotherapy, polytherapy with a combination of sodium channel inhibitors with activators of GABAergic transmission or broad-acting AEDs, which also have a similar function, can be used [13, 18, 19]. Our experience in combination therapy for partial (focal) epilepsy, where valproate was used as a second-choice drug after carbamazepine, was given above.
Valproates are the drug of choice in almost half of the cases of idiopathic cryptogenic epilepsy, in which we were able to show, including in joint studies with the Scientific Center of Neurology, a significant idiopathic component, which is the target of valproic acid. Finally, in all cases of unclassified epilepsy or in forms of the disease in which the doctor finds it difficult to identify it, valproic acid should be recognized as the drug of choice, which has proven high efficacy, good tolerability and retention of patients on treatment in comparison with topiramate and lamotrigine [20].
In the last decade, therapeutic drug monitoring (TDM) has played a significant role in clinical practice. According to Yu.B. Belousova et al. [21], who treated 614 patients, the number of cases of failure to achieve therapeutic concentrations when using valproates was 2.5 times higher, and the number of cases of overdose was 10 times less compared with carbamazepine. This indicates that the adequacy of the use of valproates in clinical practice is much higher than that of carbamazepines, i.e. valproates are more convenient for clinical use.
To this we can add the study of A.V. Sokolova et al. [22], which convincingly proved the reliability of the differences in the pharmacokinetic parameters of various valproic acid preparations with controlled release of the active substance (Depakine Chronosphere). The indicators of generic drugs - Convulex, Valparin XP and Encorate Chrono - differed significantly from Depakine, which indicates their non-equivalence to Depakine Chronosphere. As a result, the authors made recommendations to reduce their single/daily dose and the need for more frequent use of the listed AEDs.
To the above, it should be added that in our country the most important factor in state policy in the field of medicine has become economic. Therefore, unfortunately, the lists of preferential drugs for patients include not original AEDs, but generics, dooming many patients to sometimes life-long ineffective treatment, and this ultimately leads to unjustified economic costs. From these positions, one more advantage should be attributed to Depakine: it is the only economically available remedy. Therefore, in conclusion, we will refer to the opinion of those who have extensive experience in its use in Russia. Let's start with attempts to replace the original drug with reproducible copies (generics).
Data from P.N. were published. Vlasova et al. [23], based on an analysis of the treatment results of 493 patients. Already within the first month, 16.6% of patients who replaced Depakine Chronosphere with Convulex required to return to the former due to severe side effects (urticaria, gastric disorders) or an increase in epileptic seizures. Similar materials were recently published by Yu.B. Belousov et al. [24]. The authors showed that the cost-effectiveness of transferring adult patients with focal epilepsy from the original (reference) drug valproic acid Depakine Chronosphere to generic drugs is extremely low due to the lower clinical effectiveness of the generic, which leads to increased costs for medical care in general and increases indirect costs. Transferring patients in remission from the drug Depakine Chronosphere to generic tablets of valproic acid is inappropriate from a clinical point of view and unprofitable from an economic point of view (Table 2).
Table 2. Result of replacing Depakine Chronosphere with generics [24]
The above justifies the conclusions of a number of domestic researchers.
L.R. Zenkov [25] in the article “Valproic acid in retro- and perspective” (2005) wrote that valproates have a wide therapeutic spectrum - effectiveness against all types of attacks; multimodality of mechanisms of action; lack of influence on the effectiveness of most concomitantly used AEDs and drugs of other groups; good tolerability and absence of significant adverse events associated with the combination; lack of seizure aggravation potential.
V.A. Karlov [26] stated: “The properties of valproic acid, such as breadth of action - effectiveness against various types of seizures and forms of epilepsy, good tolerability, minimal risk of aggravation, high percentage of retention on monotherapy, the presence of a variety of dosage forms and forms for intravenous administration, favorable pharmacokinetic and pharmacodynamic profile make it irreplaceable in our time.”
We find a similar opinion in the article by P.N. Vlasova “Focal epilepsies: selection of antiepileptic drugs in outpatient settings” [27]. I.G. Rudakova [19] in 2015 spoke as follows: “It is impossible not to note the high demand for valproates in rational combination therapy regimens for both generalized and focal epilepsies, which persists despite the emergence of the generation of new highly effective AEDs. The clinical and pharmacoeconomic characteristics of valproates make them an indispensable means of modern pharmacotherapy for epilepsy. High efficiency in most forms of epilepsy and types of seizures, good tolerability, optimal retention rates on therapy and minimal potential for aggravation, along with accessibility for the vast majority of patients, determine the advantages of choosing valproate in combination therapy for epilepsy.”
