September 22, 2020
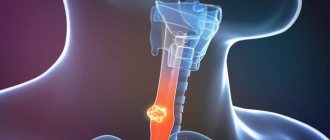
Gastritis is an inflammation of the gastric mucosa, leading to disruption of its secretory function
Gastritis is an inflammation of the gastric mucosa, leading to disruption of its secretory function. During the inflammatory process, food entering the stomach is poorly digested, which leads to impaired absorption of nutrients.
Chronic gastritis affects about 60-85% of the world's population, including young people aged 18 to 35 years. Due to the modern rhythm of life, gastritis has begun to occur more often in children aged 5 to 13 years. Among all diseases of the gastrointestinal tract, gastritis is the most common; a common “marker” of gastritis is the appearance of pain in the stomach. American scientists Marshall and Warren received the Nobel Prize for their discovery of the infectious mechanism of gastritis, caused by the microorganism Helicobacter pylori. This microorganism has been identified in the mucous membranes of many patients suffering from chronic gastritis.
Causes of gastritis
As previously mentioned, the main trigger of the disease is infection with the bacterium Helicobacter Pylori. Excessive proliferation of this bacterium in the stomach leads to irritation of the intestinal mucosa and provokes gastric ulcers. Helicobacter is also considered a serious factor in the development of stomach and small intestine cancer. Scientists are inclined to contact and household transmission of infection from the patient and the carrier. Abuse of drugs that can irritate the walls of the stomach, which include anti-inflammatory drugs and drugs containing acids, also provokes the development of gastritis.
Strong alcoholic drinks, carbonated drinks, and drinks containing acid cause irritation and chemical burns to the walls of the stomach. Smoking, in turn, stimulates excessive secretion of gastric juice, so at the treatment stage the patient is advised to give up the bad habit. If we talk about dietary habits, a diet containing insufficient fiber prevents the gastrointestinal tract from working properly. A diet rich in processed foods and low in fresh foods leads to increased secretion of gastric juices, which irritate the stomach walls.
Excessive alcohol consumption can irritate the stomach lining, making it more vulnerable to infection. Gastritis may be associated with other diseases, including HIV/AIDS, Crohn's disease, and parasitic infections. Nervous factors and various types of stress are of great importance in the development of chronic gastritis. Chronic gastritis also often develops against the background of other diseases of the gastrointestinal tract (chronic enterocolitis, helminthic infestations, diseases of the liver, biliary tract, gall bladder, pancreas). Endocrine diseases and metabolic diseases (thyroid disease, diabetes mellitus, iron deficiency anemia) play an important role in the manifestation of the disease. Genetic factors are also important, that is, the transmission of the disease by inheritance.
Vikair
This medicine for gastritis contains not only bismuth from Helicobacter pylori, but also plant components (buckthorn bark, calamus rhizome extract), as well as magnesium carbonate and sodium bicarbonate. This composition of Vikair makes it both an antispasmodic, an antacid and a drug with an astringent and laxative effect. The medicine has low cost and excellent effectiveness, so it is popular in the treatment of gastritis. But it is worth remembering that Vikair is contraindicated during pregnancy and children.
Vikair
Symptoms
Often gastritis is asymptomatic; symptoms indicating the disease may be aching or sharp burning pain in the pit of the stomach, which appears or intensifies during or after eating, heartburn, nausea, vomiting, flatulence, constant belching and heaviness in the abdomen, unreasonable weight loss , unpleasant taste in the mouth, heaviness, feeling of pressure in the chest.
The manifestation of the disease depends on the type of disease. For example, acute gastritis begins suddenly, often after food poisoning. Pain occurs in different areas of the stomach depending on the location of inflammation, and intensifies when taking foods that irritate the mucous membrane. The main symptoms of the acute phase of the disease: heartburn, vomiting, belching, frequent gas, bloating, headache, rapid heartbeat, dizziness, increased salivation or extreme thirst. Chronic gastritis is sluggish, symptoms in adults may vary, but this pathology is mainly characterized by belching with a characteristic odor, constant heartburn, a feeling of pain and heaviness, loss of appetite, diarrhea or constipation, coating on the tongue, and weight loss.
