Forms of pharyngitis
According to its clinical course, pharyngitis can be chronic and acute.
The chronic form is divided into:
- hypertrophic – this is an increase in mucous membrane;
- atrophic – this is the depletion of the mucous membrane;
- catarrhal – standard inflammation.
The acute form also exists in three types:
- allergic – provoked by allergens;
- infectious – caused by pathogenic microorganisms;
- post-traumatic – occurs due to contact with the mucous membrane of irritating substances.
When are antibiotics needed?
If, after the results of a pharyngeal smear are obtained, it is determined that the disease is bacterial in nature, antibiotic drugs are prescribed. Antibiotics for pharyngitis can be prescribed for local (local) or general action. The choice of a specific drug depends on the patient’s condition and his individual characteristics. Thus, during pregnancy, a woman (if antibiotics cannot be avoided) is prescribed mainly local drugs for irrigating the pharynx, since they penetrate into the systemic bloodstream to a lesser extent.
The use of antibiotics is required in order to stop the proliferation of the pathogen and destroy it. Thanks to this, drugs in this category help prevent the spread of the inflammatory process to surrounding tissues. In the first days of taking antibiotics, an increase in temperature is the norm, since due to the large number of dead pathogens, the body becomes intoxicated. The duration of taking antibiotics is at least 5 days. If you stop the course earlier, bacteria resistant to the drug will form, which will make its use ineffective. Each specific drug has its own contraindications, which must be taken into account when prescribing the drug.
Side effects from taking general antibiotics may include:
- fever;
- joint pain;
- disturbances in intestinal function;
- general weakness.
Such manifestations are considered normal and, as a rule, do not require replacement of the drug. However, if they develop, you must inform your doctor about this.
For pharyngitis, penicillin drugs or cephalosparins are most often used. If they are not tolerated by the patient, treatment is carried out using Azithromycin, Amoxiclav, Lincomycin, Erythromycin or Amoxicillin. Antibiotics for pharyngitis in adults and children are prescribed the same.
In the chronic form of the disease, pharyngitis without antibiotics is treated only until it worsens. If this occurs, antibiotics are prescribed.
Reasons for the development of the disease
In most cases, acute pharyngitis does not act as an independent pathology, but is only a manifestation of a general infectious process. Many infections (diphtheria, scarlet fever, measles, influenza) debut as an acute form of pharyngitis and are therefore not diagnosed in a timely manner.
In 70% of cases, acute inflammation of the pharynx is caused not by bacteria, but by viruses. Most often this is:
- influenza and parainfluenza viruses;
- rhinoviruses;
- adenoviruses;
- Epstein-Bar viruses;
- cytomegalovirus family;
- enteroviruses.
Only 30% of cases of acute pharyngitis are caused by bacterial flora:
- staphylococci;
- pneumococci;
- streptococci of groups A, C, G;
- Corynebacterium diphtheria;
- hemophilus influenzae;
- atypical pathogens are chlamydia and mycoplasma.
The latter are called atypical, because settle inside cells, and not on the surface of the mucosa, so the immune system cannot detect them. For this reason, such inflammatory processes take a long time, creating significant difficulties in carrying out etiotropic (acting on the cause) therapy.
In a small percentage of cases, pharyngitis is caused by fungal flora. As a rule, this is due to a general weakening of the immune system or local immunodeficiency (for example, in smokers). This is also facilitated by long-term use of antibacterial drugs.
If not treated correctly, acute pharyngitis can become chronic. Most often, pharyngitis caused by cytomegalovirus infection, Epstein-Barr virus, chlamydial and mycoplasma infection is chronic, since these microorganisms live inside cells and are not affected by local antibacterial and antiviral therapy. But inflammation caused by streptococci and staphylococci can also become chronic.
The development of chronic pharyngitis is a consequence of one of two processes:
- chronicity of acute inflammation of the pharynx due to poor immune defense;
- secondary infection of the pharynx from infectious foci located in the body (carious teeth, inflammation of the ENT organs, diseases of the digestive tract, etc.).
