Bronchial asthma
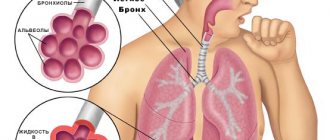
Bronchial asthma is a chronic relapsing disease with predominant damage to the respiratory tract, which is based on chronic allergic inflammation of the bronchi, accompanied by their hyperreactivity and periodic attacks of difficulty breathing or suffocation as a result of widespread bronchial obstruction, which is caused by bronchospasm, hypersecretion of mucus, and swelling of the bronchial wall.
There are two forms of bronchial asthma - immunological and non-immunological - and a number of clinical and pathogenetic variants: atopic, infectious-allergic, autoimmune, dishormonal, neuropsychic, adrenergic imbalance, primary altered bronchial reactivity (including “aspirin” asthma and physical effort asthma ), cholinergic.
Etiology and risk factors for the occurrence of bronchial asthma in children: atopy, bronchial hyperreactivity, heredity. Causes (sensitizing): household allergens (house dust, house dust mites), epidermal allergens of animals, birds, and insects, fungal allergens, pollen allergens, food allergens, drugs, viruses and vaccines, chemicals.
Pathogenesis. The general pathogenetic mechanism is a change in the sensitivity and reactivity of the bronchi, determined by the reaction of bronchial patency in response to the influence of physical and pharmacological factors.
It is believed that in 1/3 of patients (mainly those suffering from the atonic variant of the disease) asthma is of hereditary origin. The most studied allergic mechanisms of asthma are based on IgE- or IgG-mediated reactions. Leukotrienes play a central role in the pathogenesis of aspirin-induced asthma. In physical exertion asthma, the process of heat transfer from the surface of the respiratory tract is disrupted.
Clinic. The disease often begins with a paroxysmal cough, accompanied by shortness of breath with the discharge of a small amount of glassy sputum (asthmatic bronchitis). The full picture of bronchial asthma is characterized by the appearance of mild, moderate or severe attacks of suffocation. An attack may begin with a precursor (profuse discharge of watery secretion from the nose, sneezing, paroxysmal cough, etc.).
An attack of bronchial asthma is characterized by a short inhalation and an extended exhalation, accompanied by wheezing audible from a distance. The chest is in the position of maximum inspiration, the patient takes a forced position, sitting on the bed, dangling his legs down, tilting his torso slightly forward. The muscles of the shoulder girdle, back, and abdominal wall take part in breathing. When percussing over the lungs, a box sound is determined; upon auscultation, many dry rales are heard. The attack often ends with the release of viscous sputum.
Severe prolonged attacks can develop into an asthmatic state - one of the most dangerous options for the course of the disease.
Modern classification of asthma
Thanks to an in-depth study of such a unique disease as bronchial asthma, many classifications of this pathology have been developed over time. For example, according to the International Classification of Diseases, Tenth Revision (ICD-10), the following forms of asthma are distinguished:
- Allergic asthma - in this case, the cause of the development of the disease is mainly allergic processes. As a rule, the allergen can be identified during additional diagnostic studies;
- Non-allergic asthma – the disease is not caused by allergic processes;
- Mixed asthma - in which both allergic and non-allergic irritants are combined;
- Unspecified asthma – the cause of the disease cannot be determined.
After doctors determine the type of asthma, they assess the severity of the patient's condition before starting treatment. For this purpose, classification by severity is used. It is based on four simple indicators:
- Frequency of daily exacerbation symptoms per day and per week;
- Frequency of nocturnal exacerbation symptoms per week;
- The impact of an exacerbation on the patient’s quality of life;
- The value of external respiration indicators (PSV and FEV1).
Bronchial asthma occurs in two stages.
