Proflosin, 30 pcs., 0.4 mg, long-acting enteric capsules
At the first signs of orthostatic hypotension (dizziness, weakness), the patient should be seated or laid down.
Before starting therapy with Proflosin®, the patient should exclude the presence of diseases and conditions that could cause symptoms similar to those of benign prostatic hyperplasia.
Before starting treatment and regularly during therapy, a digital rectal examination and, if necessary, determination of the concentration of prostate specific antigen (PSA) should be performed.
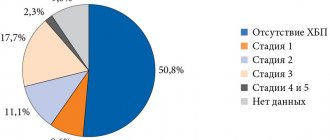
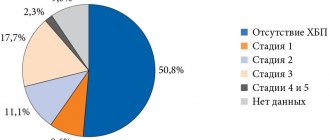
The use of tamsulosin in patients with severe renal impairment (creatinine clearance less than 10 ml/min) requires caution, since no studies have been conducted in this patient population.
During surgical interventions for cataracts or glaucoma while taking the drug or with its previous use, some patients may develop intraoperative instability syndrome of the iris (narrow pupil syndrome), which must be taken into account during the preoperative preparation of the patient and during the operation. It is recommended to stop taking tamsulosin 1–2 weeks before surgery for cataracts or glaucoma, but the benefit of stopping tamsulosin therapy has not yet been proven. Small pupil syndrome may also develop in patients who took tamsulosin for a longer period of time before surgery.
The use of tamsulosin in patients undergoing surgery for cataracts or glaucoma is not recommended.
During preoperative preparation, the ophthalmic surgeon should clarify whether the patient is currently or previously using tamsulosin in order to take appropriate measures, if necessary, to prevent small pupil syndrome.
In short-term and long-term clinical studies, cases of ejaculation disorders were observed in patients taking tamsulosin. In the post-registration period, cases of ejaculation disorders, retrograde ejaculation, and anejaculation were noted.
There have been cases of the development of prolonged erection and priapism during the use of α1-blockers. If an erection persists for more than 4 hours, you should immediately seek medical help. Treatment of priapism should be carried out immediately to avoid damage to penile tissue and irreversible loss of potency.
Impact on the ability to drive vehicles and other mechanisms
No studies have been conducted on the effect of tamsulosin on the ability to drive vehicles and operate machinery. But, given the possibility of dizziness, caution must be exercised when driving vehicles and other machinery, as well as when engaging in other potentially hazardous activities.
Proflosin®
Manufacturer: BERLIN-PHARMA CJSC (Russia)
caps. enteric-soluble long-acting valid 400 mcg: 10, 30 or 100 pcs. Reg. No.: LP-000832
Clinical and pharmacological group:
A drug used for urinary disorders associated with benign prostatic hyperplasia. Alpha1-blocker
Release form, composition and packaging
Long-acting enteric capsules
gelatin; size No. 2; opaque, with a light orange body and a gray-green cap; one black line is marked on the body and cap, “TSLO.4” is printed on the cap; The contents of the capsules are pellets from white to almost white.
| 1 caps. | |
| tamsulosin hydrochloride | 400 mcg |
Excipients:
microcrystalline cellulose - 276.9 mg, copolymer of methacrylic acid and ethyl acrylate (1:1) - 16.5 mg, triethyl citrate - 1.65 mg, talc - 16.5 mg.
Pellet shell composition:
copolymer of methacrylic acid and ethyl acrylate (1:1) - 21.63 mg, talc - 8.65 mg, triethyl citrate - 2.16 mg.
Composition of the capsule body:
red iron oxide dye - 0.0239 mg, titanium dioxide - 0.53 mg, yellow iron oxide dye - 0.258 mg, gelatin - 38.938 mg.
Composition of the capsule cap:
indigo carmine - 0.00152 mg, black iron oxide dye - 0.0107 mg, titanium dioxide - 0.356 mg, yellow iron oxide dye - 0.114 mg, gelatin - 23.889 mg.
