Causes of cardiosclerosis
1. Functional disorders:
- Damage to the heart muscle as a result of inflammatory diseases.
- Hypoxia due to insufficient blood supply to the heart muscles due to narrowing of large cardiac vessels.
- Stretching of the walls of the heart, which leads to an increase in its volume.
2. Lifestyle and bad habits of the patient:
- Alcohol abuse and smoking.
- No, minimal or excessive physical activity.
- Repetitive stress.
- The habit of overeating and, accordingly, excess body weight.
Hereditary factors play an important role in the occurrence of the disease.
Causes
The following factors play an etiological role in the development of atherosclerotic cardiosclerosis. Age. Most cases of the disease occur in people over 50 years of age. As the body ages, the activity of elastase, the production and breakdown of cholesterol, and the concentration of acidic mucopolysaccharides increase.
Gender. In men, atherosclerosis develops more often and at an earlier age. In women, under the influence of sex hormones, beta lipoproteins are formed more slowly, and the concentration of alpha proteins, on the contrary, increases, which is why the risks of atherosclerosis are reduced. Smoking. The effect of nicotine on vascular permeability is extremely negative, since with this type of intoxication the production of adrenaline sharply increases, the synthesis of bradykinin is stimulated, and damage to the walls increases.
Hereditary predisposition. Type 3 lipid metabolism disorders mainly occur in families with coronary artery disease and hypertension. But according to Mendel's laws, only type 2 is inherited. Sedentary lifestyle. It has long been recognized by everyone that movement is one of the components of health. The higher a person’s activity, the better the compensation mechanisms and collaterals (bypass paths of blood flow) in his body.
Tendency to overeat. The calorie content of food consumed should not exceed the body's needs, since abundant nutrition will lead to obesity and all related problems. To avoid the development of diseases, you should not be guided by appetite - you need to eat food based on the calories expended.
Eating fatty and high-calorie foods in large quantities leads to increased cholesterol
In addition to predisposing general factors that can lead to the appearance of atherosclerosis, there are several diseases that also provoke and accelerate the pathological process. This list includes:
- arterial hypertension (all types);
- diabetes;
- obesity;
- hypothyroidism;
- gout.
In this case, it is customary to pay attention to the risk factors present for pathology, which imply various changes in the biochemical and clinical parameters of the body, bad habits and the presence of concomitant diseases. They are divided into:
- the main ones are arterial hypertension, hypercholesterolemia (increased cholesterol in the blood) and nicotine intoxication;
- additional – sedentary lifestyle, diabetes, obesity, gout.
Classification of cardiosclerosis
According to the morphological principle, focal (most often occurs as a complication after myocardial infarction and myocarditis) and diffuse cardiosclerosis, in which the connective tissue spreads to the entire myocardium, are distinguished.
For etiological reasons, the following types are distinguished:
- Post-infarction. As a result of myocardial infarction, scars form at the site of necrotic damage, which reduces the contractility of the heart muscle. The more cases of myocardial infarction a patient has suffered, the more scar tissue is formed. The threat of chronic aneurysm increases due to protrusion of the walls of the heart muscle, which is stretched and weakened by connective tissue. Aneurysm rupture is associated with high mortality.
- Myocardial. Myocardial inflammation develops mainly in young patients with chronic allergic and infectious diseases. With this form, the right ventricle of the heart increases in volume and is insufficiently supplied with blood.
- Atherosclerotic. As a rule, it is the result of atherosclerosis of the coronary vessels and coronary heart disease. This form of the disease develops over a long period of time, because due to damage to blood vessels, heart cells do not receive enough oxygen, hypoxia develops, the course of coronary heart disease is complicated, and cholesterol levels increase. This leads to diffuse cardiosclerosis, which is accompanied by arrhythmia.
