The behavior of animals is often unpredictable, and careless interaction with them can result in bites. Most often, victims consult a doctor with dog bites. In most cases, the culprits of the incident are other people's dogs, but pets often get their teeth into their owner.
According to statistics, dog bites account for more than 90% of all animal bites. According to unofficial data, in Moscow alone, about 35 thousand people suffer from dog bites every year. It is very important to remember about infection prevention and to get tetanus and rabies vaccinations if you are bitten.
1 Dog bite. First aid
2 Dog bite. First aid
3 Dog bite. First aid
Types of bites
As a result of an attack by a dog (as well as other animals), both superficial and lacerated bites can occur.
With a superficial bite, the dog only pierces the skin with its teeth, and a puncture wound appears.
With a lacerated dog bite, not only more serious damage is observed, but also greater blood loss.
Most often, the dog tries to bite the following parts of the body: forearms, palms, thighs and ankles. When bitten by dogs, in addition to wounds and scratches, damage to tendons, blood vessels and nerves may occur.
Children's shoulders and face may be injured when attacked by “four-legged friends.” But it is especially dangerous when a dog bite hits the head or neck area. This can lead to internal bleeding, open and depressed skull fractures, and in some cases, death.
Symptoms of a dog bite
The main symptoms of a bite are bleeding and pain. If therapeutic measures are not taken, the wound may become infected.
Pay attention to the following signs of infection:
- increased body temperature;
- swollen lymph nodes;
- attacks of fever;
- swelling of the wound, pain and burning sensation in it.
The consequences of a bite from a dog, as well as from a cat and other animals, can be rabies and tetanus. Therefore, it is important to immediately seek help from a traumatologist at the nearest emergency room.
Causes of rabies in humans
The cause of the disease can be either a bite or contact with the saliva of a sick animal on the skin. In nature, the virus circulates among foxes, wolves, dogs, cats, bats, horses, sheep, cows and many other animal carriers.
Medical personnel can become infected from a patient if his saliva, tear fluid or other secretions come into contact with damaged skin or mucous membranes. Therefore, you can only work with such patients in a protective suit and mask.
What is rabies?
Rabies (or rabies, from the Latin word rabies, hydrophobia, fear of water) is an acute infectious disease resulting from the bite of a dog or other infected animal, which is characterized by severe damage to the nervous system and usually ends in death.
The danger of rabies was known in ancient times, but there were no treatment methods, and every victim was doomed to death.
Only the great French scientist Louis Pasteur managed to create a vaccine against rabies (rabies vaccine) in 1885. On July 6, 1885, he saved the life of a 15-year-old teenager who was bitten by a rabid dog.
How does rabies become infected?
The causative agent of rabies is the Neuroiyctes rabid virus, which contains a single strand of RNA. The virus is resistant to freezing, antibiotics and phenol, drying, and direct sunlight. Destroyed by heat, acids and alkalis.
When a dog (or other animal) bites, infection occurs as a result of saliva from a rabid animal entering the wound. Once under the skin, the rabies virus quickly reaches the central and peripheral nervous systems. The rate of spread of the disease depends on the location of the wound (the higher the bite site, the faster the infection), the depth and size of the wound, and the reactogenicity of the human body (i.e., the susceptibility of the nervous system to a given pathogen).
1 Dog bite. First aid
2 Dog bite. First aid
3 Dog bite. First aid
Symptoms of rabies
The incubation period lasts from 1 to 3 months (sometimes from 12 days to a year). The speed of spread is influenced by the location of the bite.
There are 3 stages of the disease: initial (depression), stage of excitement, stage of paralysis.
Stage 1 of rabies:
- unpleasant sensations at the site of the bite with irradiation to the center, itching, hyperesthesia of the skin, although the wound may already have healed;
- sometimes inflammation reappears at the wound site, the scar becomes red and swollen;
- if the bite is on the face, then olfactory and visual hallucinations are observed;
- general weakness, headaches;
- nervousness and irritability;
- disruption of the gastrointestinal tract (decreased appetite, nausea, vomiting);
- constant increase in temperature to 37-37.5 degrees;
- disruption of the nervous system (sadness, fear, anxiety, apathy, nightmares);
- severe sensitivity of vision and hearing (ordinary sound or light begins to interfere).
Stage 2 of rabies - agitation (lasts from 2 to 4 days):
- the appearance of anxiety, increased heart rate;
- difficulty breathing and swallowing;
- the appearance and intensification of hydrophobia (fear is caused by the splashing, murmur, transfusion of water, its appearance, etc.);
- fear of light, loud sounds, open air (accompanied by muscle spasms and twitching, breathing problems);
- convulsions;
- attacks of aggression (a person scratches, bites, spits, fights, hits walls);
- disturbance of reason (appearance of delusional ideas, visual and auditory hallucinations).
After the attack passes, the person calms down and feels good.
Stage 3 rabies:
Symptoms of rabies at the stage of paralysis are associated with loss of activity of the subcortical formations and cerebral cortex, manifested in a weakening of sensory and motor functions.
The attacks stop. Body temperature rises to 40-42 degrees, hypotension and tachycardia appear. Death can occur within a day due to paralysis or cardiac arrest.