10 pieces. - blisters (1) - cardboard packs. 10 pieces. - blisters (3) - cardboard packs. 10 pieces. - blisters (10) - cardboard packs.
Description of the active components of the drug "Proflosin®"
pharmachologic effect
Tamsulosin selectively and competitively blocks postsynaptic α1A-adrenergic receptors located in the smooth muscles of the prostate gland, bladder neck and prostatic urethra. This leads to a decrease in the tone of the smooth muscles of the prostate gland, bladder neck, prostatic urethra and improved urine outflow.
α-adrenergic blockers may reduce blood pressure (BP) by reducing peripheral vascular resistance. However, during clinical trials of tamsulosin, in patients with normal blood pressure levels, no clinically significant decrease in blood pressure was observed.
Indications
- benign prostatic hyperplasia (treatment of dysuric disorders).
Dosage regimen
Orally, 1 capsule 1 time per day after breakfast or the first meal. The capsule should be swallowed whole, without chewing, with a sufficient amount of water. The capsule should not be divided into parts or broken, as this may affect the rate of release of the active substance. The duration of use is not limited.
Side effect
Possible side effects when using the drug are listed below in descending frequency of occurrence: often (< 1/10, > 1/100), infrequently (< 1/100, > 1/1000), rarely (< 1/1000, > 1/10000 ), very rare (< 1/10000), including isolated reports.
Nervous system disorders:
often - dizziness; infrequently - headache; rarely - fainting.
Violations by the SSS:
infrequently - tachycardia, orthostatic hypotension.
Gastrointestinal disorders:
uncommon - constipation, diarrhea, nausea, vomiting.
Reproductive system disorders:
infrequently - ejaculation disorders; very rarely - priapism.
Disorders of the skin and subcutaneous tissues:
uncommon - rash, itchy skin, urticaria; rarely - angioedema.
Other:
in some cases - the development of atonic iris syndrome (narrow pupil syndrome) during cataract surgery, asthenia, rhinitis.
Contraindications
- hypersensitivity to tamsulosin or other components of the drug;
- orthostatic hypotension (including history);
- severe liver failure.
Carefully
— chronic renal failure (creatinine clearance less than 10 ml/min);
- arterial hypotension.
Pregnancy and lactation
The drug is prescribed only to men.
Use for liver dysfunction
Contraindicated in severe liver failure.
Use for renal impairment
Use the drug with caution in chronic liver diseases (creatinine clearance less than 10 ml/min)
special instructions
At the first signs of orthostatic hypotension (dizziness, weakness), the patient should be seated or laid down.
Before starting therapy with Proflosin®, the patient should exclude the presence of diseases and conditions that could cause symptoms similar to those of benign prostatic hyperplasia.
Before starting treatment and regularly during therapy, a digital rectal examination and, if necessary, determination of the concentration of prostate specific antigen (PSA) should be performed.
If angioedema develops, therapy with Proflosin should be stopped immediately. Repeated administration of the drug is contraindicated. During surgery for cataracts while taking the drug, the development of atonic iris syndrome is possible, which must be taken into account by the surgeon for the preoperative preparation of the patient and during the operation.
Impact on the ability to drive a vehicle and other complex mechanisms
Care must be taken when driving vehicles and engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions, due to the fact that dizziness may develop.
Overdose
There have been no cases of overdose while taking the drug to date. However, theoretically, there is a possibility of a sharp decrease in blood pressure and tachycardia, which may require appropriate measures. To restore blood pressure (including orthostatic hypotension) and heart rate to normal values, the patient must be laid down. Hemodialysis is not advisable because tamsulosin has a high affinity for plasma proteins.
To prevent further absorption of tamsulosin, it is advisable to lavage the stomach, take activated charcoal or an osmotic laxative (for example, sodium sulfate).
Drug interactions
Tamsulosin does not interact with atenolol, enalapril, nifedipine and theophylline.