Factors that increase the likelihood of pharyngitis:
- hypothermia of the whole body or only the upper respiratory tract;
- alcohol abuse;
- eating sour, spicy, hot or cold foods;
- nasal breathing disorder.
Breathing through the nose becomes difficult in conditions such as:
- deviated nasal septum;
- nasal polyps;
- hypertrophy of the inferior turbinates;
- allergic rhinitis.
In these cases, a person has to breathe through his mouth, and this dries out the oral mucosa and reduces local immunity, because The production of immunoglobulin A decreases.
Atrophic pharyngitis is also provoked by other causative factors:
- lack of vitamins;
- anemia;
- functional heart failure;
- renal failure;
- diabetes;
- decreased thyroid function (hypothyroidism);
- menopausal syndrome.
Complication
Possible complications of chronic pharyngitis are:
- Peritonsillar abscess is a purulent inflammation that develops due to bacterial pharyngitis caused by streptococcal infection.
- A retropharyngeal abscess is a purulent inflammation of the tissue located in the retropharyngeal space.
- Laryngitis is an inflammatory process affecting the mucous membrane of the larynx.
- Chronic bronchitis develops when the infection descends lower into the bronchi and causes inflammation in them.
- Systemic inflammatory diseases (glomerulonephritis, myocarditis, rheumatism) - chronic inflammation of the pharynx can cause complications on the kidneys, heart and joints.
- Atrophic processes of the pharyngeal mucosa. The most dangerous consequence of this condition is the development of oncological processes in the pharynx.
Clinical picture
The acute form manifests itself:
- sore throat, which sometimes radiates to the ears if the lateral pharyngeal ridges become inflamed;
- a feeling of tickling and burning;
- dryness and discomfort in the throat;
- slight rise in temperature (usually no more than 38.0°C).
When palpating the lymph nodes of the neck, they are determined to be enlarged and painful. Examination of the pharynx reveals redness of its posterior wall and palatine arches, granularity is clearly visible (enlarged lymphoid foci of a brighter color than the surrounding mucosa). An important differential sign is the absence of inflammation in the tonsils with pharyngitis. This distinguishes it from a sore throat.
Chronic inflammatory lesions of the pharynx are easier than acute ones - fever and general deterioration in health are almost always absent. Usually the patient is concerned about:
- feeling of dryness and sore throat;
- dry cough with attacks;
- sensation of a lump or foreign body in the throat.
Due to the fact that mucous secretion accumulates on the back wall, a person constantly needs to swallow it. This causes significant discomfort.
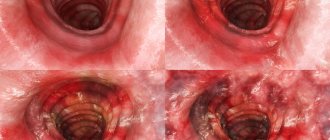
The atrophic type of pharyngitis is accompanied by thinning and dryness of the mucous membrane, through which the vessels are visible. On its surface there may be crusts of dried mucous secretion.
The hypertrophic form is diagnosed by the presence of overgrown foci of lymphoid tissue, which are determined in the form of granules or strands. They are located behind the lateral pharyngeal ridges (these are the posterior arches of the palate). During an exacerbation, hyperplastic areas swell, increase in size, acquire a bright pink color, and foci of abscess formation may appear in them.
Introduction
Chronic pharyngitis is a prolonged inflammatory process of the mucous membrane of the back wall of the pharynx. This is a longer lasting inflammation than acute pharyngitis. Chronic pharyngitis manifests itself in a series of relapses - during an exacerbation, the symptoms return again, and after some time they fade again. Such inflammation can last for years, greatly reducing the patient’s quality of life. Another unpleasant point is the risk of complications: it always persists as long as there is a chronic source of infection in the throat.
Most often, chronic pharyngitis develops due to untreated acute pharyngitis. Also at risk are people whose pharynx is exposed to the negative effects of external factors:
- smoking,
- abuse of alcoholic beverages;
- polluted air in the place of residence;
- inhalation of harmful substances, dusty, polluted air in production.
The main signs of chronic pharyngitis are dryness, soreness and discomfort in the throat.
The disease can manifest itself in several forms. Pharyngitis can develop as an independent disease, or can be combined with chronic tonsillitis. This combination of two ENT conditions is called tonsillopharyngitis.
