The causative agent of Creutzfeldt-Jakob disease and routes of infection
Pathology provoked by prions, which includes Creutzfeldt-Jakob disease (CJD), manifests itself as a severe degenerative process in the nervous system of not only humans, but also animals.
The disease is based on the accumulation of altered “wrong” prion protein in the neurons of the brain. The first mention of this disease is found in the works of the German doctor Hans Gerhard Kreuztfeldt (1920). And in 1921, his compatriot Alphonse Jacob identified the disease as spastic pseudosclerosis or encephalopathy, accompanied by diffuse damage to the brain substance. He also noted a combination of mental disorders with pyramidal (paresis, paralysis) and extrapyramidal (tremor, violent movements) symptoms.
Characteristics of the causative agent of Creutzfeldt-Jakob disease
Prion protein, or PrP, is, surprisingly, a physiological component of nerve cells with a function that is still unclear. The genes responsible for its reconstruction are located on the short arm of the 20th chromosome.
The pathology is characterized by the accumulation of an altered form of this protein, which, as a result of this metamorphosis, becomes resistant to enzymes and acquires the ability to suddenly fold to form peculiar rods. In this form, it goes outside the cell, where it creates amyloid plaques.
Although prion diseases in most cases are sporadic, that is, spontaneous, they are still classified as slow infections. A similar conclusion was made possible by the fact that a healthy person can be infected with material obtained from a sick patient or animal.
The key difference between prions and viruses and bacteria is the absence of DNA or RNA, which allow microorganisms to reproduce normally. Also, this protein does not cause alertness to the immune system and is simply ignored by it, despite the cascade of pathological processes in the brain.
Prions cannot be destroyed by known antiseptic agents and methods (boiling, formaldehyde, alcohol, ultraviolet light).
In animals, the disease is most often infectious; in humans, in 90% of cases, the pathology is considered sporadic or hereditary (due to a gene mutation). The exception is kuru, a disease found only in the tribes of Papua New Guinea due to their widespread ritual of eating the brains of dead tribesmen.
Epidemiology
Creutzfeldt-Jakob disease, one of the spongiform encephalopathies, is considered the most common in the structure of this nosology and occurs in 85% of cases of prion pathologies, despite this remaining extremely rare in general - no more than one infected person per 1 million population of the planet .
The disease occurs in people of any age, men are more often affected. In the classic version, the initial symptoms manifest at 60-65 years of age, but the new form, which is “mad cow disease,” debuts much earlier - at 29-30 years of age.
Symptoms and signs of each stage of CJD
There are three stages of Creutzfeldt-Jakob disease, each with its own symptoms :
- Prodromal period - symptoms vary and occur in a third of patients. This may be a sleep disorder, lack of appetite, fatigue, weight loss, loss of libido, changes in behavior. These signs occur weeks or months before the first signs of dementia.
- Initial period . Visual disturbances, dizziness, headaches, sensory disturbances and instability occur. For the majority, this period is moderate, less often acute or subacute (faster than moderate, but slower than acute).
- Expanded period. Patients usually exhibit spastic paralysis (paralysis due to destruction of the motor nerve in the brain or spinal cord) of the extremities, a disorder of the extrapyramidal system (responsible for automatic movements, posture formation, optimal preparation of muscles for precise actions and unconditioned reflexes), tremor (fast and rhythmic body movements and limbs), rigidity (muscle stiffening). In some cases, ataxia (impaired muscle coordination, for example when walking), muscle fibrillations (not visible to the eye due to the rapidity of contraction of some muscle fibers), atrophy of the upper neurons of the brain (constant muscle tension), and decreased visual acuity are observed.
Changes occurring in the body
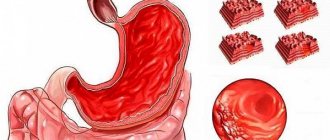
Pathological protein, multiplying and accumulating in the body, leads to:
- the development of spongiform degeneration of nerve cells, which consists of the formation of a large number of intracellular vesicles and expansion of neuron processes. These changes create a “spongy” fine-mesh effect during microscopic examination of a brain biopsy. In some cases, it cannot be detected using available research methods;
- replacement of microglia with connective tissue;
- a significant decrease in the number of neurons in the cerebral cortex, subcortical formations (basal ganglia, thalamus), cerebellum and brainstem structures;
- amyloid accumulation in 10-15% of cases.