When used simultaneously with cimetidine, a slight increase in the concentration of tamsulosin in the blood plasma was observed; with furosemide - a decrease in concentration, but this does not require adjustment of the dose of the drug Proflosin®, since the concentration of the drug remains within the normal range.
Diclofenac and warfarin may increase the elimination rate of tamsulosin.
The simultaneous administration of tamsulosin with other ai-adrenergic receptor blockers can lead to a decrease in blood pressure.
Conditions for dispensing from pharmacies
On prescription.
Storage conditions and periods
At a temperature not higher than 30°C. Keep out of the reach of children! Shelf life: 3 years.
Drug interactions
Tamsulosin does not interact with atenolol, enalapril, nifedipine and theophylline.
When used simultaneously with cimetidine, a slight increase in the concentration of tamsulosin in the blood plasma was observed; with furosemide - a decrease in concentration, but this does not require adjustment of the dose of the drug Proflosin®, since the concentration of the drug remains within the normal range.
Diclofenac and warfarin may increase the elimination rate of tamsulosin.
The simultaneous administration of tamsulosin with other ai-adrenergic receptor blockers can lead to a decrease in blood pressure.
Alcohol and drugs
Very often, patients taking medications drink alcohol. As a result, many people drink alcohol when there is a drug in their system, or vice versa. Thus, of 869 American patients who regularly took medications, 348 (40.0%) combined their medication with alcohol. In more than 20% of cases these combinations were clinically significant. Another study showed that 60% of elderly patients simultaneously take medications and regularly drink alcohol (1). At the same time, patients are not aware, do not attach importance, do not understand, or forget that alcohol can interact with medications. It is important for the primary care provider to know what medications alcohol does not combine with in order to properly advise and promptly remind about the need to avoid drinking alcohol. We will consider important significant interactions that need to be remembered in the article.
Alcohol has its own toxic effect on the body, and its combination with drugs can lead to a variety of undesirable consequences. Alcohol and medications can mutually influence each other. The consequences of joint use cannot be predicted with certainty, since many variables play a role here: drugs, characteristics of the patient’s biochemistry, quantity, type, strength and regularity of alcohol consumption, concomitant diseases and other factors.
Alcohol can negate or enhance the effect of drugs and vice versa, and medications can enhance the pharmacological effect of alcohol on organs and systems (liver, central nervous system).
Variations in alcohol interactions depending on dose, duration of use and concentration
- Mild alcoholic drinks can enhance the absorption of drugs, which will lead to a sharp increase in concentration and result in manifestations of an overdose. This can happen if a person takes a pill while drinking alcohol.
- Forty percent alcohol or more irritates the stomach and causes hypersecretion of gastric mucus. A layer of mucus protects the stomach from the irritating effects of strong alcohol and at the same time prevents the absorption of drugs.
- Drug metabolism occurs in the liver under the influence of the cytochrome enzyme system. Ethyl alcohol, consumed once in a large dose, inhibits cytochrome P-450 enzymes, while its intake over a long period of time in small and medium doses induces enzymes (1). An illustrative example in this case is warfarin . This drug is prescribed for a long time. If a person taking warfarin drinks a large dose of alcohol at once, they will have an increased risk of bleeding. And in a patient who regularly drinks a little, on the contrary, the effectiveness of warfarin will decrease and the risk of thrombosis will increase (2).
The doses of alcohol required to suppress or activate liver function are individual and vary over a wide range.
There are few scientific works devoted to the interaction of drugs and alcohol. However, there are known combinations of drugs with ethanol, obtained empirically and their negative consequences. Here are the known dangerous and undesirable interactions between ethyl alcohol and drugs.
Antihypertensive, vasodilator drugs and alcohol
- The classic combination of clonidine (Clonidine) and alcohol has long gone down in history. Concomitant use causes a sharp drop in blood pressure, collapse, amnesia and can be fatal (3).