The first stage, when symptoms appear from time to time, is called intermittent (episodic) asthma. The second stage, when symptoms are present for a long time or constantly, is called persistent (permanent) asthma. Depending on the severity of symptoms, this stage has three degrees of severity: mild, moderate and severe. Intermittent (episodic) asthma is characterized by short-term episodes of asthma attack, less than once a week. At night, attacks occur no more than twice a month (for at least three months). PEF and FEV1 > 80% of predicted value. Fluctuations in PEF during the day are less than 20%.
Persistent asthma (mild) is characterized by exacerbation of daytime and nighttime attacks (2 times a week). These episodes cause disturbances in sleep and activity. PEF corresponds to 60-80% of the predicted value. Fluctuations in PSV during the day are 20-30%.
Persistent asthma (moderate severity) is characterized by daily attacks of asthma. Nighttime symptoms occur once a week. These exacerbations gradually lead to limited physical activity and sleep disturbances. The patient requires daily use of inhaled medications (short-acting beta2-agonists). PSV - 60-80% of the required indicators. The daily fluctuation of the PSV value is more than 30%.
The persistent form (severe) is characterized by frequent nocturnal attacks, exacerbations, and a sharp limitation of physical activity. PSV
Make an appointment
Treatment of asthma in adults
Pulmonologists at the Yusupov Hospital, when conducting pharmacotherapy for bronchial asthma, direct all efforts to achieving and maintaining clinical control of the disease over a long period.
If current therapy does not provide control of bronchial asthma, increase the volume of therapy until control is achieved. If partial control of bronchial asthma is achieved, the possibility of increasing the volume of therapy is collectively considered. If control of bronchial asthma is maintained within three months of treatment, the volume of maintenance therapy is reduced in order to establish the minimum number of drugs and the lowest doses of drugs that are sufficient to maintain control. For the treatment of bronchial asthma, 2 types of pharmacological agents are used: emergency medications (to relieve bronchospasm) and medications for basic (“maintenance”) therapy. The first group of drugs includes short- and long-acting β2-agonists (fenoterol, salbutamol, formoterol) and inhaled anticholinergic drugs (tiotropium bromide, ipratropium bromide).
For the basic treatment of bronchial asthma, the following drugs are used:
- Inhaled glucocorticosteroids and systemic corticosteroids;
- Combined drugs (long-acting β2-agonists + inhaled glucocorticosteroids);
- Extended-release theophyllines;
- Leukotriene receptor antagonists;
- Antibodies to IGE.
At the beginning of 2015, the drug Salmecort was registered in the Russian Federation.
This is a fixed combination of salmeterol with fluticasone in the form of a metered dose aerosol inhaler. It is used for maintenance therapy of bronchial asthma. Emergency care for an attack of bronchial asthma:
- Reassure the patient;
- Free yourself from restrictive clothing, unbutton your shirt collar;
- Provide access to fresh air;
- Use the patient’s existing pocket inhaler (can be repeated three times with an interval of 20 minutes);
- Give a comfortable sitting position (the patient’s arms should rest on the table or chair rails, elbows spread to the sides).
If there is no effect or the patient’s condition worsens (threat of status asthmaticus), it is necessary to immediately call an ambulance.
Nebulizer therapy
Nebulizer therapy is a modern method of eliminating severe exacerbation of asthma.
The nebulizer operates on the principle of delivering a therapeutic dose of the drug in aerosol form directly into the patient’s bronchi to obtain a rapid clinical effect. The use of this device during exacerbation of asthma allows local administration of high doses of bronchodilators, while the drug is practically not absorbed into the blood and does not have side effects on other organs and systems, as is often the case when taking tablets or using injections. Thus, nebulizer therapy can not only effectively reduce the manifestation of bronchospasm, but also significantly reduce the frequency of systemic side effects of drugs.
Make an appointment
Prevention of asthma
Prevention of bronchial asthma is divided into primary and secondary.