Diagnosis of pharyngitis
In the diagnosis of acute pharyngitis, pharyngoscopy, determination of the pathogen (PCR, bacteriological and mycological examination of smears from the pharyngeal mucosa) and laboratory examination (clinical blood test, inflammatory markers, general urine analysis) are of key importance. The data obtained during diagnosis allows you to select the correct treatment, avoid complications and chronicity of the process.
In the diagnosis of chronic pharyngitis, the search for primary foci of infection is important. For this purpose the following is carried out:
- X-ray examination of the nasal cavity, paranasal sinuses and oral cavity (computed tomography of the paranasal sinuses, dental CT);
- endoscopic examination of the nasopharynx;
- esophagogastroduodenoscopy.
A detailed laboratory examination is carried out. In addition to a clinical blood test, it is necessary to conduct an examination for chronic viral infections and intracellular bacterial infections, and exclude the allergenic factor.
In some cases, a detailed examination of the immune system is required, since a decrease in local immunity leads to chronic infection.
Where to treat chronic pharyngitis in Moscow?
Treatment of chronic pharyngitis in Moscow is carried out in various medical institutions, ranging from district clinics to large multidisciplinary network clinics. The cost of treatment and the quality of services in this case cannot be the same everywhere.
The most affordable way to treat the disease is to enroll in a clinic at your place of residence. Affordable, but not the simplest or most effective. As a rule, in district clinics, appointments with an otorhinolaryngologist are quite dense, and it is very difficult to get a ticket “here and now.” You will have to wait about two weeks for an appointment (during this time, the exacerbation of chronic pharyngitis will only gain momentum), or try to get through the “live” queue, sitting all day at the ENT doctor’s office. By the way, it is not always possible to do this the first time.
Now about the quality of treatment - the doctor in the clinic has the task of accepting as many patients as possible. Everything is logical: there are many patients, one doctor. This means that the consultation time is very limited in time. But in the 10 minutes allocated for each patient, it is impossible to fully collect anamnesis and conduct an examination, let alone give effective prescriptions and carry out therapeutic manipulations. Another problem of district clinics is the lack of sophisticated, modern equipment, so the choice of treatment procedures used by the doctor is very limited. Treatment often comes down to prescribing medications that only relieve symptoms for a short time. Treatment for chronic pharyngitis can be very long and tedious.
Many patients are treated in multidisciplinary network clinics, with which they have an agreement to provide treatment under the VHI policy. In such clinics, the treatment process itself often becomes a secondary issue. It takes a doctor a lot of time to fill out medical documentation correctly, because filling it out incorrectly can lead to problems with the insurance company. Therefore, an impressive part of the reception is spent on “paper” work. Another drawback of such clinics, which patients often complain about, is the appointment of unnecessary procedures and unnecessary consultations. Network clinics need a constant flow of patients: the more people come, the more doctors or services they visit, the better. The quality of treatment under such conditions fades into the background.
The third option is treatment in highly specialized private clinics that deal with one particular medical area. Insurance companies are not interested in such clinics, so there will be no flow of people here. Highly specialized clinics, as a rule, are well equipped with medical equipment, which allows high-quality diagnostics and treatment to be carried out in one place. For the treatment of chronic pharyngitis, which requires increased attention and experience of an ENT doctor, this option is the most acceptable.
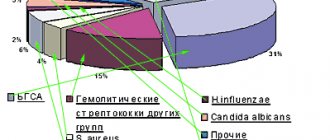
Etiology of inflammatory pathology of the pharynx.
In our country, it is customary to separate tonsillitis and pharyngitis as diseases that have a similar etiopathogenesis, but differ significantly in clinical picture and severity [1, 2]. According to the etiological factor, acute pharyngitis can be divided into viral, bacterial, fungal, allergic, traumatic (due to foreign body entry or surgical intervention, exposure to hot liquid or steam, acids, alkalis, radiation, etc.) [3].