On September 30, 2022, an Expert Council was held with the participation of members of the Russian Antiepileptic League on the use of Depakine in modern conditions in Russia. General practitioners were recommended to begin treatment of patients with the prescription of Depakine.
Thus, time has shown that valproates, and primarily such an original drug as Depakine, turned out to be not only modern AEDs, but also antiepileptic drugs of the future. We can only recall that the scope of application of depakine, in addition to epilepsy, includes catastrophic forms of non-paroxysmal manifestations of persistent epileptiform activity - epileptic encephalopathy, where they are the first choice, as well as bipolar disorders and some forms of neuropathic pain.
The author declares no conflict of interest.
Depakin
Depakine (sodium valproate) is an anticonvulsant drug used to treat epilepsy. According to statistics from the World Health Organization, the prevalence of epilepsy in developed countries is 1-2%, i.e. This disease affects every 1-2 people out of a thousand. In the absence of adequate therapeutic measures, such patients develop mental disorders such as delusions, hallucinations, dysphoria, etc. If the patient receives the correct treatment, he remains, in fact, a full member of society, being an employed, adapted and successful person. The countries of the former Union are characterized by the lack of timely diagnosis of epilepsy associated with the mild course of the disease (without seizures). Another problem is that in our country, patients suffering from epilepsy must be observed by psychiatrists (in this case, the factor of stigma and public censure plays a role). At the same time, in the arsenal of a modern doctor there are effective means for the treatment of epilepsy. One of these drugs is Depakine from. It is used in many countries and is recommended for use by the International League Against Epilepsy. The drug reduces the excitability of the motor areas of the cerebral cortex, and also increases the threshold of their convulsive readiness. At the same time, patients’ mood and psycho-emotional state improve. Valproic acid, the active component of the drug, is quickly and completely absorbed in the digestive tract, which ensures high (93%) bioavailability - an integral component of the therapeutic effectiveness of any drug. It is important that the degree of intestinal fullness does not affect bioavailability.
The maximum concentration of the active component in the blood is observed 1-3 hours after administration. The half-life of the drug ranges from 8 to 20 hours. Elimination from the body is carried out by the kidneys. The dosage regimen for Depakine is individual. The frequency of administration is 2-3 times a day. The optimal time to take it is with food. During pregnancy and breastfeeding, it is recommended to refrain from taking Depakine. Reproductively active women are advised to use contraceptive medications or other reliable contraceptive options while taking the drug. In case of liver dysfunction, Depakine is contraindicated; in case of kidney dysfunction, special care should be taken when prescribing the drug. Caution is also required in patients with pathologically altered blood count. In persons taking other antiepileptic drugs, Depakine should be started gradually, observing the principle of gradually increasing the dose and reaching a clinically effective dose no earlier than the end of the 2nd week of drug therapy. After this, a gradual withdrawal of other antiepileptic drugs is carried out. If Depakine is taken as part of monotherapy, then reaching a clinically effective dose should occur at the end of the first week of the drug course. Combined pharmacotherapy increases the risk of developing unwanted side effects from the liver. During the drug course with Depakine, it is necessary to monitor the functional activity of the liver, blood counts, and the state of the coagulation system. Particular care must be taken when operating potentially hazardous machinery, including driving a vehicle.
Depakine® chrono
Before starting to use the drug and periodically during the first 6 months of treatment, especially in patients at risk of developing liver damage, liver function tests should be performed.
As with the use of most antiepileptic drugs, when using valproic acid, a slight increase in the activity of “liver” transaminases is possible, especially at the beginning of treatment, which occurs without clinical manifestations and is transient. In such patients, it is necessary to conduct a more thorough study of biological parameters, including the prothrombin index. It may be necessary to adjust the dose of the drug, and, if necessary, repeat clinical and laboratory examination.
Before starting therapy or before surgery, as well as in the event of spontaneous occurrence of subcutaneous hematomas or bleeding, it is recommended to determine the bleeding time and the number of formed elements in the peripheral blood, including platelets.
Severe liver damage
Predisposing factors
Isolated cases of severe liver damage, sometimes fatal, have been described. Clinical experience shows that patients taking multiple antiepileptic drugs at the same time and patients taking salicylates at the same time (since salicylates are metabolized through the same metabolic pathway as valproic acid) are at risk.
Suspicion of liver damage
For early diagnosis of liver damage, clinical observation of patients is mandatory. In particular, you should pay attention to the following symptoms that may precede the onset of jaundice, especially in patients at risk:
- nonspecific symptoms, especially those that began suddenly, such as asthenia, anorexia, lethargy, drowsiness, which are sometimes accompanied by repeated vomiting and abdominal pain;
- resumption of seizures in patients with epilepsy.