Typology of the disease
Today, two approaches to the classification of cardiosclerosis are proposed. The first relies on the history of the disease and proposes to subdivide it into atherosclerotic and myocardial. The second approach is based on the localization of the disease, depending on which cardiosclerosis can be either diffuse or focal. Let's look at these terms in more detail:
- The atherosclerotic form of the disease got its name in honor of the pathology that causes it - atherosclerosis of the arteries.
- Myocardial cardiosclerosis is a direct consequence of various types of myocarditis.
- The diffuse type of the disease is diagnosed when necrosis affects muscle tissue relatively evenly.
- In focal cardiosclerosis (also known as scar), connective tissue replaces muscle tissue in individual areas of the heart, varying in size.
Consequences of cardiosclerosis
- Aneurysms and heart defects.
- Arrhythmia.
- Thromboembolism.
- Chronic fatigue syndrome.
- Chronic heart failure.
Symptoms of cardiosclerosis
Very often the initial stages of the disease are asymptomatic. In the clinic of the onset of sclerosis, the first symptom may be arrhythmia. Typical manifestations of the diffuse form should be considered heart failure and disturbances in the rhythm of the heartbeat.
Symptoms regardless of the form (post-infarction or atherosclerotic):
- heart rhythm disturbances;
- dyspnea;
- the appearance of fluid in the abdominal and pleural cavities;
- pain in the heart area;
- increased heart rate;
- pulmonary edema;
- increase in liver size.
As the area of affected heart tissue increases, the severity of symptoms increases.
Very often the course of cardiosclerosis is accompanied by arterial hypertension. In this case, high blood pressure alternates with long periods of normal blood pressure.
Atherosclerotic cardiosclerosis
Structural heart diseases, accompanied by impaired pumping function of the organ, are a common cause of death. Particularly dangerous is the lack of blood supply to the muscular lining of the heart, which often leads to the development of diseases such as coronary artery disease, atherosclerotic cardiosclerosis and myocardial infarction. In this case, treatment of the heart vessels is a priority. We should not forget that atherosclerotic cardiosclerosis is a progressive pathology.
Atherosclerotic heart disease
In the medical literature, atherosclerotic cardiosclerosis is a structural pathology characterized by the gradual replacement of the muscular lining of the heart with connective tissue cells against the background of progressive hypoxia. There are many causes of this pathology, but atherosclerotic lesions of the coronary arteries are the main etiological factor. Atherosclerotic cardiosclerosis can cause dangerous complications such as heart failure and heart attack.
The human heart is a powerful four-chambered muscular pump that supplies all cells of the body with nutrients and oxygen. The constant movement of blood in the vessels is supported by rhythmic contractions of the myocardium. The muscular lining of the heart also requires a constant flow of blood, since cardiomyocytes are not able to accumulate enough oxygen to function autonomously. Even a slight decrease in blood flow to the myocardium leads to progressive changes and disruption of pumping function. The longer ischemia develops, the more dangerous the consequences of such a disease.
Atherosclerotic cardiosclerosis is not always considered an independent disease. As a rule, this is a consequence of a long course of coronary heart disease (CHD), inflammatory and autoimmune processes. However, replacement of normal cardiomyocytes by dysfunctional scar tissue is a major cause of myocardial dysfunction. To eliminate this pathology, first of all, treatment of the root cause of organ hypoxia is required.
8
24/7
Possible reasons
The main factor contributing to the development of cardiosclerosis is insufficient oxygen supply (hypoxia) to the muscle cells of the heart. Secondary factors include inflammatory and infectious processes, autoimmune diseases and organic myocardial damage. Under hypoxic conditions, myocardial cells first change and stop contracting, and then are destroyed.
Main reasons:
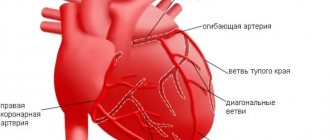
- Atherosclerosis of blood vessels is the gradual growth of fatty plaques on the inner walls of the arteries, causing a narrowing of the lumen of the vessel and a decrease in blood flow. Plaques form due to blood lipid imbalance, poor nutrition, vascular damage and other factors. With atherosclerotic disease of the coronary arteries that supply the heart, myocardial hypoxia develops.
