Acetylcysteine in the treatment of lower respiratory tract infections in adults
The inflammatory process in the lower respiratory tract (pneumonia, acute and chronic bronchitis, chronic obstructive pulmonary disease) is accompanied by a violation of mucociliary clearance, which is an important mechanism for cleansing the bronchial tree. The function of the mucociliary apparatus is the interaction of the cilia of the ciliary epithelium with the secretion of goblet cells of the epithelial lining of the bronchi and protein-mucosal glands. Foreign particles trapped in the bronchi are removed due to the movement of the cilia, which prevents the development of infection [1].
With inflammation of the respiratory tract, bronchial hyperemia develops, the number of goblet cells increases, which produce a thicker, more viscous secretion than the glands. This mucus coats the eyelashes. Due to the fact that the rheological properties of bronchial secretions change and the function of the ciliated epithelium is inhibited, the efficiency of mucociliary clearance decreases. A thick, viscous secretion collects in the bronchi, which in turn causes an increase in microbial colonization of the bronchial tree. Increased coughing does not lead to adequate cleansing of the bronchi.
For this reason, in the treatment of acute and chronic diseases of the lower respiratory tract, in addition to etiological treatment, pathogenetic therapy occupies an important place. To improve the drainage function of the bronchi and the removal of sputum, mucoactive drugs are used. There are several classifications of mucoactive drugs. For practical use, it is most convenient to distinguish two main groups of drugs used to remove sputum [2, 3]:
I. Secretomotor (stimulate expectoration).
- Reflex action (herbal remedies: thermopsis herb, marshmallow root, licorice root, coltsfoot leaves, thyme herb, etc.).
- Resorptive action (sodium iodide, potassium iodide).
II. Mucolytic (bronchosecretolytics).
- Proteolytic enzymes (trypsin, chymotrypsin, ribonuclease, etc.).
- Synthetic mucolytics (acetylcysteine, ambroxol, carbocysteine, etc.).
Secretomotor, or expectorant, agents enhance bronchial peristalsis and increase the functional activity of the ciliated epithelium of the bronchi, and increase the functioning of the bronchial glands. The action of these drugs is associated with irritation of stomach receptors and reflex stimulation of the respiratory and cough center. They are used mainly for productive coughs to improve coughing. Currently, the use of secretomotor agents that enhance expectoration (both reflex and resorptive action) is limited, especially in the presence of thick, viscous secretions, since their mucolytic effect is weak. An overdose of these drugs may cause the urge to vomit and strengthen the gag reflex. They are contraindicated for gastric and duodenal ulcers [2].
Among mucolytic drugs, proteolytic enzymes are practically not used due to the possibility of developing allergic reactions and bronchospasm.
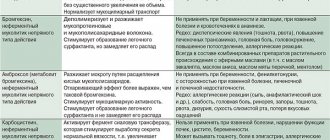
Currently, the most widely used synthetic mucolytic drugs are acetylcysteine (AC), ambroxol, carbocysteine. However, it should be noted that of these drugs, only AC has a direct mucolytic effect.
AC is a derivative of L-cysteine; its molecule contains free sulfhydryl groups. Free sulfhydryl groups break the disulfide bonds of acidic mucopolysaccharides in sputum. This leads to depolymerization of mucoprotein macromolecules and, accordingly, to a decrease in the viscosity of mucus and a decrease in its adhesion. Thus, AC improves sputum discharge through a direct effect on the rheological properties of the secretion. The mucolytic effect of AC increases with increasing sputum pH. The greatest mucolytic effect of AC is observed at pH = 7.0–9.0 [4].
An important feature of AC for practical use is the preservation of its mucolytic effect in any type of sputum - mucous, mucopurulent and purulent.
At the same time, under the influence of AC, the rate of mucociliary clearance also increases. This effect allows us to talk about AC not only as a mucolytic, but also as a mucokinetic. In addition, as a result of the action of AC, the secretion of less viscous sialomucins by goblet cells is potentiated: the sol content increases. This restores the function of the ciliated epithelium, which can independently eliminate mucus from the respiratory tract. Thus, AC also has a mucoregulatory effect [5, 6].
In recent years, studies have appeared that demonstrate the ability of AC to reduce the formation of biofilms of bacteria and fungi, as well as to destroy mature biofilms. This effect is associated with the influence of AC, as an antioxidant, on the metabolism of bacterial cells and the production of exopolysaccharides, the main component of the biofilm matrix. AC can directly destroy the disulfide bonds of bacterial enzymes that are involved in their formation or excretion [7].