Patients or their family members (when using the drug in pediatric patients) should be warned that they should immediately report the occurrence of any of these symptoms to their doctor. Patients should immediately undergo clinical examination and laboratory testing of liver function tests.
Revealing
Liver function tests should be performed before starting treatment and then periodically during the first 6 months of treatment. Among conventional studies, the most informative are studies reflecting the state of the protein-synthetic function of the liver, especially the determination of the prothrombin index. Confirmation of deviation from the norm of the prothrombin index in the direction of its decrease, especially in combination with deviations from the norm of other laboratory parameters (a significant decrease in the content of fibrinogen and blood clotting factors, an increase in the concentration of bilirubin and an increase in the activity of “liver” transaminases), as well as the appearance of other symptoms indicating for liver damage, requires discontinuation of the drug. As a precaution, if patients were taking salicylates concomitantly, their use should also be discontinued.
Pancreatitis
There are rare reported cases of severe forms of pancreatitis in children and adults, which developed regardless of age and duration of treatment. Several cases of hemorrhagic pancreatitis have been observed with rapid progression of the disease from the first symptoms to death.
Children are at increased risk of developing pancreatitis, and this risk decreases with increasing age of the child. Risk factors for developing pancreatitis may include severe seizures, neurological disorders, or anticonvulsant therapy. Liver failure combined with pancreatitis increases the risk of death.
If severe abdominal pain, nausea, vomiting and/or anorexia occur, patients should be evaluated immediately. If pancreatitis is confirmed, in particular, with increased activity of pancreatic enzymes in the blood, the use of valproic acid should be discontinued and appropriate treatment should be started.
Suicidal thoughts and attempts
Suicidal ideation and suicide attempts have been reported in patients taking antiepileptic drugs for some indications. A meta-analysis of randomized placebo-controlled trials of antiepileptic drugs also showed a 0.19% increase in the risk of suicidal ideation and suicide attempts in all patients taking antiepileptic drugs (including a 0.24% increase in this risk in patients taking antiepileptic drugs for epilepsy), compared with their frequency in patients taking placebo. The mechanism of this effect is unknown.
Therefore, patients taking the drug should be constantly monitored for suicidal thoughts and suicide attempts, and if they occur, appropriate treatment should be provided. Patients and their caregivers are advised to immediately consult a physician if they experience suicidal thoughts or suicide attempts.
Carbapenems
The simultaneous use of carbapenems is not recommended (see section “Interaction with other drugs”, “With caution”).
Patients with established or suspected mitochondrial diseases Valproic acid may initiate or aggravate the manifestations of the patient's existing mitochondrial diseases caused by mutations in mitochondrial DNA, as well as in the nuclear gene encoding the mitochondrial enzyme γ-polymerase (POLG). In particular, in patients with congenital neurometabolic syndromes caused by mutations in the gene encoding γ-polymerase (POLG), such as patients with Alpers-Huttenlocher syndrome, valproic acid is associated with a higher incidence of acute liver failure and liver-related deaths. outcomes. The presence of diseases caused by defects in γ-polymerase can be assumed in patients with a family history or symptoms of such diseases, including encephalopathy of unknown origin, refractory epilepsy (focal, myoclonic), status epilepticus, mental and physical retardation, psychomotor regression, axonal sensorimotor neuropathy, myopathy, cerebellar ataxia, ophthalmoplegia or complicated migraine with visual (occipital) aura. In accordance with current clinical practice, testing for mutations in the polymerase γ gene (POLG) should be performed to diagnose such diseases (see section "Contraindications").
Paradoxical increase in the frequency and severity of seizures (including the development of status epilepticus) or the emergence of new types of seizures
As with other antiepileptic drugs, when taking valproic acid, instead of improvement, some patients experienced a reversible increase in the frequency and severity of seizures (including the development of status epilepticus) or the appearance of new types of seizures. If seizures worsen, patients should immediately consult their doctor (see section "Side effects").
Female children and adolescents, women of childbearing potential and pregnant women
Pregnancy Prevention Program
Valproic acid has a high teratogenic effect; the use of valproic acid leads to a high risk of congenital malformations and developmental disorders of the central nervous system in the fetus.
The use of valproic acid is contraindicated:
- during pregnancy for epilepsy, except in cases of absence of alternative treatment methods (see sections “Special instructions”, “Use during pregnancy and during breastfeeding”);
— during pregnancy in the treatment and prevention of bipolar affective disorders;
- in women of childbearing potential, unless all the conditions of the Pregnancy Prevention Program are met (see sections “Special Instructions”, “Use during Pregnancy and Breastfeeding”).