- Coronary heart disease is a consequence of narrowing of the blood vessels of the heart. This may be atherosclerosis, dysregulation of tone, or a congenital anatomical defect of the arteries. IHD is a progressive disease that causes gradual replacement of cardiomyocytes with connective tissue. Atherosclerotic cardiosclerosis, in which angina pectoris occurs quite often, has a common mechanism of occurrence with ischemic heart disease.
- Coronary artery thrombosis is a partial or complete blockage of blood vessels.
- A heart attack is a sudden cessation of blood supply to the heart, accompanied by focal or diffuse destruction of cardiomyocytes. Destroyed muscle cells are also replaced by connective tissue.
- Pathologies of connective tissue, characterized by excessive proliferation of fibroblasts or the appearance of abnormal proteins.
Doctors are not always able to identify the real cause of atherosclerotic myocardial disease in a patient. Pathology is often detected in late stages.
Risk factors
Atherosclerotic cardiosclerosis of the heart can progress even faster under the influence of negative factors that are not the direct cause of the disease. This may be an unhealthy lifestyle, primary disorders of the cardiovascular system and other phenomena.
The main risk factors include:
- Pathologies of the heart and blood vessels in a family history.
- High blood pressure.
- Obesity and sedentary lifestyle.
- The predominance of fatty foods in the diet.
- Blood lipid imbalance (high concentration of bad cholesterol).
- Diabetes.
- Kidney diseases.
- Smoking and alcoholism.
- Use of drugs that affect the heart.
The listed factors largely determine the mechanism of development of almost any pathology of the heart and blood vessels.
Symptoms and signs
Atherosclerotic cardiosclerosis, the causes of which are usually associated with primary diseases of the heart and blood vessels, can manifest with various symptoms. First of all, these are symptoms of ischemic heart disease, myocarditis, heart attack or any other factor in the development of cardiosclerotic disease. In this case, the process of replacing cardiomyocytes with connective tissue practically does not manifest itself until the patient experiences myocardial dysfunction.
8
24/7
Possible manifestations of the disease:
- Constant fatigue, especially during physical activity.
- Hesitant breathing.
- Dizziness and headache.
- Loss of consciousness.
- Cardiopalmus.
- Feeling of heaviness in the chest area.
- Chest pain (angina pectoris).
- Swelling of the lower extremities and abdominal cavity.
- Pulmonary edema.
- Insomnia.
- Anxiety and fear.
- Violation of the rhythm of heart activity.
Thus, atherosclerotic cardiosclerosis masks its symptoms under ischemic heart disease and other primary diseases. As a result, cardiosclerotic changes are detected already at the stage of severe complications.
Diagnostic methods
Most often, atherosclerotic cardiosclerosis is an incidental diagnostic finding during a cardiac examination for ischemia, atherosclerosis or other diseases. Patients consult a cardiologist with complaints of angina, exercise intolerance, dizziness and other symptoms. The doctor reviews your history for risk factors and performs a physical examination. During listening (auscultation) of the heart and general examination, objective signs of myocardial dysfunction are often detected. The diagnosis of atherosclerotic cardiosclerosis is made based on the results of instrumental and laboratory methods.
Additional research:
- Electrocardiography – registration of the bioelectrical activity of the heart. To do this, special sensors are placed on the patient’s body connected to a cardiogram recording device. Based on the test results, one can judge the presence of a structural pathology that prevents the normal propagation of an impulse in the myocardium.
- Echocardiography is the main imaging method in cardiology. The doctor uses a transducer that sends high-frequency sound waves into the heart to produce an image. Monitoring the heart's performance on a monitor in real time allows you to detect the focus of cardiosclerosis and assess the degree of pumping dysfunction.
- Angiography – visualization of blood vessels. As a rule, this method is used to diagnose coronary artery disease, heart attack and atherosclerosis. Before taking the image, the doctor injects a contrast agent intravenously to improve the accuracy of the study. Based on the results of coronary angiography, one can judge the cause of cardiomyocyte hypoxia.