Studies have also shown that AC is able to inhibit the growth of Staphylococcus aureus, Pseudomonas aeruginosa, Klebsiella pneumonia, Enterobacter spp. and other bacteria. At the same time, AC is more active than ambroxol and carbocisteine. For example, the activity of reducing the viability of Staphylococcus aureus in AC is 6–7 times higher than that of ambroxol and bromhexine [6].
This antibacterial effect is associated with competitive inhibition of the utilization of the amino acid cysteine by bacteria and the ability of the sulfhydryl groups of AC to interact with microbial proteins. It has been shown that the combined administration of antibiotics and AC increases their antibacterial effect. In experiments, this effect has been proven for antibiotics such as ciprofloxacin, rifampicin, carbenicillin, gentamicin, etc. [7].
Currently, in clinical practice, in the treatment of acute and chronic respiratory diseases, another very important property of AC is used - antioxidant and antitoxic activity.
The development of oxidative stress during inflammation is a serious factor in the pathogenesis of inflammatory lung diseases. Oxidative stress is characterized by an imbalance between oxidants and antioxidants, which is associated with an increase in the level of oxidants or a lack of antioxidant protection. At the same time, the weakness of antioxidant protection is one of the reasons for the progression of the inflammatory process in the bronchi and lungs. Oxidative stress developed during inflammation causes excessive formation of O-2, OH-, H2O2, etc. in the lung parenchyma. Increased production of oxidants leads to changes in the bronchial wall, increased contraction of smooth muscle fibers, and a decrease in the function of adrenergic receptors. As a result of oxidative stress, cell lysis develops, the permeability of the alveolar epithelium increases, and in the lung stroma there is a decrease in the synthesis of elastin and collagen. In addition, the production of pro-inflammatory cytokines increases. In this regard, antioxidants are widely used as metabolic correction agents in the treatment of pneumonia, exacerbations of chronic obstructive pulmonary disease (COPD), as well as for the prevention of complications [8, 9].
Experiments have proven that AC reduces the damaging effects of almost all of the above-mentioned oxidative stress factors. AC has both direct and indirect antioxidant effects. The direct antioxidant effect of AC is associated with the presence in its molecule of a free thiol sulfhydryl group, which easily donates hydrogen, neutralizing oxidative radicals. The indirect antioxidant effect of AC is due to the fact that it is a precursor of glutathione tripeptide, the main factor of protection against the effects of toxic internal and external agents, components of tobacco smoke and other air pollutants. Glutathione synthesis depends on the presence of cysteine. Prescribing AC to a patient ensures the supply of cysteine to maintain the required level of glutathione in the body.
A study of the action of AC in the clinic showed the ability of AC to reduce the formation of O2 initiated by tobacco smoke, inhibit the production of eosinophilic cationic protein, lactoferrin, antichymotrypsin, and also restore normal cellularity of bronchoalveolar fluid [9].
Many studies have proven that long-term use of AC at a dose of 400–600 mg per day reduces the frequency of exacerbations of chronic bronchitis, as well as moderate and severe exacerbations of COPD with an improvement in respiratory function indicators in patients [10].
No less than 9 randomized, placebo-controlled studies also showed that prophylactic administration of AC for 3–6 months in patients with COPD reduced the frequency, duration and severity of exacerbations of the disease [9]. The presented data on the effectiveness of AC in chronic lung diseases are supported by other studies. A double-blind, multicenter, placebo-controlled study conducted by the Swedish Society for Pulmonary Diseases (SSPD) proved that the incidence of exacerbations of chronic bronchitis was significantly, significantly lower - by 52.5% in the group of patients receiving AC for a long time, compared with the placebo group (p < 0.01 as assessed by investigators and p < 0.001 as assessed by study coordinators) [11]. The effectiveness of the clinical use of AC was confirmed by meta-analysis data published in 1976–1994. the results of eight double-blind, placebo-controlled studies conducted in Western Europe, which involved 1048 patients. This meta-analysis confirmed a statistically significant reduction in the frequency of exacerbations of chronic bronchitis by 23% compared with placebo with long-term, more than 3 months, oral administration of AC at a dosage of 400 to 1200 mg per day [12]. Thus, the use of AC helps reduce morbidity and healthcare costs [12].
