Key Facts
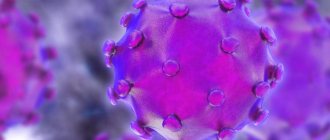
- Hepatitis B is a viral infectious disease that affects the liver and occurs in acute or chronic form.
- Transmission of the virus most often occurs perinatally from mother to child, as well as through contact with blood or other biological fluids, in particular during sexual contact with an infected partner, unsafe injection practices, cuts with piercing instruments in medical practice and in domestic conditions, and also among people who inject drugs.
- WHO estimates that in 2022, there will be 296 million people worldwide living with chronic hepatitis B (i.e. positive for hepatitis B surface antigen).
- An estimated 820,000 people died from hepatitis B in 2022, primarily as a result of hepatitis-related liver cirrhosis and hepatocellular carcinoma (primary liver cancer).
- As of 2022, 30.4 million (10)% of all people living with hepatitis B were aware of their infection, and 6.6 million (22%) of all diagnosed patients were receiving treatment. According to the latest WHO estimates, in 2022 the proportion of children under five years of age with chronic hepatitis B has fallen to just under 1%, compared with the decades before the introduction of vaccination (i.e. from the 1980s to the early 2000s). x years) this figure was about 5%.
- According to WHO estimates, in 2022, despite the availability of a highly effective vaccine, the number of people primarily infected with hepatitis B was about 1.5 million people.
- Hepatitis B is preventable through safe, accessible and effective vaccines.
Hepatitis B is a potentially life-threatening infectious liver disease caused by the hepatitis B virus (HBV). This disease is a major health problem worldwide. The infection can become chronic with a high risk of death from cirrhosis and liver cancer.
There is a safe and effective vaccine that provides 98–100% protection against hepatitis B. Prevention of viral hepatitis B helps prevent the development of complications such as chronic hepatitis and liver cancer.
General information
Hepatitis B (HVB) is a viral infection of the liver that can cause both acute and chronic illness.
The virus is transmitted through contact with the blood or other body fluids of an infected person. The hepatitis B virus can survive outside the body for at least 7 days. During this time, the virus is still capable of causing infection if it enters the body of a person not protected by the vaccine.
Hepatitis B is one of the global health problems. The virus can lead to the development of chronic liver disease and pose a high risk of death from cirrhosis and liver cancer. WHO estimates that about 2 billion people worldwide have been infected with the virus, and more than 350 million people are sick.
Approximately 780,000 people die each year from this infection—650,000 from chronic cirrhosis and liver cancer and another 130,000 from acute hepatitis B.
Hepatitis B is a serious occupational risk for healthcare workers.
However, the disease can be prevented with the currently available safe and effective vaccine, which has been used successfully since 1982. Its effectiveness in preventing infection and the development of cirrhosis, as well as primary liver cancer due to hepatitis B is 95%, which is why at one time it was called “the first vaccine against cancer.”
Diagnostics
Based on the clinical picture alone, it is impossible to differentiate between hepatitis B and other types of viral hepatitis; Therefore, laboratory confirmation of the diagnosis is extremely important. Several laboratory blood testing methods are available to diagnose and monitor patients with hepatitis B. They can be used for differential diagnosis of acute and chronic infections.
Methods for laboratory diagnosis of infection include detection of hepatitis B surface antigen (HbsAg). To ensure blood safety and prevent accidental transmission of the virus to recipients of blood products, WHO recommends systematic testing of donated blood for hepatitis B.
- Acute HBV infection is characterized by the presence of hepatitis B virus surface antigen (HBsAg) and antibodies to core antigen (HBcAg) - class M immunoglobulins (IgM). During the initial phase of infection, patients also develop hepatitis B virus e antigen (HbeAg). HBeAg is usually a marker of high levels of viral replication. The presence of HBeAg indicates the highly contagious nature of the blood and biological fluids of the infected person.
- Chronic infection is characterized by the persistence of HBsAg for at least six months (with or without the simultaneous presence of HBeAg). The persistent presence of HBsAg is a major marker of the lifetime risk of developing chronic liver disease and liver cancer (hepatocellular carcinoma).
Chance of getting sick
In areas with a high prevalence of HBV, the virus is most often transmitted from mother to child during childbirth or from person to person in early childhood. Transmission of infection during the perinatal period or early childhood can also lead to the development of chronic infections in more than one third of those infected.
Hepatitis B is also spread through cutaneous or mucosal exposure to infected blood or various body fluids, as well as through saliva, menstrual, vaginal secretions and seminal fluid. Sexual transmission of hepatitis B can occur.
Transmission of the virus can also occur through the reuse of syringes and needles, either in health care settings or among injection drug users. In addition, infection may occur during medical, surgical or dental procedures, tattooing, or the use of razor blades or similar objects contaminated with infected blood.