- Stress test - obtaining a cardiogram during increased heart activity. This test is most often used to diagnose hidden arrhythmia and pumping dysfunction.
- Holter study – recording of a cardiogram on an electronic device of a portable device within 24-48 hours. Before the study, the patient is instructed to keep a diary of well-being to clarify the time of occurrence of the arrhythmia. This is the optimal method for searching for manifestations of myocardial dysfunction.
- Cardiac biopsy – removal of a section of heart tissue followed by histological examination.
- Blood test for lipid profile, hormones, minerals and heart attack indicator enzymes.
- Computed tomography and magnetic resonance imaging are methods for obtaining high-resolution images of the heart and blood vessels. The images are often used to plan surgery.
- Radionuclide study - visualization of the heart with the preliminary introduction of radioactive isotopes into the bloodstream. The results of the study demonstrate the effectiveness of blood supply to the myocardium.
The abundance of diagnostic methods is justified by the number of possible etiological factors. To treat the disease, the doctor also needs to assess the degree of cardiosclerosis.
Treatment and prevention
Treatment should be aimed at eliminating the root cause of the pathology, restoring myocardial function and preventing the development of dangerous complications. Surgical and medicinal correction methods are used.
Prescribed drugs:
- Beta blockers to lower blood pressure and eliminate arrhythmias.
- Calcium channel blockers to improve blood supply to the myocardium.
- Aldosterone inhibitor to lower blood pressure.
- Diuretics to improve hemodynamics.
- Cardiac glycosides, statins and other drugs necessary to treat the cause of the pathology.
Atherosclerotic cardiosclerosis can rarely be eliminated with medication, but medications prevent the progression of the disease and eliminate symptoms.
Surgical methods:
- Implantation of a pacemaker or defibrillator.
- Correction of the coronary arteries to improve blood flow.
- Surgery for structural heart pathologies.
Prevention methods are also important. Giving up bad habits and fatty foods, losing weight, moderate physical activity and timely treatment of primary pathologies of the cardiovascular system helps prevent the development of irreversible changes in the heart. If symptoms of myocardial dysfunction appear, it is recommended to consult a cardiologist for examination.
8
24/7
At-risk groups
The risk of cardiosclerosis is highest in patients with pathologies in the development of the heart and cardiovascular diseases, as well as in people with various types of allergies.
Pregnant women can be identified as a separate group. Pregnancy causes hormonal, autonomic, metabolic and hemodynamic changes in the body of women and can act as a proarrhythmogenic factor. Complex heart rhythm disturbances are diagnosed both in pregnant women with cardiovascular pathology and in patients without changes in metabolism and the condition of internal organs.
Cardiosclerosis in children is possible against the background of myocardial pathologies, for example, inflammatory and dystrophic processes, in particular diseases of the heart muscle caused by metabolic disorders in heart cells. These biochemical disorders significantly weaken the contractile, conductive, excitatory and automatic functions of the myocardium.
Clinical signs of the disease
In the absence of treatment, when the disease begins to progress, characteristic symptoms are felt. Symptoms of myocardial cardiosclerosis:
- painful spasms behind the sternum radiating to the arm, under the shoulder blade, and epigastric zone;
- dry cough in the form of attacks with signs of suffocation;
- tachycardia that occurs for no reason, at rest;
- loss of strength, constant desire to sleep;
- shortness of breath with minor exertion;
- loss of consciousness, blurred vision;
- dizziness.
With an intensive course of the disease with obvious progression, fluid accumulates in the lungs and edema develops. Excessive growth of connective tissue leads to heart failure and atrial fibrillation. Myocardial cardiosclerosis with cardiac arrhythmia in the absence of qualified assistance can result in death.