Depending on the form and type of gastritis, different treatments are prescribed, so it is important to see a doctor immediately.
Treatment of exacerbations of chronic diseases of the digestive system
P. Ya. Grigoriev, Doctor of Medical Sciences, Professor E. P. Yakovenko, Doctor of Medical Sciences, Professor A. P. Yakovenko, Candidate of Medical Sciences N. A. Agafonova, A. S. Pryanishnikov, P. V. Gulyaev, E V. Talanova, S. B. Kalnova
RGMU, Moscow
The creation of a number of highly effective pharmaceuticals has provided a significant increase in the effectiveness of treatment of patients with pathologies of the digestive system. Among these drugs, histamine H2 receptor blockers (ranitidine, famotidine, etc.), proton pump inhibitors (omeprazole, lansoprazole, pantoprazole, rabiprazole), prokinetics (cisapride, domperidone, prukelopride, etc.), multienzyme drugs (Creon, pancitrate, mezim-forte, lycrease, etc.), antiviral (interferons, ribavirin, lamivudine, etc.), as well as antibacterial and antiparasitic agents. With their optimal use, remission of gastroesophageal reflux disease, gastric and duodenal ulcers is quickly and reliably achieved, and the development of complications of peptic ulcers and hemorrhagic gastroduodenitis is prevented. It is often possible to inhibit viral replication, stop the activity and progression of chronic viral hepatitis B and C, and prevent the transformation of chronic hepatitis into cirrhosis and cirrhosis-liver cancer.
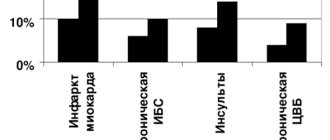
Currently, the role of Helicobacter pylori (Hp) has been proven in the pathogenesis of acute and chronic gastritis, duodenitis, gastric ulcer (GUD), duodenal ulcer (DU), gastric MALT lymphoma and even gastric cancer. The role of HP infection in the pathogenesis of a number of extragastric diseases: coronary heart disease, migraine, liver cirrhosis, etc. is discussed.
The development and introduction into practice of combined anti-Helicobacter drug therapy for peptic ulcer and peptic ulcer radically changed the prognosis of these and some other diseases of the stomach and duodenum.
Seven-day three- or four-component regimens are recognized as the optimal options for eradication therapy for peptic ulcer, peptic ulcer and erosive gastritis (gastroduodenitis) associated with HP. The three-component regimen includes omeprazole 20 mg, or lansoprazole 30 mg, or pantoprazole 40 mg, or pyloride (ranitidine bismuth citrate) 400 mg, taken at 12-hour intervals + clarithromycin 250 mg 2 times a day or amoxicillin 500 mg 4 times a day or 1000 mg 2 times a day, or tetracycline 500 mg 4 times a day or 1000 mg 2 times a day + metronidazole 400 mg 2 times a day or furazolidone 0.2 g 2 times a day. Four-component 7-10-day eradication therapy is used if the previous option was ineffective, and includes omeprazole 20 mg 2 times a day, or lansoprazole 30 mg 2 times a day, or pantoprazole 40 mg 2 times a day + bismuth preparations (Ventrisol or de -nol 120 mg 4 times a day or bismofalk 2 tablets 3 times a day) + tetracycline hydrochloride 500 mg 4 times a day, or amoxicillin 500 mg 4 times a day + metronidazole 250 mg 4 times a day or furazolidone 0.1 g 4 times a day. In this case, all antibacterial drugs must be taken with meals. In a four-component regimen, it is advisable to use the combined drug gastrostat, which contains the same ingredients. Other combinations are not recommended due to their low effectiveness.