When prescribing drugs containing valproic acid, you must:
— conduct an individual assessment of the circumstances of prescribing the drug in each individual case, discuss possible methods of therapy and make sure that the patient understands the potential risks and the need for measures taken to minimize them;
— make sure that the patient has childbearing potential;
— make sure that the patient understands the nature and magnitude of the risks of using valproic acid during pregnancy, in particular, the risks of teratogenic effects, as well as the risks of disorders of the mental and physical development of the child;
— make sure that the patient understands the need to conduct a pregnancy test before starting and during treatment;
- explain the necessary methods of contraception, make sure that the patient uses reliable methods of contraception continuously during treatment with drugs containing valproic acid;
— make sure that the patient understands the need to regularly contact a specialist in the treatment of epilepsy and bipolar affective disorders (at least once a year) to re-analyze the prescribed therapy;
- make sure that the patient understands the need to contact her doctor if she is planning a pregnancy in order to promptly assess the possibility of switching to alternative therapy before stopping the use of contraception;
- inform about the need for immediate consultation with your doctor if you suspect pregnancy;
— ensure that the patient has received all the necessary explanations about the risks and necessary precautions.
The above information is also relevant for women who are not currently sexually active, unless the attending physician is satisfied that there is no childbearing potential.
Female pediatric patients
When prescribing drugs containing valproic acid, you must:
— make sure that female pediatric patients/their legal representatives understand the need to consult with their doctor upon the onset of menarche;
— ensure that female pediatric patients who have reached menarche, or their legal representatives, receive detailed information about the risks of congenital malformations and disorders of the central nervous system in the fetus.
The treating physician should annually re-evaluate the prescribed valproic acid therapy and evaluate the possibility of prescribing alternative therapy. If drugs containing valproic acid are the treatment of choice, it is necessary to ensure that reliable methods of contraception are used and that the terms of the Pregnancy Prevention Program are followed. Before puberty, the possibility of switching patients to alternative treatment methods should be constantly considered.
Pregnancy test
Before starting treatment with drugs containing valproic acid, it is necessary to exclude pregnancy. Therapy with drugs containing valproic acid cannot be prescribed to women of childbearing potential unless a negative pregnancy test (pregnancy blood test) has been confirmed by a health care professional to prevent the drug from being prescribed during pregnancy.
Contraception methods
Female patients of childbearing potential who are prescribed therapy with drugs containing valproic acid should use reliable methods of contraception continuously throughout the entire treatment period.
Female patients of childbearing potential should be provided with detailed information about methods of preventing pregnancy, and such patients may also seek advice from their physician if they are not using a reliable method of contraception.
You must use at least one reliable method of contraception (preferably simultaneously with methods such as an intrauterine system or implant) or two complementary methods of contraception, including barrier methods. When prescribing a contraceptive method to a patient, it is necessary to take an individualized approach and discuss all possible contraceptive options with the patient to ensure that the patient adheres to and adheres to the regimen. In case of amenorrhea, the patient should also be warned about the use of effective methods of contraception.
Annual analysis of prescribed therapy
At least once a year, the treating physician should evaluate whether medications containing valproic acid are the treatment of choice. The risks associated with therapy should be discussed when prescribing the drug and at each annual review of the prescribed therapy, and ensure that the patient understands all risks.
Planning a pregnancy
If a patient is planning a pregnancy, a specialist in the treatment of epilepsy and bipolar affective disorder should evaluate therapy with drugs containing valproic acid and consider alternative therapy. Every effort should be made to switch the patient from therapy with drugs containing valproic acid before conception and until contraception is discontinued (see section “Use during pregnancy and breastfeeding”). If alternative therapy is not available, the patient should be advised of the risks associated with the use of drugs containing valproic acid for the unborn child to help make an informed decision about family planning.
What to do if you become pregnant?
If you become pregnant, you should contact your healthcare provider immediately to evaluate your treatment and consider alternative therapy.
The health worker must ensure that:
— patients understand all the risks described above;
— patients received recommendations not to stop therapy with valproic acid and to immediately contact their doctor when planning pregnancy.
Concomitant use with estrogen-containing drugs
Valproic acid does not reduce the therapeutic effectiveness of hormonal contraceptives. However, drugs containing estrogen, including estrogen-containing hormonal contraceptives, may increase the clearance of valproic acid, which may lead to a decrease in its serum concentration and, consequently, a decrease in its effectiveness. It is necessary to monitor the concentration of valproic acid in the blood serum and clinical effectiveness (seizure control and mood control) when prescribing or discontinuing estrogen-containing drugs (see section "Interaction with other drugs").