The described properties of AC show that the drug has a wide spectrum of activity, which makes it possible to effectively use it in the treatment of pneumonia, acute and chronic bronchitis, COPD, especially when patients have viscous, difficult to separate sputum.
The effect of the drug begins quite quickly - 30-90 minutes after taking it and lasts up to 2-4 hours (for dosage forms that do not have a prolonged action). AC is prescribed 200 mg 2-3 times a day or 600 mg per day once.
The duration of treatment depends on the characteristics of the disease. For short-term colds, the duration of use is usually 5–7 days. In acute diseases (pneumonia, acute bronchitis), it is best to prescribe AC on the first day of the disease in order to prevent mucostasis and improve mucociliary clearance, prevent or reduce bronchial obstruction and microbial colonization of the respiratory tract. AC can prevent the development of oxidative stress or reduce its severity. Taking AC is also advisable to reduce the manifestations of intoxication and alleviate the course of the disease.
In case of exacerbation of chronic respiratory diseases, the duration of treatment with AC can be up to 3 weeks or more. Clinical studies have shown the advisability of prescribing acetylcysteine in higher doses - 1200 mg and 1800 mg per day - to patients with COPD, chronic bronchitis for a long time - up to 6 months or more [4].
AC should be used with caution in patients with peptic ulcer disease in the acute phase (gastric ulcer, duodenal ulcer), with hemoptysis, varicose veins of the esophagus, pulmonary hemorrhage, diseases of the adrenal glands, in patients with renal and liver failure.
AC is well tolerated. A meta-analysis of 39 studies conducted between 1976 and 1994 found no difference between AC and placebo in the incidence of gastrointestinal (GI) adverse events. When using AC, 10.2% of patients complained of adverse drug reactions from the gastrointestinal tract: dyspepsia, diarrhea, heartburn, while in the control group there were 10.9% of such patients [13].
In order to avoid unwanted effects and potentiate the effect of the drug, it is necessary to follow certain rules for taking AC.
Thus, the last evening dose of AC should be no later than 18 hours, since before bedtime the patient needs to cough and clear the airways of liquefied sputum. AC should not be used immediately before bedtime, since in a horizontal position the discharge of liquid secretions increases, which will intensify the night cough and impair sleep.
To improve the drainage function of the bronchi and more active removal of mucus, approximately 60 minutes after taking AC, the patient should cough and perform breathing exercises. Kinesitherapy and vibration massage are indicated. Their implementation is especially important in elderly patients with a reduced cough reflex and in children.
You should not take antibiotics and AC at the same time, so that the latter does not actively interact with the antibiotic. The antibiotic should be taken no earlier than 2 hours after AC. With such separate use, AC enhances the effect of the antibiotic, which, after liquefying the sputum, more easily penetrates the bronchial mucosa [6]. Compliance with the correct intake of AC ensures high effectiveness of therapy.
Thus, AC is an effective and safe drug for the treatment of lower respiratory tract infections. Its high effectiveness is due to a rather rare combination of mechanisms of action on the inflammatory process. It can be used for acute diseases - pneumonia, acute bronchitis, as well as for chronic diseases - chronic bronchitis, COPD, reducing the frequency of exacerbations of the disease and improving the quality of life.
Literature
- Inflammation. Guide for doctors / Ed. V. V. Serova, V. S. Paukova. M.: Medicine, 1995; 468–481.
- Rational pharmacotherapy of respiratory diseases. Guide for practicing physicians / Under the general editorship. A. G. Chuchalina. M.: Litterra, 2004; 104–111.
- Knyazheskaya N.P. The place of acetylcysteine in the complex therapy of acute and chronic respiratory diseases // Handbook of a polyclinic doctor. 2010; 3:26–31.
- Gembitskaya T. E., Kovaleva L. F. Pharmacotherapy for impaired mucociliary clearance in patients with chronic respiratory diseases // Consilium Medicum. 2009; 11 (3): 105–108.
- Novikova L., Baranova O., Ilkovich Yu. Use of acetylcysteine in clinical pulmonology // Doctor. 2014; 2:13–16.
- Simonova O.I. Mucolytics for children: complex questions, important answers // Questions of modern pediatrics. 2014; 13 (1): 26–32.
- Ushkalova E. N-acetylcysteine in the treatment of infections associated with the formation of biofilms // Doctor. 2013; 11:33–36.