In approximately 90% of cases, the causative agents of tonsillitis and pharyngitis (tonsillopharyngitis) are viruses [4]. Viral infection, in particular the Epstein-Barr virus (HHV-4), herpes virus type VI, plays a special role in the chronicization of inflammatory processes in the pharynx [5]. Other members of the family Herpesviridae
(HSV-1, HSV-2, CMV) initiate acute inflammation of the pharyngeal mucosa [6].
In bacterial inflammation of the pharynx, Streptococcus α-haemolyticus, β-haemolyticus, 0x9A;-haemolyticus, Staphylococcus aureus, CNS Staphylococcus, Neisseria spp., Haemophilus spp., Corynebacterium spp.,
as well as fungi of the genus
Candida,
filamentous fungi [5]. Irrational antibiotic therapy, including local, leads to persistent dysbiotic changes in the oropharynx and the development of antibiotic resistance. When examining patients with a long and persistent history of the disease, the fungal nature of inflammation is detected in 44.7% of patients [6]. In 90% of cases, the bacterial flora of the pharynx is represented by associations of 2-3 types of microbes [7].
Much less common are group C and G streptococci, Arcanobacterium haemolyticum, Neisseria gonorrhoeae, Corynebacterium diphtheria
(diphtheria), anaerobes and spirochetes (Simanovsky-Plaut-Vincent angina), extremely rarely - mycoplasma and chlamydia.
In accordance with the International Classification of Diseases, X revision, “Streptococcal pharyngitis” (J02.0) and “Streptococcal tonsillitis” (J03.0) are classified as a separate disease [8]. In the vast majority of cases, tonsillitis occurs in the palatine tonsils, while other tonsils are involved in the inflammatory process much less frequently. Therefore, in medical practice, the term “angina” usually means inflammation of the tonsils. Most tonsillitis is an exacerbation of chronic tonsillitis [4]. In the Russian Federation, since 1994, compared with previous years, there has been an increase in the primary incidence (detection) of acute rheumatic fever from 0.06 to 0.16 among children and from 0.08 to 0.17 among adolescents, which is mainly due to with the inattentive attitude of doctors to the treatment of such a disease as chronic tonsillitis.
The “gold standard” for determining β-hemolytic streptococcus in the oral cavity for the purpose of prescribing antibacterial therapy is streptatest. The sensitivity of this test is, according to multicenter clinical studies, 97.3%, and the specificity is 95.3% [10]. Modern test systems make it possible to obtain results in 15-20 minutes with high specificity (95-100%), but with less sensitivity than with cultural testing (60-95%). Express methods complement, but do not replace, the cultural method. In addition, only by isolating the pathogen can its sensitivity to antibiotics be determined [11, 12].
Clinical picture.
The clinical picture of pharyngitis and tonsillitis is characterized by soreness, dryness, discomfort and pain in the throat, in an acute condition - general malaise, fever, the pharyngoscopic picture is characterized by hyperemia of the mucous membrane [13]. Perhaps the pain syndrome is the most unpleasant for the patient.
The mucous membrane of the pharynx has rich innervation; there are a large number of pain, chemo-, mechano- and proprioceptors. The pharynx is innervated from the pharyngeal plexus, located on the outer surface of the middle pharyngeal sphincter under the buccal-pharyngeal fascia. The plexus is formed by the branches of the glossopharyngeal and vagus nerves, as well as sympathetic fibers of the superior cervical ganglion. Sensitive innervation of the pharynx is mainly carried out by the glossopharyngeal nerve, which has anastomoses with the second branch of the trigeminal nerve in the region of the pharyngeal openings of the auditory tubes, as well as by the superior laryngeal nerve - a branch of the vagus nerve. Sore throat is one of the most common reasons for self-medication and emergency department visits. On average, every adult experiences a sore throat approximately 2-3 times a year [14]. Discomfort in the throat is often associated with the forced need to constantly swallow mucus in the back of the throat, which makes patients irritable, interferes with their usual activities and disrupts sleep [13].