After completing 7-10 days of eradication therapy, it is necessary to continue treatment for PU for seven weeks, for DU - five weeks, for erosive gastroduodenitis - three weeks with one of the following antisecretory drugs: ranitidine 300 mg per day, famotidine 40 mg per day, omeprazole 20 mg per day, lansoprazole 30 mg per day, pantoprazole 40 mg per day. Antacids (Maalox, etc.) and cytoprotectors (Venter, etc.) can additionally be used as symptomatic agents.
The above therapy leads to eradication of HP in more than 90% of cases. As a result, active inflammation in the mucous membrane (M) of the stomach and duodenum is stopped, healing of erosions and ulcers is ensured, and the development of exacerbations and complications (bleeding, perforation, stenosis), lymphoma and, possibly, stomach cancer is prevented.
Domestic scientists draw the attention of practitioners to the fact that there is often overdiagnosis of peptic ulcer disease and gastritis (gastroduodenitis), the causes of diseases are not disclosed, and it is not taken into account that the erosive-ulcerative process in the gastroduodenal ulcer is heterogeneous in nature and is not always associated with peptic ulcer. For example, with acute gastritis, erosions, local areas of hemorrhage in the mucus and bleeding may also appear. Histological examination of such patients reveals moderate signs of inflammation in the mucosa. The most common causes of such acute gastritis (gastroduodenitis) are: chemical damage to CO (alcohol, non-steroidal anti-inflammatory drugs, aggressive alkaline liquids), viruses (cytomegalovirus, herpes viruses), bacteria (hemolytic streptococci, etc.), uremia, radiation exposure. Occasionally, some microbes even cause acute phlegmonous gastritis. Scientists were able to establish the causes of stress gastritis, the risk factors for the development of which are: hypoxia, liver and kidney diseases, severe operations, burns, sepsis, and central nervous system injuries. Often, within 24 hours after exposure to stress factors, acute erosions and ulcers occur in the coolant. In this case, approximately 30% of patients experience gastrointestinal bleeding, and in some of them they are massive and life-threatening. In victims with burns, injuries to the upper gastrointestinal tract are often diagnosed, which are called “Curling ulcers”, in which, especially those localized in the duodenum, there is a high risk of not only the development of bleeding, but also perforation. In patients with head trauma and stroke, acute ulcers (Cushing's ulcers) are often found in the gastroduodenal mucus. With these ulcers, especially duodenal localization, there is also a high risk of bleeding and perforation. Therefore, it is extremely important to identify people at high risk of developing stress injuries to the gastrointestinal tract and begin treatment with antisecretory drugs as early as possible to prevent the development of bleeding and perforation.
| Superficial pyloric ulcer |
Domestic scientists have conducted many studies to establish a connection between the use of non-steroidal anti-inflammatory drugs (NSAIDs) and gastrointestinal damage. In patients taking these drugs for rheumatoid arthritis, osteoarthritis and other diseases, ulceration is observed in 15-20% of cases, complications (bleeding and perforation) often occur, especially in people with a history of ulcers. The total risk of gastrointestinal damage in those taking NSAIDs is approximately three times higher than in those not taking these drugs. In older patients (over 65 years of age), this risk increases fivefold. Doctors prescribing these drugs are required to address three objectives: preventing the development of NSAID-induced ulcers (especially in the presence of risk factors), their treatment (often in conditions where continued use of NSAIDs is required), as well as the prevention of damage to the mucosa of the small and large intestine, arising from prolonged use. Despite the fact that a new class of NSAIDs (selective cyclooxygenase-2 inhibitors), which should not have a damaging effect on the gastrointestinal tract, is beginning to be introduced into medical practice, their safety requires clinical confirmation, and these studies have not yet been completed.