- Ethanol dilates blood vessels, so combination with Nitroglycerin or another vasodilator can lead to orthostatic hypotension and acute vascular insufficiency (1.4).
- Taking ethanol during anaprilin therapy can sharply reduce blood pressure (5). With chronic alcohol consumption, anaprilin loses its effectiveness, and the depression of the central nervous system by ethanol increases (2.5).
- After vasodilation when drinking alcohol, there is a constriction phase, which is important for hypertensive patients taking antihypertensive drugs. Drinking alcohol can neutralize the effect of drugs and cause a rise in blood pressure.
Alcohol and drugs acting on the central nervous system
- Taking alcohol together with antipsychotics ( Aminazin , etc.), tranquilizers (especially benzodiazepines ), hypnotics ( barbiturates , etc.), narcotic analgesics ( Tramadol, Fentanyl, codeine-containing drugs ) potentiates the inhibitory effect on the central nervous system. This is expressed in memory impairment, coordination, drowsiness, loss of consciousness, even stopping breathing (4.6).
- Combinations of alcohol with first-generation antihistamines Suprastin, Diphenhydramine, Tavegil, Diazolin, Ketotifen ) lead to increased sedation, headache, lethargy, and loss of consciousness (3).
- Drinking alcohol during therapy with antidepressants-MAO inhibitors ( Nialamide, Iproniazid ) can cause increased heart rate, vasospasm, increased blood pressure, the risk of hypertensive crisis, “tyramine syndrome” (7). Alcohol stimulates the release of adrenaline, which should normally be inactivated by monoamine oxidase. And alcoholic drinks such as red wine and unrefined beer contain tyramine, which has a structure and effect similar to adrenaline.
- Ethanol may slow down the liver metabolism of tricyclic antidepressants ( Amitriptyline, Maprotiline, Clomipramine, Imipramine ). As a result, you can get hypersedation, cardiac arrhythmia, convulsions, hallucinations and other severe consequences, including coma (8). Alcohol is a depressant and is therefore pharmacologically incompatible with all antidepressants.
- Ethyl alcohol also affects other drugs with a central mechanism of action. Alcohol enhances the sedative effect of the antiemetic drug Metoclopramide and reduces the tolerance of Bromocriptine , used to suppress lactation, which is manifested by drowsiness, decreased blood pressure, lethargy, tachycardia and other adverse reactions (9,10). The muscle relaxant Baclofen enhances the inhibitory effect of ethanol. Joint use provokes general weakness, drowsiness, dizziness, and decreased blood pressure (11).
Combined effects of ethanol and drugs on the liver
Concomitant use with alcohol of drugs that adversely affect the liver, such as, for example, Metronidazole , increases the risk of hepatotoxicity. The combination of alcohol and paracetamol is especially dangerous . It is often taken as an antipyretic and analgesic, and is included in almost all cold powders and in many painkillers. People who drink regularly increase the activity of the CYP2E enzyme, which metabolizes paracetamol to N-acetyl-p-benzoquinone imine, which is toxic to the liver. At the same time, the amount of glutathione, which neutralizes it, decreases with constant alcohol consumption. The dangerous metabolite destroys hepatocytes and acute liver failure may occur (2).
Combinations of alcohol with Furazolidone , Cephalosporins ( Cefamandol, Cefoperazone ), hypoglycemic sulfonylurea derivatives ( Tolbutamide, Chlorpropamide, Glibenclamide, Glipizide, Gliclazide, Glimepiride ), Isoniazid , oral contraceptives , Doxycycline (4) will be difficult for the liver.
Statins are a group of drugs that are dangerous in terms of hepatotoxicity and the development of cirrhosis and liver failure when combined with alcohol.
With chronic alcoholism, liver damage occurs up to cirrhosis, detoxification function deteriorates and the liver can no longer cope with the neutralization of drugs (12). In this case, it is necessary for the doctor to adjust the dosage of drugs towards a reduction.