- Mechanisms of inflammation of the bronchi and lungs and anti-inflammatory therapy / Ed. G. B. Fedoseeva. St. Petersburg: Nordmed-Izdat, 1998; 187–189.
- Gembitskaya T., Cheremensky A. Acetylcysteine in the treatment of chronic obstructive pulmonary disease // Doctor. 2013; 2:37–40.
- Gembitskaya T. E., Kovaleva L. F. Mucociliary clearance disorders in patients with chronic respiratory diseases // Handbook of a polyclinic doctor. 2009; 10:33–36.
- Boman G., Backer U. Oral acetylcysteine reduces exacerbation rate in chronic bronchitis: report of a trial organized by the Swedish Society for Pulmonary Diseases // European Journal of Respiratory Diseases. 1983; 64(6):405–415.
- Granjean E.M., Berthet P., Ruffmann R., Leuennberger. Efficacy of oral Long-Term N-Acetylcysteine in chronic bronchopulmonary disease: a meta-analysis of published double-blind, placebo-controlled clinical trials // Clinical Therapeutics. 2000; 22 (2): 209–221.
- Stey C. et al. The effect of oral N-Acetylcysteine in chronic bronchitis: a guantitative systematic review // Eur.Respir. J. 2000; 16:253–262.
RU1410253273
S. Ya. Batagov, Doctor of Medical Sciences, Professor
GBOU VPO First St. Petersburg State Medical University named after. ak. I. P. Pavlova Ministry of Health of the Russian Federation, St. Petersburg
Contact Information
Acetylcysteine Canon (100mg, 200mg, 600mg)
Pharmacodynamics
Acetylcysteine is a mucolytic expectorant used to thin mucus in diseases of the respiratory system. Acetylcysteine is a derivative of the natural amino acid cysteine (N-acetyl-L-cysteine). It has a pronounced mucolytic effect and belongs to the class of direct mucolytics.
The action of acetylcysteine is associated with the ability of the free sulfhydryl group to cleave intra- and intermolecular disulfide bonds of sputum glycoprotein aggregates, which leads to depolarization of mucoproteins, having a strong thinning effect and reducing the viscosity of mucus. Acetylcysteine exhibits mucolytic activity against any type of sputum - mucous, mucopurulent, purulent. Acetylcysteine increases the secretion of less viscous sialomucins by goblet cells and reduces the adhesion of bacteria to the epithelial cells of the bronchial mucosa. Stimulates mucous cells of the bronchi, the secretion of which is lysed by fibrin.
Acetylcysteine thins sputum, increases its volume, facilitates sputum separation and significantly softens cough.
In addition to the direct mucolytic effect, acetylcysteine has powerful antioxidant pneumoprotective properties that provide effective protection of the respiratory system from the toxic effects of negative factors: inflammatory metabolites, environmental factors, and tobacco smoke.
Acetylcysteine has a direct antioxidant effect because it includes a free thiol group (-SH), which can interact directly with and neutralize electrophilic oxidative toxins.
Acetylcysteine protects alpha1-antitrypsin (an enzyme that inhibits elastase) from loss of activity that may occur as a result of exposure to HOCL, a powerful oxidative substance produced by the myeloperoxidase enzyme of active phagocytes.
Easily penetrating into the cell, acetylcysteine is deacetylated, releasing L-cysteine, an amino acid necessary for the synthesis of glutathione, which is the most important factor in intracellular protection against exogenous and endogenous oxidative toxins and various cytotoxic substances. This feature of acetylcysteine makes it possible to effectively use the latter in acute poisoning with paracetamol and other toxic substances (aldehydes, phenols, etc.).
The mucolytic properties of acetylcysteine begin to appear within 1 to 2 days from the start of therapy. When taken prophylactically, acetylcysteine reduces the frequency and severity of exacerbations of chronic bronchitis and cystic fibrosis.