The main task of preventing stress gastritis and, to a certain extent, NSAID-associated damage to the gastroduodenal mucus is to increase the pH of the intragastric contents to 4 or higher, since at this pH level the proteolytic enzyme pepsin is inactivated and blood coagulation increases. Today, for this purpose, it is advisable to use histamine H2 receptor blockers (ranitidine, famotidine, etc.) or proton pump inhibitors (omeprazole, lansoprazole, pantoprazole).
Domestic and foreign scientists also paid great attention to the study of various forms of chronic gastritis (CG). Along with CG associated with HP and CG type A, eosinophilic, lymphocytic and granulomatous (Crohn's disease, tuberculosis, histoplasmosis, syphilis, sarcoidosis, etc.) gastritis are distinguished, as well as hypertrophic gastropathy (Menetrier's disease, pseudolymphoma of the stomach, Zollinger syndrome - Ellison), congestive gastropathy with portal hypertension (not true gastritis), alkaline (bile) reflux gastritis. In some forms of hCG, hypo- and achlorhydria and vitamin B12 deficiency develop. According to domestic scientists, the clinical significance of hCG is that it can be considered an early precancerous disease, the development of which occurs from atrophy of the mucous membrane to intestinal metaplasia and further to gastric cancer. The diagnosis of CG should always be based only on the results of a qualified histological examination of targeted biopsies of the coolant, as indicated in the above-mentioned state standards.
One of the most common acid-related diseases is gastroesophageal reflux disease (GERD), for the treatment of which recommendations have been developed and the responsibilities of the patient and the doctor have been defined.
The patient is recommended to: sleep on a bed with the head end elevated by at least 15 cm; reduce body weight if you have morbid obesity; do not lie down after eating for 1.5 hours; do not eat before bed, limit fat intake; stop smoking and drinking alcohol; avoid tight clothing, tight belts, and working in an inclined position; if possible, limit the intake of medications that have a negative effect on the motility of the esophagus and the tone of the lower esophageal sphincter (long-acting nitrates, calcium antagonists, theophylline, myogenic antispasmodics, as well as drugs that damage the esophageal mucus (aspirin and other analogues).
Drug treatment is prescribed differentially depending on the severity of clinical, functional and morphological changes in the upper parts of the digestive tract. For gastroesophageal reflux without esophagitis (there are symptoms, but no visible changes in the esophagus), two treatment options are used. In cases where GERD is combined with a slower evacuation from the stomach, decreased tone of the lower esophageal sphincter, hypomotor intestinal dyskinesia, it is advisable to prescribe oral prokinetics - motilium (domperidone) 10 mg or coordinax (cisapride, peristil and other analogues) 5-10 mg 4 times a day in combination with buffered antacids (Maalox or analogues) one dose one hour after meals and one dose immediately before bedtime. After achieving clinical remission, “on-demand therapy” continues, that is, intermittent symptomatic treatment (for heartburn - motilium + antacid or instant Zantac - 150 mg). In the presence of severe insufficiency of the lower esophageal sphincter and/or high level of intragastric acidity, it is advisable to use histamine H2 receptor blockers (ranitidine 150 mg 2 times a day or famotidine 20 mg 2 times a day), and if they are ineffective, proton pump inhibitors (omeprazole 20 mg per day or lansoprazole 30 mg per day) until clinical remission is achieved. Subsequently, “on-demand therapy” is prescribed, which involves taking antisecretory drugs in half the daily dose or antacids when symptoms of GERD appear.
For grade I reflux esophagitis, histamine H2 receptor blockers are used for 6 weeks - ranitidine 150 mg, or famotidine 20 mg 2 times a day with an interval of 12 hours, or proton pump inhibitors - omeprazole 20 mg per day or lansoprazole 30 mg per day day. When remission occurs (on average after 6 weeks), the patient is transferred to “on demand” therapy using antacids, or H2 blockers, or proton pump inhibitors.