Diagnosis of rabies in humans
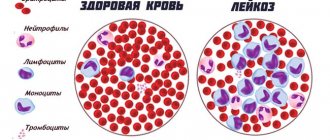
The diagnosis is made clinically, based on characteristic symptoms and medical history (animal bite). An analysis of the cerebrospinal fluid is prescribed, in which a slight increase in protein concentration and the number of lymphocytes is noted.
Additional diagnostic methods:
- virological study by infecting newborn mice with sick biomaterial;
- PCR is the most accurate rabies test for detecting genetic viral material;
- determination of virus antigen and antibodies by enzyme immunoassay.
Blood tests look for signs of dehydration, and a chest X-ray may reveal pneumonia.
Why should you contact the Mama Papa Ya clinic?
The network of family clinics “Mama Papa Ya”, whose branches are located in different districts of Moscow, provides services for the prevention of rabies through vaccination. To get vaccinated, you need to make an appointment with a therapist or pediatrician, and then get an injection there. Advantages of our clinic:
detailed consultation with a specialist before vaccination;
- the opportunity to visit an allergist for relevant diseases;
- various laboratory diagnostics;
- affordable prices and no queues.
For more detailed information, make an appointment with a specialist by phone or on our website.
Reviews
Good clinic, good doctor!
Raisa Vasilievna can clearly and clearly explain what the problem is. If something is wrong, she speaks about everything directly, not in a veiled way, as other doctors sometimes do. I don’t regret that I ended up with her. Anna
I would like to express my gratitude to the staff of the clinic: Mom, Dad, and me. The clinic has a very friendly atmosphere, a very friendly and cheerful team and highly qualified specialists. Thank you very much! I wish your clinic prosperity.
Anonymous user
Today I had a mole removed on my face from dermatologist I.A. Kodareva. The doctor is very neat! Correct! Thanks a lot! Administrator Yulia Borshchevskaya is friendly and accurately fulfills her duties.
Belova E.M.
Today I was treated at the clinic, I was satisfied with the staff, as well as the gynecologist. Everyone treats patients with respect and attention. Many thanks to them and continued prosperity.
Anonymous user
The Mama Papa Ya clinic in Lyubertsy is very good. The team is friendly and responsive. I recommend this clinic to all my friends. Thanks to all doctors and administrators. I wish the clinic prosperity and many adequate clients.
Iratyev V.V.
We visited the “Mama Papa Ya” Clinic with our child. A consultation with a pediatric cardiologist was needed. I liked the clinic. Good service, doctors. There was no queue, everything was the same price.
Evgeniya
I liked the first visit. They examined me carefully, prescribed additional examinations, and gave me good recommendations. I will continue treatment further; I liked the conditions at the clinic.
Christina
The doctor carefully examined my husband, prescribed an ECG and made a preliminary diagnosis. She gave recommendations on our situation and ordered additional examination. No comments so far. Financial agreements have been met.
Marina Petrovna
I really liked the clinic. Helpful staff. I had an appointment with gynecologist E.A. Mikhailova. I was satisfied, there are more such doctors. Thank you!!!
Olga
Prevention of rabies
With timely medical care, the disease will not develop.
Prevention of rabies in humans includes primary immunization and post-exposure prophylaxis. Rabies vaccination is given to healthy people of certain professions - veterinarians, hunters, foresters, taxidermists, dog catchers. For this purpose, an anti-rabies vaccine is used.
Post-exposure prophylaxis – measures after a bite or saliva of a sick animal gets on damaged human skin:
- immediately wash the wound with water and soap for 15 minutes, then treat with 70% alcohol;
- All victims are given a rabies vaccine.
In addition, some groups of patients are given anti-rabies injections containing rabies immunoglobulin. These are specific antibodies that immediately begin to resist the pathogen that enters the blood. Immunoglobulin is administered for percutaneous bites or scratches, contact with saliva of damaged skin or mucous membranes, as well as for injuries received from bats. If the skin is not bitten, there are only small scratches, then such immunoglobulin is administered only to patients with immunodeficiency.
Vaccinated patients also receive injections after an animal bite, but their dosage and quantity are reduced in accordance with the instructions.
Who is at risk?
- People who have been bitten by wild or domestic animals;
- People living in rural areas and keeping animals at home that have not been vaccinated against rabies;
- People who travel to developing countries (Southeast Asia, Africa);
- People who go outdoors and come into contact with wild animals (raccoons, foxes, bats, etc.);
- Trappers and hunters;
- Veterinarians;
- People who work in nurseries, zoos, animal shelters;
- People who work with the rabies virus in the laboratory.
Treatment of rabies in humans
There is no drug that destroys this virus. Therefore, treatment of rabies is symptomatic, designed only to improve the patient’s condition. Whether he survives or not depends on the severity of the disease and the condition of the body.
The patient is placed in a dark, quiet room, a tracheostomy is performed, a urinary catheter is inserted, and tube feeding is established. The following groups of medications are used:
- anticonvulsants and sedatives;
- supporting heart function;
- replenishing the volume of fluid in the blood and eliminating intoxication.
If necessary, artificial ventilation is performed.