This article uses excerpts from the chapter of the same name in the Face Anatomy atlas. It is of particular importance for specialists involved in the correction of age-related changes and contouring using fillers. The title “Dangerous triangle of the face” was not chosen by chance; it is in this zone that there are prerequisites of an anatomical and functional nature that can interfere with medical manipulation and cause side effects, including severe ones. Let's look at the topography of this triangle and the reasons for its danger.
Introduction
So, a dangerous triangle of the face. We can describe this zone in this way: the apex of the triangle is located in the glabella area, its legs enclose the nasolabial folds and reach the base, which is located under the lower lip [Fig. 1].
Rice. 1. Dangerous triangle of the face.
The area within this zone is often corrected with filler: just think about glabellar lines, nasal hump correction, nasolabial folds and lip remodeling. The anatomical feature, or originality of this zone, which makes it so “insidious”, lies in its blood supply and especially in the topography of the arteries.
Preparing for a non-surgical procedure
Before elective stenting, your endovascular surgeon will review your medical history and perform a physical examination. Can be assigned:
- Ultrasound . To obtain images using sound waves of the narrowed artery and the speed of blood flow to the brain.
- Contrast-enhanced computed tomography (MSCT) or Magnetic resonance angiography (MRA) . This diagnostic produces highly detailed images of blood vessels using radiofrequency waves in a magnetic field or X-rays injected with a radiopaque contrast agent.
Food and medicine
You will receive instructions about what you can eat or drink before your angioplasty and ICA stenting. Preparation may be different if you are already in the hospital before the intervention.
The night before your endovascular surgery:
- Follow your doctor's instructions about adjustments to your current medications. Your doctor may tell you to stop taking certain medications before having angioplasty, especially if you take certain diabetes medications or blood thinners.
- Arrange transportation home in advance. Angioplasty usually requires a hospital stay, and you may not be able to go home the next day due to the lingering effects of the sedation.
Triangle and arteries
One of the main arteries in this area is the facial artery, a branch of the external carotid artery. The facial artery, immediately after its origin, goes upward and passes to the face in front of the masticatory muscle, where its pulsation can be determined by palpation. Next, it is directed medially and towards the lips, giving off branches - the superior and inferior labial arteries, then passes under the muscle that lifts the upper lip, and reaches the wing of the nose, where its course becomes superficial and ends with two terminal branches - the arteries of the wing of the nose and the angular . Up to this point, everything is clear and clear, but in reality this is not always the case [Fig. 2].
Rice. 2. Facial artery - angular artery.
I will explain more clearly: there are many works with cadavers that emphasize the fact of the existence of frequently encountered anatomical variations and the place of origin of the facial artery, the course of this vessel and its branches. Often such variations are more the norm than the exception. Therefore, it can be argued that even with in-depth knowledge of anatomy, there is a possibility of complications due to the abnormal arrangement of blood vessels. Therefore, it is necessary to use techniques that help to avoid possible side effects as much as possible.
Classification of diseases
The main classification of diseases of the vascular bed of the brain depends on the cause of the development of the pathology. This is important for choosing treatment tactics that should affect the etiology. The following are the main groups of diseases of the brachiocephalic vessels:
- congenital pathology - arteries develop with anatomical anomalies, pathological tortuosity, impaired development of connective tissue areas or the muscular layer of arteries may be observed;
- atherosclerotic changes - this type of disease is the most common;
- narrowing of the lumen of the artery due to external pathology - a volumetric process or pathology of the spinal column at the site of the artery;
- inflammation of the vascular wall - vasculitis;
- alternate decreases and increases in blood pressure;
- compression of blood vessels due to pathology of the spinal column;
- aneurysm - expansion of the vessel and protrusion of its wall in the form of a “pocket”;
- changes in blood vessels due to the underlying disease (diabetes, endocrine pathology);
- consequences of injuries and surgical interventions.
If we talk about the frequency of occurrence, atherosclerosis accounts for about 90% of all cases of pathology of the brachiocephalic arteries. Atherosclerosis develops as a result of exposure to risk factors - hereditary predisposition, smoking, age-related changes, disorders of fat metabolism (chronic pathologies).
Chronic cerebrovascular diseases can be compared to a time-delayed explosive device - you never know when the mechanism will go off. However, there is always a risk to health and even life. Timely consultation with a doctor and initiation of treatment minimizes the risk of disability and death.
Possible side effects
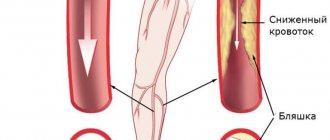
Basically, complications arise not so much due to rupture of a venous vessel, but due to interruption of arterial blood flow due to compression or when the drug is administered into the lumen of the vessel with subsequent embolization of the terminal branches with small fragments [Fig. 3].
Rice. 3. Reasons for the development of skin necrosis. Intravasal injection (top), vessel compression (bottom).