For grade II reflux esophagitis, treatment with proton pump inhibitors - omeprazole, or lansoprazole, or pantoprazole in the full daily dose - is carried out for 8 weeks. Less commonly used are H2 blockers - ranitidine 300 mg or famotidine 40 mg 2 times a day until the symptoms of the disease are relieved, followed by a dose reduction to 150 mg and 20 mg 2 times a day, respectively. After 8 weeks, if remission occurs, the course of treatment is stopped and the patient is transferred to on-demand therapy.
For grade III-1V reflux esophagitis, a proton pump inhibitor omeprazole 20 mg or lansoprazole 30 mg is prescribed for 4 weeks, 2 times a day with an interval of 12 hours. Further, when the symptoms of GERD are relieved, omeprazole 20 mg per day or lansoprazole 30 mg per day is continued for up to 8 weeks, followed by transition to continuous maintenance therapy using the above drugs in half the daily dose for a year. If this therapy is insufficiently effective, it is possible to combine antisecretory agents with prokinetic agents such as Motilium or Coordinax in normal daily doses. Additional treatments for refractory forms of GERD include sucralfate (Venter, Sucrat-gel) 1.0 g 4 times a day 30 minutes before meals for one month.
Practitioners often encounter patients with bacterial overgrowth syndrome (SIBO) and changes in the composition of microflora in the intestines, called dysbiosis. Various reasons can lead to the occurrence of this syndrome: diseases of the digestive system, accompanied by secretory-motor disorders, especially in the presence of foci of inflammation; previous acute intestinal infections (bacterial dysentery, yersinia enterocolitis, etc.); long-term use of medications that affect the secretion of digestive glands, epithelial regeneration and motor-evacuation function of the digestive tract; long-term and sometimes irrational use of antibacterial drugs; malnutrition; alcoholism. Clinical manifestations of bacterial overgrowth syndrome in the intestine are associated with hyperexcess production of organic acids and premature deconjugation of bile acids, release of bacterial toxins, destruction of digestive enzymes, and the development of motor disorders.
SIBO is characterized by the presence of abdominal pain or discomfort in the abdomen, abnormal stool (change in shape and loss of passage), bloating and a feeling of fullness in the abdomen, weight loss, weakness, increased fatigue, and irritability. Treatment of SIBO, along with an appropriate diet, includes one or two seven-day courses of antibacterial therapy, the prescription of enzyme preparations, medications that regulate intestinal motor-evacuation function and intraintestinal pH level, eliminating deficiency of vitamins, mineral elements, etc., that is, a combined treatment is carried out. Indications for prescribing antibacterial therapy are: 1) excessive bacterial growth in the small intestine; 2) the presence of inflammatory changes in the intestinal mucosa; 3) identification of opportunistic microflora in intestinal content cultures.
For SIBO in the small intestine, one of the following antibacterial drugs is mainly used: tetracycline hydrochloride 250 mg 4 times a day, ciprofloxacin 250 mg 2 times a day, Biseptol 960 mg 2 times a day, metronidazole 500 mg 2 times a day, furazolidone 100 mg 3-4 times a day, ersefuril 200 mg 4 times a day, intetrix 1 caps. 4 times a day, cephalexin 250 mg 4 times a day. In some cases, you can use enterol 2-4 capsules or packets per day. For SIBO in the colon, preference is given to one of the following drugs: phthalazole or sulgin 1.0 g per day, ersefuril 800 mg per day, Intetrix 4 capsules per day, metronidazole 1.0 g per day, bactisubtil 4-6 capsules per day.
After completing the course of antibacterial therapy, probiotics are prescribed - preparations containing normal strains of intestinal flora and prebiotics - agents that ensure their growth and functional activity. To restore the microflora of the small intestine, probiotics containing aerobic strains are used (bifiform 2-4 capsules per day or lactobacterin 5-10 doses per day), in the colon - probiotics containing anaerobic strains (bifidumbacterin 5-10 doses per day or colibacterin 5-10 doses per day), large and small intestine - combination drugs (bifiform 2-4 capsules per day or bificol 5-10 doses per day). The duration of their use is 2-4 weeks.