According to numerous multicenter studies, antibiotics
reduce the duration of tonsillopharyngitis symptoms by less than 1 day. Moreover, the likelihood of returning to a medical facility for pharyngitis is higher among people who received antibiotics than among those who did not take them. It should be remembered that antibacterial drugs are a potentially toxic pharmacological group and cause up to 25-30% of all side effects of drugs. Thus, systemic antibacterial therapy is indicated only for confirmed bacterial etiology of tonsillopharyngitis.
Currently, the absolute indication for systemic antibacterial therapy is only streptococcal tonsillitis or pharyngitis. This indication is based on the results of controlled studies published back in 1950, which established that achieving eradication of GABHS in recurrent tonsillitis and pharyngitis can significantly reduce the number of recurrent episodes of the disease. Subsequent studies have found that a 10-day course of oral antibiotic therapy is optimal for achieving complete eradication of GABHS.
In addition, when carrying out antibacterial therapy for acute streptococcal tonsillitis, it is necessary to keep in mind the following:
— Although GABHS itself is not capable of producing β-lactamases and still remains sensitive to penicillin, co-pathogens that produce β-lactamases may be present in the oropharynx; in such cases, a course of treatment with protected antibacterial drugs is recommended.
— Possible intracellular localization of GABHS. Although GABHS are considered extracellular pathogens, recent studies have demonstrated that these microorganisms can penetrate the epithelial cells of the human respiratory tract, where they are protected from the action of most antibiotics.
— Low patient performance. There is evidence that by the 9th day of standard penicillin therapy, only 8% of patients continue treatment. This may be due to the fact that already on the 2-3rd day from the start of therapy, as a rule, a pronounced clinical improvement occurs.
With viral tonsillopharyngitis, there is a need to use a local drug, the use of which is acceptable for inflammatory pathologies of the pharynx of various etiologies.
The main drugs that are used for local treatment of pharyngitis can be divided into 6 groups: antibiotics, antiseptics, antimycotics, immunocorrectors, anesthetic and anti-inflammatory and homeopathic drugs. As you know, an antibiotic destroys bacterial flora. But nature abhors a vacuum, and fungal flora takes the place of the bacterial flora, especially against the background of a reduced immune response. In this regard, the prescription of antiseptics, i.e. drugs that also act on fungal flora can solve this problem. However, the abuse of antiseptics, in turn, leads to the death of the surface layer of the epithelium lining the pharynx, which increases the patient’s discomfort.
The composition of drugs for local treatment of inflammatory pathology of the pharynx includes one or more antiseptics (chlorhexidine, hexetidine, benzydamine, ambazone, thymol and its derivatives, alcohols, iodine preparations, etc.), essential oils, local anesthetics (lidocaine, tetracaine, menthol) , less often - antibiotics (fusafyungin, framycetin) or sulfonamides, deodorizing agents. Preparations may also contain bacterial lysates, natural antiseptics (plant extracts, bee products), synthesized factors of nonspecific protection of mucous membranes, which also have an antiviral effect (lysozyme, interferon), vitamins (ascorbic acid). Antimicrobial drugs can be prescribed in the form of rinses, insufflations, inhalations, as well as tablets and lozenges.
The main requirements for drugs applied to the mucous membrane are:
- a wide spectrum of antimicrobial action, preferably including antiviral and antibacterial activity;
- lack of toxic effect and low rate of absorption from mucous membranes;
- low allergenicity; no irritating effect on the mucous membrane.
Most drugs (Hexalize, Drill, Septolete, Faringosept, Neo-angin, Strepsils, etc.) for the treatment of pharyngitis are available in the form of tablets, lozenges or lozenges. They are easy to use, but usually contain antiseptics. The doctor should remember the toxicity of chlorhexidine, which is part of many drugs with an antiseptic effect (antiangin, drill, sebidine, eludril), and should not allow their unlimited, uncontrolled use by patients (especially children).
The prescription of a number of drugs is limited by their high allergenicity and irritating effect. This includes drugs containing iodine derivatives (iodinol, iox, vocadine, povidone-iodine), propolis (proposol), sulfonamides (bicarmint, ingalipt). Preparations containing herbal antiseptics and essential oils are effective and harmless, but their use is contraindicated in patients suffering from allergies to pollen, and the number of people with this disease in some geographic areas is up to 20% of the population [13].