What could happen next? Stopping arterial flow leads to necrosis and tissue death in the blood supply zone of a given vessel. Cases of necrosis of the skin of the wing and tip of the nose, lip tissue and glabella area have been described [Fig. 4–5].
Rice. 4. Necrosis of the tip or wing of the nose.
Rice. 5. Zones of necrosis.
An even more serious risk factor is associated with the fact that the facial artery represents the communication between the external and internal carotid arteries. Its terminal branch, the angular artery, anastomoses with the ophthalmic artery, a branch of the internal carotid artery. It is this connection between the vessels that can lead to embolization of the ophthalmic artery with small fragments of filler and further penetration into the central retinal artery with a possible decrease in vision up to blindness [Fig. 6–7].
Rice. 6. Iatrogenic retinal artery occlusion caused by the injection of fillers.
Rice. 7. Microembolism of the ophthalmic artery: etiopathogenesis.
Treatment methods at the Innovative Vascular Center
The vascular surgeons of our clinic have significant experience in unique operations on the carotid arteries with pathological tortuosity. The main problem for surgical treatment is determining clear indications for surgical treatment. Our clinic has developed a clear diagnostic protocol that allows us to determine the clinical significance of a particular tortuosity and the degree of its effect on cerebral blood flow. The experience of successful operations in our clinic for pathological tortuosity exceeds 200 cases.
Therapeutic strategies to prevent and manage complications
It is obvious that it is necessary to use techniques that minimize the risk of developing these dangerous complications. The text of the atlas describes, area by area, all the precautions and manipulations that must be taken to reduce this risk: the use of a cannula, the depth of injection, the quantity and quality of filler injected, and so on. Pallor of the skin and patient complaints of sudden pain in the injection area are signs that blood flow has stopped in this area. We must be able to control this situation.
All measures are aimed at restoring blood flow: urgent dissolution of the filler (if hyaluronic acid was used), warm compresses, massage, etc. Then there are prescriptions that need to be followed at home: antibiotic therapy to prevent bacterial superinfection, antiplatelet agents, topical medications.
In the introduction to the atlas I placed the inscription
“Only non-practitioners do not make mistakes; only through practice does it become possible to reduce the risk of error.”
If all measures are carried out on time and correctly, the spread of the necrosis zone will be minimal, a large area of skin will be preserved and, therefore, the chance of restitutio ad integrum will be higher.
Stenosis of the internal carotid artery, vertebral artery
January 6, 2016
In the body, arteries carry oxygen-rich blood from the heart throughout the body. The carotid arteries (one on each side of the neck) deliver blood to the brain. The vertebral arteries, which pass through the spine, supply blood to the back of the brain (brain stem and cerebellum). Carotid artery stenosis is a narrowing of the carotid artery, which usually develops as a result of atherosclerosis. Atherosclerosis is an extremely complex degenerative disease. Today, scientists do not know the main cause of atherosclerosis, however, many components are known that contribute to the development of atherosclerotic lesions. One of the most popular theories states that atherosclerosis occurs as a response to injury to the arterial wall. Factors known to contribute to arterial wall injury include mechanical factors such as hypertension and low wall elasticity, as well as chemical factors such as nicotine, hyperlipidemia, hyperglycemia, and homocysteine. Lipid accumulation begins in vascular smooth muscle cells and macrophages as a result of the inflammatory response to injury. These lipid deposits can narrow or block the carotid artery, thereby increasing the risk of stroke. Factors that increase the risk of developing stenosis include: - Family history of atherosclerosis (any location); - Age. The risk of developing atherosclerosis increases with age, in particular, men under the age of 75 years have a greater risk of developing carotid atherosclerosis than women, but after 75 years of age, women have a higher risk than men; - High levels of low-density lipoprotein (LDL, “bad cholesterol”) and triglycerides in the blood. However, this factor is less pronounced than for coronary heart disease; — Smoking; — High blood pressure (hypertension); — Diabetes; — Obesity; - Sedentary lifestyle
As a rule, carotid artery stenosis develops several years later than the coronary arteries are affected. People with coronary artery disease or other atherosclerosis (eg, peripheral artery disease) are at higher risk of developing carotid artery stenosis. There are no symptoms of carotid artery stenosis, but there are warning signs of a stroke. Transient ischemic attacks (called "mini-stroke") are one of the most important warning signs of stroke. Transient ischemic attacks occur when a “blood clot” briefly blocks an artery supplying blood to the brain. The following symptoms of transient attacks, which are temporary in nature, can last from a few minutes to several hours: - Sudden loss of vision or blurred vision in one or both eyes; - Weakness and/or numbness on one side of the face, or in one arm or leg, or on one side of the body; - Slurred speech, or difficulty understanding what others say; - Loss of coordination; - Dizziness or confusion; - Difficulty swallowing. Transient attacks are a medical emergency because it is impossible to predict whether the condition will progress to an ischemic stroke. If you or someone you know experiences these symptoms, call an ambulance immediately. Immediate treatment may save your life or increase your chances of a full recovery. Transient attacks, to some extent, are harbingers of a future stroke; a major stroke is 10 times more likely to develop in people who have survived transient attacks. An ischemic stroke occurs when a blood vessel in the brain becomes blocked for one reason or another. The brain is unable to accumulate and store oxygen, and functions as long as the network of blood vessels provides it with arterial, oxygen-rich blood. A stroke causes a lack of blood supply, causing the surrounding nerve cells to be deprived of nutrients and oxygen. If brain tissue is not supplied with oxygen for more than 3 to 4 minutes, the brain begins to die. A stroke can occur if: - the artery becomes significantly narrowed as a result of a blood clot; - part of the blood clot breaks off and moves to a smaller-caliber cerebral artery; - A blood clot blocks a narrowed artery.