Pharmacokinetics
After oral administration, acetylcysteine is quickly and almost completely absorbed from the digestive tract. In the liver it is metabolized to cysteine (a pharmacologically active metabolite) and diacetylcystine, cystine and then to mixed disulfides. The bioavailability of acetylcysteine after oral administration is about 10% due to the pronounced “first pass” effect through the liver. The maximum concentration of the drug (Cmax) after oral administration is reached within 1-3 hours. In the body, acetylcysteine and its metabolites are determined in various forms: partly as a free substance, partly in connection with blood plasma proteins, partly as incorporated amino acids. It is excreted almost completely in the form of inactive metabolites (inorganic sulfates, diacetylcystine) by the kidneys. Only a small amount of acetylcysteine is excreted unchanged through the intestines. The half-life (T½) from blood plasma is approximately 1 hour and depends on the rate of biotransformation in the liver. In case of liver failure, it can increase to 8 hours. Acetylcysteine can cross the placental barrier and accumulate in the amniotic fluid.
Acetylcysteine
A mucolytic agent that thins sputum, increases its volume, and facilitates the separation of sputum. The action is associated with the ability of free sulfhydryl groups of acetylcysteine to break intra- and intermolecular disulfide bonds of acidic mucopolysaccharides of sputum, which leads to depolymerization of mucoproteins and a decrease in sputum viscosity.
In addition, it reduces induced hyperplasia of mucoid cells, enhances the production of surfactants by stimulating type II pneumocytes, and stimulates mucociliary activity, which leads to improved mucociliary clearance.
Remains active against purulent sputum, mucopurulent and mucous sputum.
Increases the secretion of less viscous sialomucins by goblet cells, reduces the adhesion of bacteria on the epithelial cells of the bronchial mucosa.
Stimulates mucous cells of the bronchi, the secretion of which is lysed by fibrin. It has a similar effect on the secretions formed during inflammatory diseases of the ENT organs.
It has an antioxidant effect due to the presence of an SH group that can neutralize electrophilic oxidative toxins.
Acetylcysteine easily penetrates into the cell and is deacetylated to L-cysteine, from which intracellular glutathione is synthesized. Glutathione is a highly reactive tripeptide, a powerful antioxidant, cytoprotector that traps endogenous and exogenous free radicals and toxins. Acetylcysteine prevents exhaustion and helps increase the synthesis of intracellular glutathione, which is involved in the redox processes of cells, thus promoting the detoxification of harmful substances. This explains the effect of acetylcysteine as an antidote for paracetamol poisoning. Paracetamol exerts its cytotoxic effect through the progressive depletion of glutathione. The main role of acetylcysteine is to maintain proper levels of glutathione concentration, thereby providing protection to cells.
Protects alpha1-antitrypsin (elastase inhibitor) from the inactivating effects of the oxidizing agent HOCl produced by myeloperoxidase of active phagocytes. It also has an anti-inflammatory effect (by suppressing the formation of free radicals and reactive oxygen-containing substances responsible for the development of inflammation in the lung tissue).
Acetylcysteine: proven benefits and promising directions
Mucociliary transport is the most important protective mechanism that performs barrier, immune and cleansing functions. Clearing the respiratory tract of foreign particles and microorganisms occurs due to their removal along with tracheobronchial mucus. An increase in mucus viscosity not only disrupts the drainage function of the bronchi, but also reduces the local protection of the respiratory tract [2]. Stagnation of bronchial contents leads to disruption of the ventilation and respiratory function of the lungs, and inevitable infection leads to the development of endobronchial or bronchopulmonary inflammation. In addition, in patients with acute and chronic respiratory diseases, the viscous secretion produced can cause bronchial obstruction [1]. Inflammatory diseases of the respiratory tract are characterized by changes in the rheological properties of sputum, hyperproduction of viscous secretions and a decrease in mucociliary transport (clearance). As a consequence, a cough develops, the physiological role of which is to cleanse the respiratory tract of foreign substances that have entered from the outside (both infectious and non-infectious origin) or formed endogenously [3]. Coughing is a protective mechanism aimed at restoring airway patency. However, cough can perform a protective function only with certain rheological properties of sputum [2]. In this regard, at present, in the treatment of bronchopulmonary diseases, drugs that have a targeted effect on qualitatively and quantitatively changed bronchial secretions (sputum) have become widespread [2]. They are called bronchosecretolytic or mucolytic. Secretomotor drugs known for several centuries (thermopsis, marshmallow, licorice, sodium and potassium iodide, ammonium chloride) have been