Alcohol combined with insulin and hypoglycemic agents
Ethanol suppresses gluconeogenesis, which increases the risk of hypoglycemia, and when combined with alcohol, this can lead to hypoglycemic coma. Moreover, at first, when drinking alcohol, the glucose level increases. Such glucose surges do not have the best effect on well-being and distort the picture when monitoring blood glucose levels (2.7).
Ethanol can either increase or decrease the hypoglycemic effect of insulin , also causing changes in blood glucose concentrations (8). Chronic consumption of alcoholic beverages during treatment with Metformin can lead to lactic acidosis (2).
Hypoglycemic sulfonylureas slow down the biotransformation of alcohol (7).
Some other combinations
- Alcohol and NSAIDs: Aspirin, Diclofenac, Ibuprofen, Indomethacin, Ketorolac and others increase the irritant effect on the gastrointestinal mucosa, creating a risk of erosion and gastrointestinal bleeding (2).
- Combinations with anticoagulants such as the aforementioned Warfarin, as well as Sinkumar and Phenilin, are dangerous. In combination, they can lead to an increased risk of poorly controlled bleeding, especially internal bleeding. Brain hemorrhage or stroke can be fatal (7).
- Alcohol reduces the effectiveness of female sex hormones , and they in turn slow down the metabolism of ethanol (4).
- Caffeine, taken as a psychostimulant during intoxication or as part of painkillers for headaches, subsequently increases intoxication even further by facilitating the penetration of ethanol through the blood-brain barrier. It can provoke a hypertensive crisis, and if used frequently with alcohol, it can cause wear and tear of the heart muscle (7).
- Alcohol consumption leads to potassium deficiency, for this reason arrhythmias may occur with cardiac glycosides and diuretics (7).
Medicines that affect the biotransformation of alcohol.
Ethanol is neutralized by the liver in 2 stages. First, alcohol dehydrogenase to toxic acetaldehyde, and then aldehyde dehydrogenase to acetic acid. A number of drugs inhibit the work of aldehyde dehydrogenase, and “acetaldehyde syndrome” appears in the body. A person experiences fever, shortness of breath, palpitations, nausea, vomiting, general malaise, increased sweating, chills, heart pain, heaviness in the head, a feeling of fear for life, and blood pressure may drop. It is this property that forms the basis for the treatment of alcohol dependence with disulfiram, which suppresses the production of acetaldehydrogenase in the liver (7). The reaction caused by taking disulfiram is called disulfiram-ethanol reaction. Metronidazole, ornidazole, chloramphenicol, furazolidone, some cephalosporins, ketoconazole, clotrimazole, griseofulvin, isoniazid, sulfamethoxazole/trimethoprim have an antabuse-like effect. Drinking alcohol in any form during treatment with these drugs and for at least three days after completion is contraindicated.
Slows down the conversion of alcohol into acetaldehyde and analgin : simultaneous use increases intoxication (7, 13). The drug Verapamil slows down the elimination of alcohol, increasing its toxicity (14).
Alcohol and antibiotics
A number of antibiotics, antimicrobial and antifungal agents, which we mentioned above, cause unwanted disulfiram-like reactions when taken together with alcohol. There is evidence that ethanol reduces the effectiveness of antibiotics. In particular, ethanol reduces the plasma concentration of doxycycline, which means it does not have the required effect (15).
There are no strict restrictions on taking alcohol with other antibiotics. A good reason not to drink while on antibiotic therapy is that alcohol definitely does not help mobilize the body’s defenses in the fight against infection, but creates additional stress on the liver, which is busy removing drugs and microbial toxins. Therefore, when treating with antibiotics, it is better to avoid alcohol.
The result of drinking alcohol in combination with medications can be unpredictable, and as experience shows, in most cases it is negative for the body. Therefore, to the buyer’s question: “Can I drink during treatment?” — it is important to remember about dangerous combinations, and it is better to recommend refraining from taking alcohol with any medications.