Kidney failure
It may be necessary to reduce the dose of valproic acid due to an increase in the concentration of its free fraction in the blood serum. If it is impossible to monitor plasma concentrations of valproic acid, the dose of the drug should be adjusted based on clinical observation of the patient.
Enzyme deficiency of the carbamide cycle (urea cycle)
If an enzymatic deficiency of the carbamide cycle is suspected, the use of valproic acid is contraindicated. In such patients, several cases of hyperammonemia with the development of stupor or coma have been described. In these cases, metabolic studies should be carried out before starting treatment with valproic acid (see section “Contraindications”).
In children with unexplained gastrointestinal symptoms (anorexia, vomiting, cases of cytolysis), a history of lethargy or coma, with mental retardation or a family history of death of a newborn or child, metabolic studies should be carried out before starting treatment with valproic acid drugs, in particular determination of ammonemia (presence of ammonia and its compounds in the blood) on an empty stomach and after meals (see section “Contraindications”).
Patients with systemic lupus erythematosus
Although immune dysfunction is extremely rare during treatment with valproic acid, the potential benefits of their use must be weighed against the potential risks when administered to patients with systemic lupus erythematosus.
Weight gain
Patients should be warned about the risk of weight gain at the beginning of treatment and the need to take dietary measures to minimize this phenomenon.
Patients with diabetes mellitus
Given the possibility of adverse effects of valproic acid on the pancreas, when using the drug in patients with diabetes mellitus, blood glucose concentrations should be carefully monitored. When testing urine for the presence of ketone bodies in patients with diabetes, it is possible to obtain false-positive results, since valproic acid is excreted partially by the kidneys in the form of ketone bodies.
Patients infected with human immunodeficiency virus (HIV)
in vitro studies
Valproic acid has been found to stimulate HIV replication under certain experimental conditions.
The clinical significance of this fact is unknown. In addition, the significance of data obtained from in vitro
for patients receiving maximally suppressive antiretroviral therapy has not been established. However, these data should be taken into account when interpreting the results of continuous viral load monitoring in HIV-infected patients taking valproic acid.
Patients with existing carnitine palmitoyltransferase (CPT) type II deficiency:
Patients with existing CPT type II deficiency should be warned of the higher risk of developing rhabdomyolysis when taking valproic acid.
Ethanol
: During treatment with valproic acid, ethanol consumption is not recommended.
Other special instructions
The inert matrix of the drug (extended release drug), due to the nature of its excipients, is not absorbed in the gastrointestinal tract; after the release of the active substances, the inert matrix is excreted by the intestines.
Depakine chrono long-acting film-coated tablets 300 mg No. 100
Before starting to use the drug Depakine chrono and periodically during the first 6 months of treatment, especially in patients at risk of developing liver damage, liver function tests should be performed.
As with the use of most antiepileptic drugs, when using valproic acid, a slight increase in the activity of liver enzymes is possible, especially at the beginning of treatment, which occurs without clinical manifestations and is transient. In these patients, a more detailed study of biological parameters, including the prothrombin index, is necessary, and dose adjustment of the drug may be required, and, if necessary, repeated clinical and laboratory examinations.
Before starting therapy or before surgery, as well as in the event of spontaneous occurrence of subcutaneous hematomas or bleeding, it is recommended to determine the bleeding time and the number of formed elements in the peripheral blood, including platelets.
Severe liver damage
Predisposing factors
There have been isolated reports of severe liver damage, sometimes fatal. Clinical experience shows that patients at risk include those taking multiple antiepileptic drugs at the same time, infants and children under three years of age with severe seizures, especially in the presence of brain damage, mental retardation and/or congenital metabolic or degenerative diseases, patients concomitantly taking salicylates (since salicylates are metabolized through the same metabolic pathway as valproic acid).
After the age of three, the risk of liver damage decreases significantly and decreases progressively as the patient ages. In most cases, such liver damage occurred during the first 6 months of treatment, most often between 2 and 12 weeks of treatment and usually when valproic acid was used as part of combination antiepileptic therapy.
Symptoms suspicious for liver damage
For early diagnosis of liver damage, clinical observation of patients is mandatory. In particular, you should pay attention to the appearance of the following symptoms, which may precede the onset of jaundice, especially in patients at risk (see above):
- nonspecific symptoms, especially those that suddenly begin, such as asthenia, anorexia, lethargy, drowsiness, which are sometimes accompanied by repeated vomiting and abdominal pain,
- resumption of seizures in patients with epilepsy.
Patients or their family members (when using the drug in children) should be warned that they should immediately report the occurrence of any of these symptoms to their doctor. Patients should immediately undergo clinical examination and laboratory testing of liver function tests.