The goal of primary prevention is to prevent the development of sensitization in patients at risk. The risk group for the development of allergic diseases includes people with a hereditary predisposition to atopy. Secondary prevention is carried out in a group of people with established sensitization who do not have asthma symptoms. These include children with atopic dermatitis or allergic rhinitis, with a family history of bronchial asthma. For effective prevention, it is necessary to minimize the harmful effects of external factors, which often cause the development of bronchial asthma in adults:
- Lead a healthy and active lifestyle;
- Avoid contact with allergens (ventilate the room, do wet cleaning, etc.);
- Eat properly.
Complications
The most serious complication of bronchial asthma is the development of status asthmaticus. This is a prolonged attack, characterized by severe obstruction, severe respiratory failure, and impaired bronchial drainage function. During such an attack, the patient’s usual inhaled medications do not help. Only inpatient treatment is required. One of the causes of status asthmaticus may be an overdose of inhaled sympathomimetics or rapid withdrawal of glucocorticoid drugs. There are three stages in the mechanism of formation of this complication of asthma:
- The first stage is similar to a protracted attack (can last more than 12 hours), which is not controlled by conventional inhaled drugs;
- The second stage - at this stage the patient develops tachycardia, lethargy is noted, the skin becomes bluish and becomes covered with sticky sweat. Shortness of breath is significantly pronounced;
- Third stage - at this stage the patient develops a sharp disturbance in the activity of the central nervous system up to coma, which causes death.
Another rather rare complication of asthma is spontaneous pneumothorax. With a long and persistent course of asthma, pulmonary emphysema and cor pulmonale develop, which leads to pulmonary heart failure.
Basic therapy
Today, first-line medications for the preventive treatment of asthma in patients of any age include inhaled glucocorticoid drugs (ICS):
- Beclomethasone dipropionate;
- Flunisolide;
- Fluticasone propionate;
- Triamcinolone acetonide;
- Mometasone furoate.
Experts prescribe this group of medications to almost all patients with asthma, including those with mild severity of the disease.
ICS are the most powerful anti-inflammatory drugs. Having a wide spectrum of action, they exert their effect on both cellular and humoral mechanisms of the development of allergic (immune) inflammation. These drugs are the choice for patients with persistent asthma of any severity. In addition, ICS is prescribed to all patients with bronchial asthma who take short-acting β2-agonists more than once a day.
In second place in basic therapy are cromones (mast cell membrane stabilizers):
- Sodium cromoglycate;
- Undercut.
These drugs belong to the group of inhaled non-steroidal anti-inflammatory drugs.
Used in the treatment of patients with mild persistent asthma. In addition, they can be prescribed for prophylactic purposes to prevent bronchospasm during physical activity, inhalation of cold air, and possible contact with an allergen. Antileukotriene drugs (leukotriene receptor antagonists): zafirlukast, montelukast. These drugs are recommended to be taken mainly by patients with aspirin-induced bronchial asthma, as well as to prevent bronchospasm provoked by allergens and physical activity.
Systemic glucocorticoid drugs:
- Prednisolone;
- Methylprednisolone.
If a patient is diagnosed with severe bronchial asthma, in which high doses of inhaled glucocorticoids in combination with regular use of bronchodilators are ineffective, systemic glucocorticoids are prescribed.
Diagnostics
The diagnosis of bronchial asthma is made by pulmonologists at the Yusupov Hospital based on the following indicators:
- Complaints, medical history and life of the patient;
- Clinical and functional examination with assessment of the reversibility of bronchial obstruction;
- Specific allergy examination (skin tests with allergens and determination of specific immunoglobulin class E in blood serum);
- Exceptions for other diseases.
The following clinical signs increase the likelihood of having bronchial asthma:
- The presence of more than one of the following symptoms: wheezing, shortness of breath, chest tightness and cough, especially when the patient's condition worsens at night and early in the morning;
- The occurrence of symptoms when exposed to cold air and allergens, physical activity, after taking or β-blockers and acetylsalicylic acid;
- A history of atopic diseases, asthma or atopic diseases in relatives;
- Widespread dry wheezing when auscultating;
- Low peak expiratory flow or forced expiratory volume in 1 second that cannot be explained by other reasons;
- An increase in the number of eosinophils in the peripheral blood, unexplained by other reasons.