As a local therapy for tonsillopharyngitis to suppress pain in the pharynx, it is primarily customary to use non-steroidal anti-inflammatory drugs
(NSAIDs). It is well known that the anti-inflammatory and analgesic effect of the NSAID group is associated with inhibition of the activity of the enzyme cyclooxygenase (COX). There are 2 forms of COX: constitutional (COX-1), as a result of which “homeostatic” prostaglandins (I2, E2, thromboxane A2) are formed and induced (COX-2), which appears only during inflammation and also controls the synthesis of prostaglandins, but “pro-inflammatory” ", supporting inflammation. Inhibition of COX-2 explains the anti-inflammatory and analgesic effects of drugs, while blocking COX-1 creates the preconditions for the occurrence of their side effects.
To avoid the systemic effect of NSAIDs and at the same time ensure direct contact of the drug with the mucous membrane of the oral cavity and pharynx, NSAIDs have been developed in the form of lozenges containing low doses of the active substance in dosage form. An example of such a dosage form is the topical NSAID flurbiprofen for the symptomatic treatment of sore throat, 8.75 mg in the form of strepsilc intensive lozenges. Being an NSAID with pronounced anti-inflammatory activity, strepsil intensive acts on the inflammatory process, regardless of its etiology. According to IMS Health dated March 15, 2013, strepsil intensive is the only drug for sore throat with flurbiprofen circulating in the Russian Federation [15].
To compare the effectiveness of the most popular local drugs used for diseases of the pharynx, clinical local symptoms, symptoms of intoxication, and pharyngoscopic signs were analyzed on a 4-point scale; the dynamics of pain severity was assessed on a 10-point visual analogue scale over 10 days. The study found that Strepsils intensive lozenges have a rapid onset of action, significantly reduce the severity of pain within 15 minutes, and after complete dissolution of the tablet, provide the patient with pain relief for at least 90 minutes. Thus, the effectiveness of strepsil intensive lozenges was significantly higher compared to other drugs [16].
The main advantages of the drug Strepsils intensive are:
— a unique formula with an optimal dose of flurbiprofen for topical use of 8.75 mg;
- rapid action (onset of action - after 2 minutes, pronounced analgesic effect - after 15 minutes), duration - more than 3 hours;
- reduction of swelling of the pharyngeal tissues and easier swallowing for up to 4-6 hours;
- convenient tablet form for lozenges.
The drug should be used in adults and children over 12 years of age, 1 lozenge every 2-3 hours until pain is relieved. The maximum daily dose is 5 tablets. They must be absorbed until completely dissolved. To avoid the accumulation of side effects, you should not use Strepsils intensive for more than 3 days.
Thus, the use of topical NSAIDs provides a high safety profile for the use of this group of drugs due to the minimal risk of systemic action and a good analgesic effect, realized by eliminating inflammation and swelling in the pharyngeal cavity, which cause pain. Strepsils intensive, having a local analgesic and anti-inflammatory effect, significantly improves the quality of life of patients. The use of a local anti-inflammatory drug is one of the main components of the treatment of inflammatory pathology of the pharynx, regardless of the nature of the disease (bacterial or viral).
Inhalations and rinses
Inhalations for pharyngitis, as well as rinses, help to significantly speed up recovery. An action directly aimed at the inflamed mucosa gives a quick result, especially if the pathology is not advanced.
Inhalations can be carried out using steam using essential oils and medicinal plants or using a nebulizer, which is filled with the necessary medications. In this case, specific medications are prescribed by the doctor. Using a nebulizer, cold inhalations can be carried out with antibiotics, saline (if it is necessary to soften and moisturize mucosal tissue), as well as mucolytics.
Antiseptic agents are used for rinsing. This can be a simple saline solution or decoctions of eucalyptus, sage or calendula. Pharmacy antiseptics are also used, such as hydrogen peroxide, miramistin, furatsilin, propolis tincture and other agents that can destroy pathogenic bacteria without irritating a sore throat.