Revealing
Liver function tests should be performed before starting treatment and then periodically during the first 6 months of treatment. Among conventional studies, the most informative are studies reflecting the state of the protein-synthetic function of the liver, especially the determination of the prothrombin index. Confirmation of a deviation from the norm of the prothrombin index in the direction of its decrease, especially in combination with deviations from the norm of other laboratory parameters (a significant decrease in the content of fibrinogen and blood coagulation factors, an increase in the concentration of bilirubin and an increase in the activity of liver transaminases), as well as the appearance of other symptoms indicating damage liver (see above), requires discontinuation of the drug Depakine Chrono. As a precaution, if patients were taking salicylates concomitantly, their use should also be discontinued.
Pancreatitis
There are rare reported cases of severe forms of pancreatitis in children and adults, which developed regardless of age and duration of treatment. Several cases of hemorrhagic pancreatitis have been observed with rapid progression of the disease from the first symptoms to death.
Children are at increased risk of developing pancreatitis, and this risk decreases as the child ages. Risk factors for developing pancreatitis may include severe seizures, neurological disorders, or anticonvulsant therapy. Liver failure combined with pancreatitis increases the risk of death.
Patients who experience severe abdominal pain, nausea, vomiting and/or anorexia should be evaluated immediately. If the diagnosis of pancreatitis is confirmed, in particular with increased activity of pancreatic enzymes in the blood, the use of valproic acid should be discontinued and appropriate treatment should be initiated.
Female children and adolescents, women of childbearing potential and pregnant women
Depakine Chrono should not be used in female children and adolescents, women of childbearing potential and pregnant women, unless alternative treatments are ineffective or not tolerated. This limitation is associated with a high risk of teratogenicity and mental and physical development disorders in children who were exposed to valproic acid in utero. The benefit/risk ratio should be carefully re-evaluated in the following cases: during regular review of treatment, when a girl reaches puberty and, urgently, if a woman taking valnroic acid plans or becomes pregnant.
During treatment with valproic acid, women of childbearing potential should use reliable methods of contraception, and they should be informed of the risks associated with taking Depakine Chrono during pregnancy (see section Use during pregnancy and breastfeeding). To help the patient understand these risks, the physician prescribing valproic acid should provide the patient with comprehensive information about the risks associated with taking Depakine Chrono during pregnancy.
In particular, the physician prescribing valproic acid should ensure that the patient understands:
- the nature and magnitude of the risks when using valproic acid during pregnancy, in particular, the risks of teratogenic effects, as well as the risks of disorders of the mental and physical development of the child,
- the need to use effective contraception,
- the need for regular review of treatment,
- the need for urgent consultation with her doctor if she suspects that she is pregnant, or when she suspects the possibility of pregnancy.
A woman planning a pregnancy should definitely try, if possible, to switch to an alternative treatment before she attempts to conceive (see section Use during pregnancy and breastfeeding). Treatment with valproic acid should be continued only after a physician experienced in the treatment of epilepsy and bipolar disorders has re-evaluated the benefits and risks of treatment.
Suicidal thoughts and attempts
Suicidal thoughts and attempts have been reported in patients taking antiepileptic drugs for some indications. A meta-analysis of randomized placebo-controlled trials of antiepileptic drugs also showed a 0.19% increase in the risk of suicidal ideation and attempts in all patients taking antiepileptic drugs (including a 0.24% increase in this risk in patients taking antiepileptic drugs for epilepsy ), compared with their frequency in patients taking placebo. The mechanism of this effect is unknown.
Therefore, patients taking the drug Depakine Chrono should be constantly monitored for suicidal thoughts and attempts, as well. if they occur, appropriate treatment must be carried out. Patients and caregivers are advised to seek immediate medical attention if a patient experiences suicidal thoughts or attempts.
Carbapenems
The simultaneous use of carbapenems is not recommended (see section Interactions with other drugs).
Patients with known or suspected mitochondrial diseases
Valproic acid can initiate or aggravate the manifestations of the patient's mitochondrial diseases caused by mutations in mitochondrial DNA, as well as in the nuclear gene encoding the mitochondrial enzyme polymerase (POLG). In particular, in patients with congenital neurometabolic syndromes caused by mutations in the gene encoding β-polymerase (POLG), such as patients with Alpers-Huttenlocher syndrome, valproic acid was associated with a higher incidence of acute liver failure and liver-related deaths. Diseases due to β-polymerase defects may be suspected in patients with a family history of such diseases or symptoms suggestive of their presence, including unexplained encephalopathy, refractory epilepsy (focal, myoclonic), status epilepticus, mental and physical retardation, psychomotor regression, axonal sensorimotor neuropathy, myopathy, cerebellar ataxia, ophthalmoplegia or complicated migraine with visual (occipital) aura and others.