Classification, or Main forms of Creutzfeldt-Jakob disease
Until recently, only three types of Creutzfeldt-Jakob disease were distinguished, and only about 20 years ago they started talking about a new “variant” pathology, which arose as a result of the “mad cow disease” epidemic in Western Europe. All forms of pathology have one cause - the persistence of a modified prion protein in the body. But they develop differently. The clinical picture is also somewhat different.
Classical
Classic Creutzfeldt-Jakob disease, also called sporadic, has an unclear genesis. That is, its origin has not been reliably established. It is believed that pathological prion proteins arise in the brain independently, and not under the influence of any factors. Mostly patients over 50 years of age become hostages of the disease.
The clinic debuts with impaired short-term memory, mood instability (tearfulness or laughter is quickly replaced by aggression), apathy and lack of initiative. As the pathology progresses, the patient ceases to perform even his daily duties. At the end, visual impairment, hallucinatory and speech disorders occur.
Photo: https://pixabay.com/illustrations/head-think-slide-strips-film-674124/
In 40% of patients with the classic variant of Creutzfeldt-Jakob disease, a subacute type of course and a steady progression of intellectual-mnestic disorders are detected. The same number of patients suffer from cerebellar dysfunction. And in 20% of cases, a combination of the above-described symptom complexes is observed.
Along with this, the clinical picture of the pathology is characterized by pyramidal (one-sided weakness in the arms and legs) and extrapyramidal (trembling in the limbs, involuntary movements) signs, as well as myoclonic focal seizures, that is, twitching of the facial muscles, etc. Paroxysms are triggered by loud noises, flashing lights, and even touch.
In the last phase of the disease, pronounced cognitive dysfunction is revealed. Death occurs in patients 8-9 months after the development of the first symptoms of CJD.
Hereditary
The hereditary, or familial, form of Creutzfeldt-Jakob disease, accounting for about 10% of cases of prion pathology, is associated with a mutation in the PRNP gene, which is inherited. Signs of pathology do not differ from the sporadic form.
Iatrogenic
The iatrogenic type of Creutzfeldt-Jakob disease has two ways of spreading:
- during surgical interventions involving transplantation of infected dura mater or cornea, or when using contaminated neurosurgical instruments. The incubation period will then be 1.5-4.5 years, and the disease will manifest itself as mental disorders;
- upon ingestion of growth hormone, gonadotropin, which were isolated from the pituitary gland of large livestock suffering from prion pathology. It takes from 5 to 17 years before the first clinical signs develop due to this transmission route. The disease is largely characterized by cerebellar dysfunction.
Cases of infection of doctors during surgery or autopsy are rare.
Photo: https://pixabay.com/photos/surgery-hospital-sanjay-gupta-81875/
"Variant"
In 1995, 20 cases of Creutzfeldt-Jakob disease were recorded in England and France, which developed spontaneously and had an atypical course. One of the features was that the disease debuted with mental disorders in young patients - up to 40 years old. Then cerebellar disorders were added. But cognitive disorders and myoclonic attacks appeared only at the final stage of the pathology.
There are no standard EEG patterns for this type of prion pathology described by Creutztfeldt and Jacob.
Patients usually die 7-23 months after the onset of the disease. Typical brain damage characteristic of animals made it possible to diagnose a “variant” type of nosology, such as “mad cow disease” in humans. It is believed to have been caused by the consumption of contaminated cattle meat. This discovery allowed us to conclude that the prion protein can be transmitted from one species of mammal to another, because previously this was considered impossible.
Treatment
There is no proven therapy or cure for any form of Creutzfeldt-Jakob disease.
Many potential therapeutic interventions for the disease remain currently under debate.
Treatment involves trying to keep the person living as comfortably as short as possible and reducing symptoms with medications. For example:
- Psychological symptoms such as anxiety and depression can be treated with sedatives and antidepressants.
- Other medications, such as clonazepam and sodium valproate, may be used to treat muscles and tremors.