Bifiform is a probiotic, one capsule of which contains bifidumbacterin and enterococci in a volume of at least 10 to the seventh power of each type of bacteria. The capsules of the drug are covered with an enteric coating, due to which the bacteria reach the intestines unchanged. The presence of anaerobic flora in the preparation makes it universal for restoring the microbiocenosis of the small and large intestines. In addition, each capsule contains a special nutrient medium necessary for the growth and reproduction of lactic acid bacteria, which allows the microflora contained in the bifiform preparation to survive and be metabolically active.
Our study involved 119 patients, including 68 women and 51 men aged from 21 to 76 years (average age 39.7 years).
To develop effective approaches to prescribing bifiform, we have tested three treatment regimens. The first regimen, in which bifiform was prescribed without previous therapy aimed at intestinal decontamination, was used in 37 patients. The second regimen, which involved taking bifiform after previous intestinal decontamination, was prescribed to 28 patients. The third regimen, in which treatment with bifiform was carried out as monotherapy, was received by 24 patients. Patients in the control group received therapy similar to the second regimen, but they did not receive bifiform or other probiotics.
Bifiform was prescribed 1 capsule twice a day for 15 days. However, if by the seventh day of treatment the severity of clinical manifestations decreased by less than one degree, the dose of the drug was increased to 2 capsules twice a day and therapy continued for another two weeks. To decontaminate the intestines and relieve inflammation in patients with chronic diseases of the digestive system, one to three courses of antimicrobial therapy lasting from five to seven days were carried out with a change of drugs in the next course.
Taking bifiform had a positive effect on the composition of the intestinal microflora. By the end of treatment, 35 (76.1%) patients showed restoration of normal intestinal microflora, and only 11 (23.9%) its composition remained changed. In most patients, the total amount of intestinal flora normalized, an increase in the number of E. coli, bifidobacteria, normalization of the content of enterococci and the disappearance of opportunistic enterobacteria (lactose-negative, hemolyzing strains of intestinal flora, representatives of the genera Klebsiella, Enterobacter, Proteus, Pseudomonas, Citrobacter, etc.) were noted. It should be noted that a significant proportion of patients who still had changes in the composition of the intestinal flora also had clinical symptoms (abdominal pain, flatulence, stool disorders), which confirms their pathogenetic connection.
Bifiform, both in complex treatment and as monotherapy, has shown its effectiveness in relieving the clinical manifestations of dyspepsia, normalizing digestive processes and restoring the normal composition of the intestinal flora in a wide range of diseases of the digestive system. A dose of bifiform 1-2 capsules twice a day for two weeks is quite effective in the management of patients with chronic diseases of the digestive system.
Simultaneously with taking probiotics, a prebiotic is prescribed - hilak-forte, 60 drops 3 times a day for a week, then 30 drops 3 times a day for 1-2 weeks. For persistent constipation, you can additionally use lactulose 15-20 ml once a day until stool normalizes. Approximate treatment regimen for patients with SIBO: 1st week - ersefuril and/or metronidazole + enzyme preparation (mezim-forte, or pancreatin, or festal, or pancitrate, or creon, etc.) + buffer antacid (maalox, or phosphalugel, or alumag, etc.) + adequate regulator of intestinal motor function (no-shpa, or spasmomen, or dittel, or coordinax, etc.); 2-3rd week - hilak + bifiform + enzyme preparation.
The lack of effect from the treatment may be associated with dietary disorders, psychoemotional disorders, alcohol consumption, but more often - incomplete restoration of normal intestinal microflora as a result of inadequate drug therapy.