Despite the fact that Russia is a country with a moderate rate of hepatitis B infection, the risk of becoming infected with this virus throughout life for each of us is 20-60%.
Symptoms
The incubation period for hepatitis B lasts on average 75 days, but can increase to 180 days. The virus can be detected 30-60 days after infection.
During the acute infection stage, most people do not experience any symptoms. However, for some, acute hepatitis B infection may cause symptoms that last several weeks, including yellowing of the skin and eyes (jaundice), dark urine, extreme tiredness, nausea, vomiting, and abdominal pain. A relatively small number of patients with acute hepatitis may develop acute liver failure, often leading to death (fulminant hepatitis).
In some people, the hepatitis B virus can also cause a chronic liver infection that can later develop into cirrhosis or liver cancer.
Complications after an illness
Hepatitis B is dangerous because of its consequences: it is one of the main causes of liver cirrhosis and the main cause of hepatocellular cancer of the liver. The likelihood that hepatitis B virus infection will become chronic depends on the age at which a person acquires the infection. Children most likely to develop chronic infections are those infected before the age of six:
- chronic infections develop in 80-90% of children infected during the first year of life;
- Chronic infections develop in 30-50% of children infected before the age of six.
- 15-25% of adults who become chronically infected during childhood die from liver cancer or cirrhosis.
Among adults:
- Chronic infections occur in <5% of infected, otherwise healthy adults;
- 20%-30% of chronically infected adults develop cirrhosis and/or liver cancer.
The probability of complete recovery from chronic hepatitis B is very low - about 10%. But a state of relative health (remission), in which the virus practically does not bother the patient, can be achieved in more than 80% of cases.
Viral hepatitis B
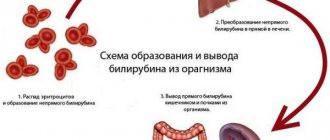
The causative agent of viral hepatitis C is a DNA genomic virus of the Orthohepadnavirus genus of the Hepadnaviridae family. Particles of three morphological types circulate in the blood of patients with viral hepatitis B. Spherical particles are most often found, thread-like forms are less common. Viral particles of these types do not exhibit infectious properties. Only 7% of particles are represented by complex two-layer spherical formations with a complete structure (the so-called Dane particles), exhibiting pronounced infectivity. Their upper layer forms a supercapsid. The genome is represented by an incomplete (one strand shorter) double-stranded circular DNA molecule and an associated DNA polymerase. Virions have four antigens: surface (HBsAg) and three internal (HBeAg, HBcAg and HBxAg). The main antigens of Dane particles are surface HBsAg and core HBcAg . Antibodies against HBsAg and HBcAg appear during the course of the disease. An increase in the titer of antibodies against HBcAg is directly related to the formation of antiviral immune reactions; HBcAg (core, or core, antigen) plays an important role in the reproduction of the virus. During an infectious process, it is detected only in the nuclei of hepatocytes. HBeAg is localized not only in the core of the virus, it circulates in the blood in free form or associated with antibodies. It is defined as an infectivity antigen. HBsAg (surface antigen) determines the ability for long-term persistence of the virus in the body; it has relatively low immunogenicity, heat stability, and resistance to proteases and detergents. There are several known subtypes of HBsAg, differing in subdeterminants: adw, adr, ayw, ayr. The common antigenic determinant is a determinant, therefore post-vaccination immunity is protective against any subtype of the virus. In Ukraine, mainly subtypes ayw and adw are registered. The clinical manifestations of the disease do not depend on the subtype of the virus. HBxAg remains the least studied. Presumably it mediates malignant transformation of liver cells.
The hepatitis B virus is extremely stable in the external environment. It persists in whole blood and its preparations for years. The virus antigen is found on bedding, medical and dental instruments, and needles contaminated with blood serum (when stored for several months at room temperature). The virus is inactivated after autoclaving at 120 °C after 45 minutes, sterilization with dry heat at 180 °C after 60 minutes. Hydrogen peroxide, chloramine, and formalin have a detrimental effect on it.
The source of infection is persons with manifest or subclinical forms of the disease (patients with acute and chronic hepatitis, with cirrhosis of the liver and so-called “healthy” virus carriers). The virus appears in the patient’s blood long before the onset of the disease (2-8 weeks before the increase in aminotransferase activity) and circulates throughout the entire acute period of the disease, as well as in chronic carriage, which occurs in 5-10% of cases. According to experts, there are 300-350 million virus carriers in the world, each of which poses a real threat as a source of infectious agents. The infectivity of sources of infection is determined by the activity of the pathological process in the liver and the concentration of hepatitis B viral antigens in the blood.