Diagnostics
The doctor develops therapeutic regimens after additional research. The course of treatment depends on the stage of development of the pathology, timely detection of the disease or the protracted nature and neglect of the case. Upon admission of the patient, the doctor conducts a detailed examination with palpation, percussion and auscultation. Measures blood pressure and pulse, listens to complaints, asks leading questions. After studying the anamnesis, the following tests are prescribed:
- ECG - electrocardiograms to determine the work of the heart over a period of time.
- General blood tests to assess the patient's condition.
- Biochemical blood test.
- Determination of cholesterol levels in the blood.
- Echocardiography, which records scar tissue, its volume, and expansion of the heart.
- Ultrasound - to detect hypertrophy of the left ventricle of the heart muscle.
- MRI is the most informative method that allows you to examine the vascular walls and myocardium.
- Stincigraphy - showing the activity of pathology.
Daily monitoring, during which heart function is recorded for 24 hours. Only having all the research results can the doctor make a diagnosis and prescribe adequate treatment.
Methods of treating the disease
The development of science is progressing, but doctors have not yet learned how to restore degenerated heart tissue. The main task of doctors is to stop the process of destruction, maintain the function and rhythm of the heart within normal limits.
Drug treatment is necessary:
- to exclude possible complications;
- detection and elimination of negative factors provoking the disease;
- relief of the main symptoms of the disease.
To determine the course of therapy, the doctor takes into account the patient’s age, clinical picture, the presence of concomitant pathologies and the possible use of drugs to treat the root cause.
Maintenance therapy may include:
- ACE inhibitors;
- statins;
- diuretics;
- adrenaline beta blockers.
The pathology is quite serious and if you do not follow the doctor’s recommendations or change your usual lifestyle, it can end in death. It is necessary to adjust the work and rest regime, not to overload the body physically and emotionally. Eliminate all external negative influences.
Nevertheless, illness is not a reason to refuse measured physical activity, walks in park areas, and the fresh air. Sleep should be at least 8 hours a day. You should also not sleep more than 10 hours.
Cardiosclerosis medications
The European Society of Cardiology recommends the following medications for the treatment of cardiosclerosis, eliminating the symptoms of the disease, as well as its root cause:
- Antihypertensive drugs. To maintain vascular tone and normalize blood pressure, ACE inhibitors (Captopril, Enalapril, Ramipril) are prescribed; calcium antagonists (Amlodipine, Semlopin, Phenigidine), beta blockers (Atenolol, Bisoprolol, Metoprolol), antiplatelet drugs (Aspirin), lipid-lowering drugs (Simvastatin, Atorvastatin, Allesta).
- Cardioprotectors (antianginal agents). Their task is to maintain the functional activity of the heart and counteract the influence of negative exo- and endogenous factors on it. These include organic nitrates (Nitroglycerin, Isosorbide Mono- and Dinitrate); sydnonimines (Mosikor, Sidocard); metabolic agents (Trimetazidine).
- To normalize heart rate and conduction: amiodarone (Amiodarone), dronedarone (Multak).
- To normalize metabolic processes - potassium and magnesium preparations: Panangin, Asparkam, Magnerot.
- Antibiotics and corticosteroids: for myocarditis and other inflammatory processes.
Diagnosis of cardiosclerosis
To diagnose the disease, the following studies are carried out:
ECG - on it you can see the affected areas, changes in the heart, failures.
Biopsy - changes in the heart can be detected.
Angiography – this procedure is performed directly to diagnose coronary cardiosclerosis. ECHO KG - this study shows the degree of growth of pathological tissue and helps to see the functioning of the heart valves.
X-ray – allows you to see the stage of the disease and detect an aneurysm.
CT or MRI - these studies help to detect foci of growth.
Treatment of cardiosclerosis
Since it is not possible to completely cure the disease, treatment is aimed at treating complications and eliminating symptoms.
Treatment is carried out in several ways, and one of them is surgery:
A heart transplant is a complete organ transplant.
Coronary bypass surgery.
Installation of a pacemaker - this type of treatment is carried out in the presence of arrhythmia, as well as in case of disruption of the rhythm. In case of an aneurysm, an operation is performed in which the aortic aneurysm is completely removed.