The success of treatment to a certain extent depends not only on the drug therapy prescribed by the doctor, but also on the patient, who needs to get rid of bad habits, change their lifestyle, take medications punctually, etc. Note to the authors
- the material is submitted in printed form in two copies with the signature of all authors, it is advisable to provide a copy on magnetic media (floppy disk) or sent by e-mail;
- the material is accompanied by a direction from the organization with the signature of the head;
- mandatory information about the author: specialty, academic degree (if any), place of work (institution, department);
- The recommended size of articles is no more than 10 typewritten pages;
- articles are accompanied by an abstract, including the title, authors and main provisions of the article (no more than 10 sentences);
- Illustrative material is desirable: photos, slides, tables, graphs, diagrams, diagrams, etc.;
- the drawing can be submitted in electronic form (.eps or .tif). In this case, the file name must be specified in the material;
- drawings that are attached to the material on a separate sheet must be numbered and provided with information containing the name of the author, the title of the article, as well as the designation of the top and bottom of the drawing;
- Each figure is given a general caption and (if necessary) all digital and letter designations are explained. In the caption to photographs of microslides, it is necessary to indicate the magnification and staining method;
- if the article includes figures from external sources (atlases, magazines, CDs, etc.), then the coordinates of these figures must be accurately indicated;
- If a list of references is attached to the article, then the text must contain digital footnotes.
All materials received by the editors are reviewed by independent reviewers and edited if necessary. The editors are not responsible for the loss of the manuscript.
Submission to the editor of works previously published or submitted for publication in other publications is not permitted.
Do not forget to indicate the exact postal address and telephone number for contact.
Diagnostics.
Diagnosis of chronic gastritis is based on identifying complaints, collecting anamnesis, objective examination and conducting laboratory and instrumental examination methods.
The patient is recommended to undergo a clinical blood test, a biochemical blood test - ALT, AST, total bilirubin, amylase, glucose. The gold standard for diagnosis is an FGDS; to diagnose Helicobacter pylori infection, a urease breath test or a stool test for Hp Ag is used.
Additional methods:
- Ultrasound of the abdominal organs;
- with atrophy of the gastric mucosa - determination in the blood: pepsinogen 1, pensinogen 2, gastrin 17;
- determination of antibodies in the blood to gastric parietal cells and intrinsic Castle factor;
- determination of the level of vitamin B12 in the blood.
Treatment of gastritis
In order to recover from gastritis, it is necessary to follow an individual diet and take a set of medications that will help restore the acid balance of the gastric mucosa.
The treatment regimen depends on the type of gastritis. Treatment is divided into the treatment of gastritis with low acidity using replacement therapy drugs, secretion stimulation drugs, improving microcirculation and symptomatic therapy. Treatment of gastritis with high acidity is carried out using such groups of drugs as secretolytics (proton pump inhibitors, H2-histamine blockers), antacids or alginates, gastroprotectors, which have a protective effect on the mucous membrane of the stomach and duodenum. Also, if the patient is diagnosed with the bacterium Helicobacter pylori, antibiotic therapy is prescribed.
Back to articles
Gastal
"Gastal" are lozenges, so they are always convenient to have on hand and do not need to be washed down with water. It contains magnesium and aluminum, which instantly “quench” heartburn, and the positive effect lasts for about two hours after the tablet is dissolved. "Gastal" not only reduces acidity, but also helps the gastric mucosa to recover. The drug is prescribed in the complex treatment of gastritis and ulcers.
The course of treatment with Gastal is selected by the doctor; you can also use the drug as a one-time “first aid” to relieve the symptoms of heartburn. You can take no more than 8 Gastal tablets per day. It is important that side effects from taking this medication are very rare.
Gastal
TEVA, Ukraine
The combined drug Gastal contains aluminum hydroxide, magnesium carbonate and magnesium oxide.
The combination of active ingredients provides a high antacid (reducing stomach acidity) effect and reducing the possibility of constipation. from 100
1081
- Like
- Write a review
Read also: Top 5 best sorbents for poisoning Rating of the most effective and safe sorbents that help with poisoning and hangover syndrome.