- Opiate-based pain medications can provide effective pain relief.
Team of specialists
When someone is diagnosed with UC, they are referred to the appropriate center for diagnosis and treatment. A doctor and nurse from these services will be assigned to the patient to link with local services such as a GP, social worker, physiotherapist and occupational therapist.
Teams of specialists are available to diagnose and provide clinical and emotional support to patients and their families, and work alongside the local care team. The local care team may include doctors and nurses, occupational therapists, nutritionists, continence consultants and social workers.
Care and support
As the disease progresses, people with Creutzfeldt-Jakob disease will require significant care and practical support.
In addition to assistance with feeding, bathing, and mobility, some people may need assistance with urination. The use of a catheter (a tube that is inserted into the bladder and is used to drain urine) is often required.
Many people have trouble swallowing, so they may have to feed and drink through a feeding tube.
It may be possible to treat people with UC at home, but this will depend on the progression and severity of the disease.
The pressure of caring for someone with UC can be difficult. Instead of dealing with the problem at home, many caregivers choose to use hospital services.
Clinical manifestations of Creutzfeldt-Jakob disease
A typical clinical nosology begins gradually, the severity of symptoms increases slowly. Only 10% of patients have an acute onset of pathology, which leads neurologists to think about a stroke.
Nonspecific symptoms
The disease begins with the usual symptoms characteristic of many nosologies with general intoxication syndrome.
In this case it is observed:
- headache;
- dizziness;
- constant general weakness with sleep disturbance;
- eating disorders (from unwillingness to eat at all to pathological cravings for food);
- weight loss;
- diffuse, indescribable pain in the body.
Specific symptoms
These symptoms are followed by more specific ones, depending on the predominant localization of the pathological process. If the frontal lobes of the cerebral hemispheres are mainly involved, then mental disorders are the first to develop. It all starts with a deterioration in attention, short-term memory, and thinking processes, accompanied by a general “slowness” of consciousness.
Then behavioral anomalies are added, including lack of initiative, uncriticality of one’s condition and appearance, irritability, sometimes alternating with aggression, and depression. Seizures accompanied by disorientation in space and time and visual hallucinations are also not excluded. In the end, patients experience severe dementia.
When Creutzfeldt-Jakob disease manifests itself with visual disturbances, the first complaints are double vision, blurriness of the visible picture, narrowing or loss of areas of the visual fields, and inability to recognize surrounding objects.
A third of patients at the initial stage of the disease pay attention to cerebellar symptoms, namely:
- difficulty walking due to unsteadiness;
- impaired coordination in the limbs, especially when trying to perform targeted movements, the latter is accompanied by severe tremors;
- deterioration of speech, manifested by slowing down and poor pronunciation of sounds;
- rhythmic oscillatory twitching of the eyeballs, called nystagmus.
90% of patients experience attacks of myoclonus, that is, involuntary muscle contractions that can affect not only facial muscles, but also limbs, sometimes even individual fingers. Generalized paroxysms of epilepsy usually occur only against the background of the terminal stage of the pathology.
The extrapyramidal group of symptoms that develops at the height of Creutzfeldt-Jakob disease is represented by tremor, violent movements, akinetic-rigid syndrome, accompanied by deterioration of motor activity against the background of increased muscle tone.
The late stage of the disease is characterized by akinetic mutism, when patients physically have the ability to move and speak, but simply cannot do this. The terminal stage of the pathology occurs in the form of a coma.
Photo: https://pixabay.com/photos/alone-being-alone-archetype-513525/
Possibilities of modern diagnostics in confirming the diagnosis
Increasing dementia, combined with myoclonic seizures and characteristic changes in the EEG, gives doctors the right to suspect Creutzfeldt-Jakob disease.
Diagnosis of definite CJD
At the moment, definite, probable and possible CJD is diagnosed. In the first case, you must have:
- typical clinical picture and abnormalities in the structure of the brain matter detected during biopsy and neuroimaging studies;
- modified, enzyme-resistant prion protein in the cerebrospinal fluid, detected by protein immunoblotting;
- scrappie-associated particles.