Mechanism of transmission of viral hepatitis B. Isolation of the virus with various biological secretions (blood, saliva, urine, bile, tears, breast milk, sperm, etc.) determines the multiplicity of transmission routes. However, only blood, semen and, possibly, saliva pose a real epidemiological danger, since in other liquids the concentration of the virus is very low. The disease is transmitted mainly parenterally through blood transfusions and blood substitutes, and through the use of medical instruments without sufficiently effective sterilization. The percentage of post-transfusion viral hepatitis B has decreased significantly in recent years. It is still common for patients to become infected during various therapeutic and diagnostic procedures, accompanied by a violation of the integrity of the skin or mucous membranes (injections, dental procedures, gynecological examination, etc.).
Natural transmission mechanisms include contact (sexual) transmission, as well as transmission of the virus through various contaminated household items (razors, toothbrushes, towels, etc.) when the pathogen enters the body through microtraumas on the skin and mucous membranes. Infection also occurs as a result of tattooing, piercing the earlobes and other manipulations. The sexual route of transmission of viral hepatitis B is realized through homo- and heterosexual contacts: the virus penetrates through microtraumas of the mucous membranes during sexual intercourse. The contact and household route of transmission of infection is intrafamily infection, infection in organized groups of children and adults. The main danger is posed by carriers of viral hepatitis B during close communication in these groups.
Vertical transmission of the pathogen is also possible. Typically, infection occurs during childbirth, but infection of the fetus is possible in the uterus when the placenta ruptures. The risk of transmission of infection increases tenfold if a woman has not only HBsAg, but also HBeAg. If special preventive measures are not taken, viral hepatitis B becomes infected in up to 90% of children born to virus-carrying mothers.
The share of natural routes of infection is 30-35% and tends to increase. A serious danger is posed by the spread of viral hepatitis B in groups where children stay around the clock: in orphanages, orphanages, boarding schools. These children, as a rule, have a complicated medical history and are often subjected to parenteral therapeutic and diagnostic procedures. The threat of infection with viral hepatitis B also exists for medical workers in orphanages caring for children.
Natural receptivity is high. It is known that blood transfusion containing HBsAg leads to the development of hepatitis in 50-90% of recipients, depending on the infectious dose. Post-infectious immunity is long-lasting, possibly lifelong. Repeated cases of disease are observed extremely rarely.
The main epidemiological signs of viral hepatitis B. Viral hepatitis B is one of the most common infectious diseases. It is believed that about 2 billion people are infected with the virus, and about 2 million patients die every year. The annual economic loss caused by the incidence of viral hepatitis B in Ukraine and the CIS countries is about $100 million. In the later stages of the disease, there is a risk of developing a tumor and cirrhosis of the liver, especially in people infected in childhood. In some countries, the hepatitis B virus is responsible for 80% of all cases of primary hepatocellular carcinoma. Viral hepatitis B accounts for about half of all clinical hepatitis, and the mortality rate from acute viral hepatitis B is about 1%.
The incidence of viral hepatitis B is mainly associated with poor social and economic living conditions. The entire world can be divided into regions of high, intermediate and low endemicity. Among “healthy” carriers, there is a significant percentage of undetected asymptomatic forms of infection. There is every reason to believe that the latent epidemic process with viral hepatitis B exceeds the manifest one in its intensity and rate of increase in indicators.
The young working population is intensively involved in the epidemic process: among the sick, people aged 15 to 30 years predominate, accounting for about 90% of the sick. This age composition of hepatitis patients is due to the fact that the structure of infection routes is dominated by “drug addicts” and sexual transmission of the infection. Young people under 30 years of age who used drugs account for 80% of those who died from viral hepatitis B. A significant portion of deaths (up to 42%) are caused by simultaneous infection with viral hepatitis B, viral hepatitis C and viral hepatitis D. Currently in our country The problem of parenteral hepatitis is essentially turning from a medical one into a social one.
Among the cases, the majority of patients were those who had undergone blood transfusions and other medical parenteral procedures. Risk groups include medical workers who, in the course of their professional activities, come into contact with blood and its preparations (surgeons, dentists, hemodialysis workers, laboratories, etc.), as well as drug addicts (especially in recent years) when using a single syringe and transmitting sexually transmitted infections from each other by. The incidence is characterized by a familial nature, where sexual and contact routes of infection are actively implemented. Different main routes of infection predominate in different regions of the world. In highly developed countries with an initially favorable epidemic situation, more than 50% of new cases of viral hepatitis B are caused by sexual transmission of infection. Adolescents and young adults, due to their active sexual life, constitute a group at a particularly high risk of contracting viral hepatitis B. In regions with low endemicity, infection through parenteral or percutaneous routes is of great importance in the transmission of the hepatitis B virus. In regions with high endemicity, the most common route of transmission is perinatal infection of the child from the mother. Approximately 5-17% of pregnant women are carriers of the hepatitis B virus.