Treatment with drugs:
Frequently asked questions about cardiosclerosis
Which doctor treats cardiosclerosis?
If you suspect cardiosclerosis, you should contact a cardiologist.
What signs should you see a doctor for?
High blood pressure; arrhythmia; increased fatigue and swelling of the limbs.
Can cardiosclerosis develop in children?
Cardiosclerosis in children can develop against the background of inflammatory and dystrophic processes in the myocardium - in particular, diseases of the heart muscle caused by metabolic disorders in heart cells.
Definition of pathology
When the valves and heart muscle are damaged, intensive growth of connective tissue is observed, which leads to dysfunction of contractility - a phenomenon called cardiosclerosis.
There are two forms of pathology:
- ICD 10 - code for myocardial cardiosclerosis with rhythm disturbance (120.0 - 120.9.). Usually the form develops at the site of a former source of inflammation. Developmental processes are associated with exudation and proliferation in the stroma, destruction of myocytes.
- PMC in ICD-10 - the atherosclerotic form manifests itself as a consequence of ischemic heart disease. Due to the slow degenerative process and death of fibers, it occurs with scant clinical manifestations.
The second develops against the background of an inflammatory process in the heart muscle.
It is worth noting that the disease occurs frequently, but with small areas of transformation, the disease may not manifest symptoms. It can be detected on an ECG during a random routine examination. When a large area of the myocardium is degenerated, the clinical picture indicates obvious dysfunction, serious complications appear that can end tragically.
ICD-10 with codes of myocardial cardiosclerosis 120.0 – 120.9, constitutes a large group of diseases of the circulatory system. This is a disease characterized by the proliferation of connective tissue fragments in place of muscle tissue. How the pathology will proceed is determined based on many factors. First of all, pay attention to the volume of the lesion.
Negative factors in the development of pathology
The causes of myocarditis with subsequent cardiosclerosis are as follows:
- Infectious lesions of influenza, cytomegalovirus, ECHO viruses, HIV, Epstein Barr disease, bacterial infections.
- Negative effects of beta-hemolytic streptococci, helminthic infestations, fungal infections.
- Allergic manifestations due to excessive susceptibility to the action of antibiotics, anti-tuberculosis drugs, vaccines, sulfonamides. Antihypertensive medications can also trigger the development of inflammation in the myocardium.
- Intoxication of the body with narcotic drugs, antidepressants, against the background of thyrotoxicosis.
The cause may be idiopathic in nature and have no logical explanation, but manifest itself with all the symptoms inherent in pathology.
The reasons can be layered, aggravate the problem, increase the area of tissue scarring, which contributes to the development of irreversible processes.
The degeneration of the heart muscle can be influenced by: excess weight, endocrine system dysfunction, environmental conditions, lifestyle, depressed immunity.
How much does it cost to treat cardiosclerosis in Israel?
The price for medical services at the Ikhilov clinic is one of the most affordable in the world. Taking into account the level of the medical institution and the qualifications of doctors, as well as the quality of the treatment provided, Ikhilov can be compared with the best clinics in the world, but the cost of treatment is usually 2-3 times lower than in Western Europe or America. WITH
You can find out the exact cost of treatment in this Israeli clinic by filling out the application form on this website or asking the relevant questions in the online chat. In addition, consultation on price and treatment issues is available by telephone; to do this, you need to call the specified number or request a call back.
Benefits of treatment in Ikhilov
- High treatment efficiency
- High information content and diagnostic accuracy
- Cardiac surgeons with many years of experience
- Affordable prices for medical services, no prepayments
- The most modern methods and equipment to achieve optimal treatment results
If you or your loved ones have signs of cardiosclerosis, and you would like to get a consultation with an Israeli doctor, order it today. Our medical consultant will do everything possible so that within two to three working days you can communicate directly with a cardiologist from Ikhilov.
- 5
- 4
- 3
- 2
- 1
(1 vote, average: 5 out of 5)