To establish a diagnosis of bronchial asthma, pulmonologists at the Yusupov Hospital use special diagnostic methods:
- Studies of the ventilation function of the lungs with assessment of the reversibility of bronchial obstruction;
- Detection of increased bronchial reactivity;
- Conducting a specific allergy examination.
When performing spirometry, an important parameter is FEV1 (forced expiratory volume in the first second of the maneuver).
It indicates the degree of bronchial obstruction. In patients with spirometry within normal limits, a methacholine inhalation test is performed. In bronchial asthma, sputum tests reveal eosinophils, Kurshman spirals, and Charcot-Leyden crystals. Eosinophilia is understood as an increase in the number of eosinophils (leukocyte blood cells) of more than 5%. In parallel, the level of IgE in the blood serum increases, which is a specific mediator of allergic inflammation in the human body. When examining sputum under a microscope, one can detect Courshmann spirals (casts of small bronchi) and Charcot-Leyden crystals (shiny, smooth formations formed from the eosinophil enzyme).
All patients with suspected asthma undergo a study of external respiratory function in order to establish the presence, level and degree of obstruction of the tracheobronchial tree. Tests for assessing physical function include:
- Spirometry;
- Pneumotachometry;
- Recording a flow-volume curve.
A decrease in FEV1 of less than 65% of vital capacity and an increase in residual lung volume of more than 25% of vital capacity indicates a serious problem with airway patency.
To establish the reversibility of changes in the respiratory tract, functional tests with bronchodilators are performed. An improvement in spirometry by 25%, as well as complete restoration of bronchial patency after inhalation of these drugs, indicates the reversibility of bronchospasm.
To identify a specific allergen, an allergological study is performed - skin tests with various antigens. Such tests can only be carried out during remission. In the therapy clinic of the Yusupov Hospital, the scope of the planned examination for the patient is determined by a highly qualified specialist.
Make an appointment
Treatment of asthma complications
Since status asthmaticus (AS) is an extremely dangerous complication of asthma, which can potentially threaten the patient’s life, its treatment must be carried out within the walls of a medical institution. The first measure in the treatment of AS is the intravenous administration of large doses of glucocorticoid drugs, in parallel with sympathomimetics and drugs that promote the rapid expansion of spasmodic bronchi. In addition, the patient needs infusion and symptomatic therapy. If it was not possible to stop AS at the first stage, then the patient is transferred to artificial ventilation and undergoes sanative bronchoscopy.
Treatment
Bronchial asthma refers to a certain type of disease that cannot be completely cured, but it can be controlled. Treatment goals set by the doctors at the Yusupov Hospital:
- Achieving and maintaining seizure control;
- Preventing exacerbations;
- Maintaining respiratory function indicators as close to normal levels as possible;
- Elimination of restrictions on the physical activity of patients, including physical education and sports;
- Minimizing side effects and adverse events from the use of medications;
- Preventing the formation of irreversible bronchial obstruction.
Treatment of asthma is based on two stages: symptomatic therapy to provide emergency assistance and preventive or basic treatment to control the course of asthma.
Nutrition for asthma in adults
To prevent recurrence of asthma attacks and alleviate the course of the disease, the patient is recommended to follow a diet. The following are excluded from the diet:
- Seafood;
- Citrus fruits (except lemons);
- Beekeeping products;
- Nuts;
- Chocolate;
- Alcohol and cigarettes;
- Dairy products;
- Baking and white bread.
Meals should be divided into 4-5 small portions, and try to avoid overeating. With the right approach, avoiding contact with allergens and a favorable psycho-emotional environment, the patient can minimize the frequency of asthmatic attacks and improve their general condition.