- Tarlovskaya, E. I., Koziolova, N. A., & Chesnikova, A. I. (2016). The influence of lifestyle on the effectiveness and safety of drugs in cardiology practice: what should a doctor take into account? Russian Journal of Cardiology, (1 (129)).
- Drug-Alcohol Interactions: A Review of Three Therapeutic Classes. – [Electronic resource] –URL: https://www.uspharmacist.com/article/drug-alcohol-interactions-a-review-of-three-therapeutic-classes
- Interaction of drugs with ethyl alcohol and drinks containing alcohol. – [Electronic resource] –URL: https://www.sechenov.ru/pressroom/publications/vzaimodeystvie-ls-s-etilovym-spirtom-i-napitkami-soderzhashchimi-alkogol1/
- 5 arguments why you should not combine medications with alcohol. – [Electronic resource] – URL: https://e.novapteca.ru/515015
- According to GRLS: Instructions for the drug Anaprilin.URL: https://grls.rosminzdrav.ru/Grls_View_v2.aspx?routingGuid=9a012de3-42a9-4c94-8acf-577d914bd055&t
- Mosolov, S. N., Malin, D. I., Ryvkin, P. V., & Sychev, D. A. (2019). Drug interactions of drugs used in psychiatric practice. Modern therapy of mental disorders, 1, 1-35.
- Register of Medicines of Russia RLS Patient 2003. - Moscow, Register of Medicines of Russia, 2002. > Part 2. Medicine and people > Chapter 2.10. Medicines and alcohol Classes. – [Electronic resource] – URL: https://www.rlsnet.ru/library/books/rls-pacient-2003/chast-2.-lekarstvo-i-chelovek/glava-2.10.-lekarstva-i-alkogol
- Interaction of drugs with alcohol: myths and facts. – [Electronic resource] –URL: https://www.katrenstyle.ru/goods_sales/vzaimodeystvie_ls_s_alkogolem_mify_i_fakty
- According to GRLS: Instructions for the drug Metoclopramide. URL: https://grls.rosminzdrav.ru/Grls_View_v2.aspx?routingGuid=318293c0-1254-4297-8bbe-9397c1324155&t
- According to GRLS: Instructions for the drug Bromocriptine-Richter. URL: https://grls.rosminzdrav.ru/Grls_View_v2.aspx?routingGuid=ad112abc-121b-4205-b67e-c3a09449d6b0&t
- According to GRLS: Instructions for the drug Baclofen. URL: https://grls.rosminzdrav.ru/Grls_View_v2.aspx?routingGuid=cb8768ea-cd94-4ed5-a25f-2ed7241ef4f8&t
- Bochanova, E. What drugs should not be mixed with and why. Memo to the first capital / E. Bochanova // New pharmacy. – 2022. – No. 8. – P. 106-111.
- According to GRLS: Instructions for the drug Analgin. URL: https://grls.rosminzdrav.ru/Grls_View_v2.aspx?routingGuid=52ecec84-94fc-45bf-84cc-c4eb9acbb6b6&t
- According to GRLS: Instructions for the drug Verapamil. URL: https://grls.rosminzdrav.ru/Grls_View_v2.aspx?routingGuid=880c1df5-64ee-407d-ab42-1e6a828de133&t
- According to GRLS: Instructions for the drug Doxycycline. URL: https://grls.rosminzdrav.ru/Grls_View_v2.aspx?routingGuid=fc67c3ef-4b1b-4e64-bc93-1721897fe259&t
We answer questions live on VKontakte: https://vk.com/pharmznanie
You can discuss the latest news with all your Russian colleagues in chats: Telegram: https://tglink.ru/pharmordenVKontakte: https://vk.me/join/AJQ1d_D2XxaDy9IdzL0e6EqH To leave a comment on the article, you need to register or log in.
Interested in the article? You can find out even more in the section Working in a pharmacy