Stroke can also occur as a result of other diseases, such as bleeding in the brain (intracerebral hemorrhage), subarachnoid hemorrhage, atrial fibrillation, and cardiomyopathy. Diagnostic tests include:
— Doppler ultrasound of neck vessels. This is a vascular test that uses ultrasound waves to study the presence of narrowing of the carotid arteries. This is the most common test used to evaluate the condition of the carotid arteries;
— Angiography of the carotid arteries. During this invasive procedure, a catheter is inserted into a blood vessel in the arm or leg and connected to the carotid artery. At the next stage, a contrast agent is injected into the catheter and an X-ray of the carotid artery being studied is taken. This test can determine the extent of narrowing or blockage of the carotid artery, determine the risk of stroke, and assess the need for further treatment, such as carotid stenting or surgery;
— Magnetic resonance angiography (MRA) is a scan using a contrast agent that uses a magnetic field and radio waves. MRA provides images of the carotid arteries. In many cases, MRA can provide information that cannot be obtained during X-ray and ultrasound examinations. This test can provide important information about the carotid and vertebral arteries and the degree of their stenosis.
- Computed tomography (CT) of the brain may be performed if a stroke or transient attack is suspected. This test can identify areas of damage in the brain.
— Computed tomography with angiography is a study that uses advanced CT technology to obtain high-resolution 3D images of the carotid arteries. CT angiography allows doctors to determine the degree of stenosis in the carotid and vertebral arteries, as well as evaluate the blood vessels leading to these arteries.
Lifestyle changes.
To prevent the progression of carotid artery stenosis, the National Stroke Association (USA) makes the following recommendations: - Stop smoking; — Control of high blood pressure, cholesterol, diabetes and coronary artery disease; - Eating foods low in saturated fat, cholesterol and sodium; — Achieving and maintaining the desired weight; - Regular exercise - at least 30 minutes of exercise most days a week. — Limiting alcohol consumption; — Find out if you have heart rhythm problems such as atrial fibrillation, which increases your risk of blood clots, which can lead to stroke. If you have atrial fibrillation, you must take anticoagulant medications.
Medications.
Antiplatelet drugs. All patients with carotid artery stenosis should take antiplatelet medications to reduce the risk of stroke and other cardiovascular complications. In some cases, anticoagulants may be prescribed to reduce the risk of blood clots. Tissue plasminogen activators can be used to treat ischemic stroke to dissolve blood clots. Tissue plasminogen activator is effective if given within three hours of the onset of stroke symptoms.
Therapeutic manipulations
Therapeutic procedures such as carotid endarterectomy or carotid artery stenting are used if there is severe carotid artery stenosis and are aimed at preventing a possible stroke.
The vascular surgeon at our clinic, based on the studies mentioned above, will give you recommendations on which treatment method is best in your situation. Carotid endarterectomy is the traditional surgical treatment for carotid artery stenosis. Carotid endarterectomy has been shown to be recommended for symptomatic patients with stenosis of 50 percent or more, as well as for asymptomatic patients with stenosis of 60 percent or more. Carotid endarterectomy can be performed under general anesthesia or local anesthesia with intravenous sedation. During the operation, the surgeon makes an incision in the neck in the projection of the blocked carotid artery. After removing the blood clot or atherosclerotic plaque, the surgeon sutures the vessel and then sutures the skin. Blood flow to the brain is restored through the normal pathway. Carotid angioplasty and stenting are recommended as treatment for some patients (eg, those at high risk for surgery) with carotid artery stenosis. Carotid angioplasty and stenting are performed without general anesthesia, but using sedation. During the manipulation, a balloon catheter is inserted into a blood vessel and, under the control of an angiograph (a special X-ray machine), is directed to the site of blockage or narrowing of the carotid artery. Once in place, the balloon is inflated within a few seconds to open or widen the artery. During stenting, instead of a balloon, a stent (a small mesh tube) corresponding to the size of the artery is placed in the narrowed area. The stent remains in place permanently and, by supporting the walls of the arteries, the lumen of the vessel remains open. Studies have shown that carotid artery stenting, when used with an embolic protection device, is safe and effective. Both carotid endarterectomy and carotid angioplasty and stenting usually do not require a long hospital stay. Patients often return to normal activities within one to two weeks.