Treatment
Medical care for hepatitis B is aimed at maintaining comfort and a rational combination of nutrients, including replacing fluid lost as a result of vomiting and diarrhea. People with chronic hepatitis B who need treatment can be treated with medications, including oral antivirals (such as tenofovir and entecavir) and interferon injections. Treatment of hepatitis B may slow the progression of cirrhosis, reduce the incidence of hepatocellular carcinoma, and improve long-term survival. However, in many resource-poor areas, access to such treatment is difficult.
Liver cancer is almost always fatal and often occurs in people who are in their prime productive years and are providing for their families. In developing countries, most people with liver cancer die within months of diagnosis. In high-income countries, surgery and chemotherapy can prolong life by several years. Patients with cirrhosis sometimes undergo liver transplants, with varying degrees of success.
Effectiveness of vaccination
As of 2013, 183 Member States were vaccinating infants against hepatitis B as part of their national vaccination schedules, and 81% of children had received hepatitis B vaccination. This represents significant progress compared to 31 countries in 1992, when the World Assembly Health Council adopted a resolution recommending global vaccination against hepatitis B.
Additionally, as of 2013, 93 Member States have introduced hepatitis B dose provision at birth. Since 1982, more than one billion vaccine doses have been used worldwide.
In many countries where typically 8% to 15% of children had chronic hepatitis B virus infection, vaccination has reduced rates of chronic infection among immunized children to less than 1%.
Vaccines
Expert opinion
CM. Harit
Professor, Doctor of Medical Sciences, Head of the Department of Prevention of Infectious Diseases, Research Institute of Children's Infections
Hepatitis B is contracted everywhere equally through blood (everyone) and through sexual contact (teenagers and adults). A drop of blood is so small that you cannot see it and it is already contagious, so families become infected through toothbrushes, razors, etc...
The basis for preventing hepatitis B is vaccination. WHO recommends that all infants should receive hepatitis B vaccine as soon as possible after birth, preferably within 24 hours. If a child does not receive this vaccination in the maternity hospital, the risk of infection increases significantly, and if a newborn is infected during the neonatal period, liver cirrhosis develops in adolescence or early adulthood.
The dose given at birth should be followed by two or three subsequent doses to complete the vaccination series. In most cases, one of the following two options is considered optimal:
- A three-dose hepatitis B vaccination regimen, in which the first dose (of monovalent vaccine) is given at birth and the second at 1 month of age, which is also very important, since this dose minimizes the risk of infection of the child from infected family members. The third dose (of monovalent or combination vaccine) is administered at 6 months, simultaneously with the DTP vaccine, which determines the duration of immunity against hepatitis B.
- A four-dose regimen in which the first dose of monovalent vaccine given at birth is followed by 3 doses of monovalent or combination vaccine, usually given along with other vaccines as part of routine childhood immunization, is indicated for children born to mothers infected or with hepatitis B.
After a full series of vaccinations, more than 95% of infants, children of other age groups and young adults develop protective antibody levels. Protection lasts for at least 20 years and possibly a lifetime.
More about vaccines
Contraindications to vaccination and undesirable effects from administration
Immunologists call the hepatitis B vaccine one of the safest. Adverse reactions are rare and usually do not require medical attention. The most common include:
- soreness, redness and thickening of the skin at the injection site;
- mild malaise, weakness, flu-like symptoms.
The only absolute contraindication to the administration of the drug is intolerance to yeast and other components or a registered exacerbation of chronic diseases due to previous administration.
Temporary contraindications are:
- acute infectious and other diseases;
- exacerbation of chronic (including skin) diseases;
- pregnancy.
For children with frequent acute respiratory viral infections, according to the order of the Ministry of Health, the drug is administered after 5-10 days from the relief of acute symptoms of infection. Residual effects (runny nose, cough) are not classified as contraindications.
Clinical studies confirm that the incidence of adverse events such as muscle pain and fever in the group of patients receiving vaccination did not differ from those receiving placebo. Data on allergic reactions are rare. In addition, studies deny the connection between vaccination and the subsequent development of systemic diseases, diabetes, and arthritis.
Some pediatricians do not recommend vaccinating a newborn baby with signs of physiological jaundice and postpone the first vaccination until the age of 1 or 2 months. However, it has been proven that vaccination against hepatitis B does not affect the duration or severity of the syndrome and does not have a toxic effect on the liver. Therefore, physiological jaundice is not considered a contraindication for child immunization.
Due to the impossibility of conducting clinical studies among pregnant women, this category of people is vaccinated only in special cases - for example, if it is necessary to travel to a region unfavorable for hepatitis B. Formally, before pregnancy, a woman must already be vaccinated three times according to the standard regimen. If she did not have time to complete the vaccination as scheduled, the last portion of the vaccine can be administered after birth. The exception is situations in which there is a high probability of infection. Breastfeeding is not a contraindication to the administration of the drug.