In accordance with current clinical practice, testing for mutations in the polymerase β gene (POLG) should be performed to diagnose such diseases (see section Contraindications).
Increased seizures
As with other antiepileptic drugs, when taking valproic acid, some patients experienced, instead of improvement, a reversible increase in the frequency and severity of seizures (including the development of status epilepticus) or the appearance of new types of seizures. If seizures worsen, patients should immediately consult their doctor (see Side Effects section).
Children (information refers to dosage forms of the drug Depakine that can be taken by children under three years of age)
In children under three years of age, if it is necessary to use the drug, it is recommended to use it in monotherapy and in the dosage form recommended for children. However, before starting treatment, you should weigh the ratio of the potential benefits of using valproic acid and the risk of liver damage and the development of pancreatitis when using it.
In children under 3 years of age, the simultaneous use of valproic acid and salicylates should be avoided due to the risk of liver toxicity.
Kidney failure
It may be necessary to reduce the dose of valproic acid due to an increase in the concentration of its free fraction in the blood serum. If it is impossible to monitor plasma concentrations of valproic acid, the dose of the drug should be adjusted based on clinical observation of the patient.
Enzyme deficiency of the carbamide cycle (urea cycle)
If an enzymatic deficiency of the carbamide cycle is suspected, the use of valproic acid is contraindicated. Several cases of hyperammonemia with stupor or coma have been described in such patients. In these cases, metabolic studies should be performed before starting treatment with valproic acid (see section Contraindications).
In children with unexplained gastrointestinal symptoms (anorexia, vomiting, cases of cytolysis), a history of lethargy or coma, with mental retardation, or a family history of death of a newborn or child, metabolic studies should be carried out before starting treatment with valproic acid, in particular, determination of ammonemia (presence of ammonia and its compounds in the blood) on an empty stomach and after meals (see section Contraindications).
Patients with systemic lupus erythematosus
Although it has been shown that during treatment with Depakine Chrono, dysfunction of the immune system is extremely rare, the potential benefits of its use must be compared with the potential risks when using the drug in patients with systemic lupus erythematosus.
Weight gain
Patients should be warned about the risk of weight gain at the beginning of treatment, and measures, mainly dietary, should be taken to minimize this phenomenon.
Patients with diabetes mellitus
Given the possibility of adverse effects of valproic acid on the pancreas, when using the drug in patients with diabetes mellitus, blood glucose concentrations should be carefully monitored. When testing urine for the presence of ketone bodies in patients with diabetes, it is possible to obtain false-positive results, since valproic acid is excreted by the kidneys, partly in the form of ketone bodies.
Patients infected with human immunodeficiency virus (HIV)
In in vitro
Valproic acid has been found to stimulate HIV replication under certain experimental conditions.
The clinical significance of this fact, if any, is unknown. Additionally, the significance of these in vitro
for patients receiving maximally suppressive antiretroviral therapy has not been established. However, these data should be taken into account when interpreting the results of continuous viral load monitoring in HIV-infected patients taking valproic acid.
Patients with existing deficiency of carnitine palmitoyltransferase (CPT) tin II
Patients with existing CPT type II deficiency should be warned of the increased risk of rhabdomyolysis when taking valproic acid.
Ethanol
During treatment with valproic acid, ethanol consumption is not recommended.
Other special instructions
The inert matrix of the drug Depakine Chrono (extended release drug), due to the nature of its excipients, is not absorbed in the gastrointestinal tract; after the release of the active substances, the inert matrix is excreted in the feces.
One tablet of Depakine Chrono 300 mg contains 1.2 mmol (27.6 mg) sodium. One tablet of Depakine Chrono 500 mg contains 2 mmol (46.1 mg) sodium. This must be taken into account in patients on a strict low sodium diet.
Depakine syrup 57.64 mg/ml 150 ml bottle No. 1 ➤ instructions for use
Pregnancy: Based on experience in treating mothers with epilepsy, the risks associated with the use of valproate during pregnancy are described as follows:
Risk associated with epilepsy and antiepileptic drugs.
It has been shown that when using any antiepileptic drugs in women with epilepsy, the overall incidence of congenital defects in children born to them is 2-3 times higher than among the general population (about 3%). Although an increased number of children with congenital defects has been noted in the case of combination drug therapy, the respective role of the disease itself and the drugs taken by the mother has not yet been formally established. The most common malformations are cleft lip and malformations of the cardiovascular system. Sudden interruption of antiepileptic treatment may worsen the course of the mother's illness and lead to detrimental consequences for the fetus.