Diagnosis of probable Creutzfeldt-Jakob disease
Issued on the basis of:
- steadily developing dementia;
- pathology-specific EEG complexes – high-amplitude sharp peaks-waves that occur despite a general decrease in the electrical activity of the brain;
- the presence of at least two of the following signs (myoclonus, visual disturbances, cerebellar disorders, pyramidal and extrapyramidal signs, akinetic mutism).
Possible CJD
It is diagnosed on the basis of a combination of dementia with a characteristic clinical picture, with a duration of pathology of less than two years and the inability to perform an EEG study or the identification of atypical patterns on film.
Instrumental diagnostic methods
To confirm the diagnosis of Creutzfeldt-Jakob disease, CT or MRI is not enough.
Although data obtained using neuroimaging technologies are also useful in establishing the true cause of the disease. Thus, on MRI, pathological changes in the area of the thalamus and caudate nucleus will be observed, resembling a “honeycomb” or a sponge, as well as diffuse cortical atrophy, the severity of the latter usually does not coincide with the severity of cognitive dysfunction. CT is less sensitive in this case and can only detect atrophy of the cerebral cortex and cerebellum.
Cerebrospinal fluid analysis and tissue biopsy
With a conventional analysis of cerebrospinal fluid, apart from a slight increase in protein levels, it is not possible to identify any pathological inclusions.
If all of the listed diagnostic methods make doctors doubt the correctness of their guesses, the only reliable method remains a biopsy of brain tissue followed by histological examination. This procedure can only be performed with the consent of the patient’s closest relatives (guardians) when the patient is declared incompetent.
Photo: https://pixabay.com/photos/mri-magnetic-resonance-imaging-2813899/
Treatment of CJD pathology
There is no etiotropic (targeted) therapy. Treatment of Creutzfeldt-Jakob disease is symptomatic.
All drugs that can have a depressing effect on higher nervous activity are discontinued.
Some drugs slow the progression of the disease:
- Brefeldin A - this drug destroys the Golgi apparatus in cells, which slows down the emergence of new molecules of altered protein;
- Calcium channel blockers have a vasodilatory effect, which promotes longer survival of already damaged brain tissue.
Treatment of Creutzfeldt-Jakob disease
At this stage of research on CJD, no specific treatment for the pathology has been developed.
All therapy comes down to the use of symptomatic drugs, since standard antiviral drugs (Remantadine, interferons) have proven ineffective. You should also stop using medications that have a negative effect on the patient’s cognitive functions.
Some scientists claim that Quinacrine, an antimalarial drug, and the antipsychotic Chlorpromazine are able to inhibit the formation of a modified prion protein. But this information has not yet been confirmed in large experiments.
Among the drugs that actually have the ability to somewhat stop the pathology, the following can be distinguished:
- Brefeldin A, which destroys intracellular structures involved in the synthesis of prion proteins;
- NMDA receptor blockers (Ketamine, Phencyclidine) - a class of anesthetics most often used in animals;
- Tiloron is a synthetic immunomodulator.
Prevention
Under normal conditions, the patient is not contagious and therefore does not need to be isolated in a boxed ward. After all, the only danger is the cells of the eye, brain and spinal cord, which contain the prion protein. That is, the patient’s immediate environment has nothing to fear.
There is no specific prevention of CJD, but this does not replace typical general infectious precautions: wearing gloves, washing hands after contact with the patient. Instruments used during neurosurgical interventions in such patients require special treatment. Ideally, needles and electrodes should be destroyed or subjected to long-term autoclaving.
Photo: https://pixabay.com/photos/hands-soap-bubbles-hygiene-wash-2238235/
Causes of the disease
In fact, there is only one reason - abnormal proteins (prions). Interesting information: prions are unique in nature, their peculiarity is that they are more likely not substances, but, oddly enough, living organisms that can reproduce in the absence of DNA and RNA.
Despite the fact that the disease is directly associated with the consumption of low-quality beef meat, in fact there are several reasons for its occurrence:
- Spontaneous disease - when an illness affects a person for no apparent reason,
- Genetics - most patients belong to the category of “hereditary”, that is, a tendency to the disease was observed in the family before,
- Infection - in this case, the cause of development is the direct entry of pathogenic bacteria directly into the human blood.