Risk associated with sodium valproate
The overall risk of malformations in women when taking valproate in the first trimester of pregnancy is no higher than when taking other antiepileptic drugs. Cases of facial dysmorphia have been described. Rare cases of multiple malformations, especially of the limbs, have been observed. The frequency of such effects has not yet been precisely established. Along with this, sodium valproate predominantly causes disruption of the development of the neural tube: myelomeningocele, spina bifida... The frequency of such complications is 1-2%.
In light of this data:
If a woman is planning a pregnancy, the indications for antiepileptic treatment should be reconsidered; It is recommended to consider the issue of additional administration of folates. During pregnancy, antiepileptic treatment with valproate should not be interrupted if it is effective. In such cases, monotherapy is recommended, the minimum effective daily dose of which should be divided into several doses per day. However, the patient should be referred for specific prenatal evaluation to identify any anomalies of the neural tube or other defects.
Risk to the newborn
Isolated cases of hemorrhagic syndrome have been described in newborns whose mothers took sodium valproate during pregnancy. This hemorrhagic syndrome is associated with hypofibrinogenemia; Afibrinogenemia, which can be fatal, has also been described. This hypofibrinogenemia is possibly due to a decrease in clotting factors. However, this syndrome must be distinguished from the decrease in vitamin K-dependent factors caused by phenobarbital and other enzyme inducers. Therefore, in newborns, platelet count, plasma fibrinogen levels, coagulation tests and determination of coagulation factors should be performed.
Lactation Excretion of valproate into milk is low and ranges from 1 to 10% of serum levels. Until now, we have monitored infants who received breast milk and did not develop any clinical manifestations during the neonatal period. Impact on the ability to drive and perform work requiring increased attention The patient should be warned about the danger of drowsiness, especially in the case of anticonvulsant polytherapy or combination with benzodiazepines. Interaction with other drugs
Neuroleptics, MAO inhibitors, antidepressants and benzodiazepines
Depakine® can potentiate the effect of other psychotropic drugs - antipsychotics, MAO inhibitors, antidepressants and benzodiazepines. Therefore, clinical monitoring and, if necessary, dose adjustment are recommended.
Phenobarbital
Depakine® increases the plasma concentration of phenobarbital (due to inhibition of hepatic catabolism) and signs of sedation may appear, especially in children. Therefore, clinical monitoring is recommended during the first 15 days of combination treatment, with immediate reduction of the phenobarbital dose if signs of sedation occur and determination of phenobarbital blood levels, if necessary.
Primidon
Depakine® increases the concentration of primidone with an increase in its side effects (for example, sedation); these phenomena cease with long-term treatment. Clinical monitoring is recommended, especially at the start of combination treatment, with dose adjustment if necessary.
Phenytoin
Depakine® reduces the concentration of phenytoin in plasma. Moreover, Depakine® increases the amount of free form of phenytoin with the possible appearance of signs of overdose (valproic acid replaces phenytoin in its binding to plasma proteins and reduces its catabolism in the liver). Therefore, clinical monitoring is recommended and free forms should be assessed when determining plasma levels of phenytoin.
Carbamazepine
Valproate may potentiate the toxic effects of carbamazepine. Clinical monitoring is recommended, especially at the beginning of combination therapy and, if necessary, dosage adjustment.
Lamotrigine
Valproate may slow the metabolism of lamotrigine and increase its elimination half-life; dosages should be adjusted if possible (reducing the dose of lamotrigine). There are suggestions, still awaiting proof, that the risk of rash increases when lamotrigine and valproic acid are used together.
Zidovudine
Valproate may increase plasma concentrations of zidovudine, resulting in increased zidovudine toxicity.
Antiepileptic drugs with an enzyme-inducing effect (phenytoin, phenobarbital, carbamazepine) reduce the concentration of valproate in the serum. If combination therapy is used, doses should be adjusted depending on the level of the drug in the blood. On the other hand, the combination of felbamate and valproate may increase serum concentrations of valproate. The dosage of valproate should be monitored. Mefloquine increases the metabolism of valproic acid and may cause convulsions. Therefore, during combination therapy, epileptic seizures may occur. In the case of simultaneous use of valproate and drugs that bind tightly to proteins (aspirin), the concentration of free valproate in the serum may increase. Careful monitoring of the prothrombin index should be carried out in case of simultaneous use of vitamin K-dependent anticoagulants. Serum levels of free valproate may increase (as a result of decreased hepatic metabolism) when administered concomitantly with cimetidine or erythromycin.
Other types of interaction
Valproate generally does not have an enzyme-inducing effect; as a result, valproate does not reduce the effectiveness of estroprogestogen drugs for women using hormonal contraceptives.