rarely used in recent years due to their poor tolerability and low effectiveness, especially in the treatment of chronic respiratory diseases, when mucociliary clearance changes significantly. Mucolytics are widely used in the treatment of both acute respiratory tract diseases (tracheitis, bronchitis, pneumonia) and chronic ones (chronic obstructive pulmonary disease (COPD), bronchial asthma (BA), congenital and hereditary bronchopulmonary diseases, including cystic fibrosis) [ 1–4]. Their use is also indicated for diseases of the ENT organs, accompanied by the release of mucous and mucopurulent secretions (rhinitis, sinusitis) [1]. Mucolytic drugs can be divided into 3 groups: – ambroxol drugs; – acetylcysteine preparations; – carbocisteine preparations. The use of proteolytic enzymes as mucolytics is unacceptable due to their possible damage to the pulmonary matrix, as well as the high risk of hemoptysis, allergic reactions and bronchospasm [2]. Active mucolytic drugs are acetylcysteine preparations, for example ACC® [3]. The uniqueness of the acetylcysteine molecule lies in its ability to provide a rapid and pronounced mucolytic effect, achieved through a direct effect on the structure of sputum. The acetylcysteine molecule contains reactive sulfhydryl groups, which break the disulfide bonds of acidic mucopolysaccharides of sputum, and depolymerization of macromolecules occurs, and sputum becomes less viscous and easier to separate when coughing. An increase in the secretion of less viscous sialomucins by goblet cells and a decrease in bacterial adhesion to epithelial cells of the respiratory mucosa are also observed. Stimulation of bronchial mucosal cells leads to increased secretion production, which lyses fibrin. The drug remains active against any type of sputum: mucous, mucopurulent, purulent. This is very important, especially for bacterial infections, when the viscosity of sputum with purulent inclusions must be quickly reduced to allow it to be evacuated from the respiratory tract and prevent the spread of infection. The main indications for the use of acetylcysteine in clinical practice are given in Table 1. Acetylcysteine preparations are prescribed orally in a daily dose for adults and adolescents over 14 years of age of 400–600 mg, divided into 2–3 doses, often in the form of effervescent tablets or granulates for the preparation of a solution. Regarding the variety of dosage forms, you should pay attention to one of the most widely used drugs with this active substance - ACC®. It is available both in dosage forms intended for administration 2–3 times a day (tablets of 100 and 200 mg), and in prolonged-release forms for administration 1 time per day: ACC® Long effervescent tablets 600 mg and ACC® granules for preparing a solution of 600 mg (the latter has no analogues among mucolytic drugs and is intended for drinking hot). The action of acetylcysteine begins within 30–60 minutes and lasts 4 hours [1]. Acetylcysteine, when taken orally, is almost immediately completely absorbed from the gastrointestinal tract. Due to the high “first pass” effect through the liver, the bioavailability of acetylcysteine is very low - about 10%. Metabolized in the liver into a pharmacologically active metabolite - cysteine, as well as diacetylcysteine, cystine and various mixed disulfides. The binding of acetylcysteine to plasma proteins is approximately 50%. The maximum concentration of the active metabolite in the blood is determined after internal use after 1–3 hours and is 2 µmol/l [5]. Acetylcysteine is excreted in the urine almost exclusively in the form of inactive metabolites (inorganic sulfates, diacetylcysteine). Impaired liver function leads to an increase in the concentration of the active metabolite, which can take up to 8 hours, since the rate of excretion of acetylcysteine is mainly determined by hepatic biotransformation. In rare cases, acetylcysteine can have an excessive liquefying effect, which can cause the so-called “flooding” syndrome of the lungs. This effect can develop if the patient has a disturbance in mucociliary transport, a weak cough reflex, or with the irrational use of mucolytic drugs. In young children, this may require the use of suction to remove accumulated secretions [1]. Acetylcysteine should not be prescribed simultaneously with antitussives due to the risk of sputum stagnation due to suppression of the cough reflex. Thus, sometimes the mucolytic effect of acetylcysteine may be undesirable. The simultaneous use of acetylcysteine and nitroglycerin can lead to an increase in the effect of the latter. Since the drug reduces the absorption of penicillins, cephalosporins and tetracyclines, they should be taken no earlier than 2 hours after ingestion of acetylcysteine. When prescribing large doses of acetylcysteine, a decrease in prothrombin time is possible. It is not recommended for use for hemoptysis. A significant advantage of acetylcysteine is its antioxidant effect, due to the presence of an SH group that can neutralize free radicals [4]. Moreover, acetylcysteine exhibits a pronounced antioxidant effect even in low concentrations. Obviously, this happens not only at the biochemical, but also at the biological level [5]. Thus, in 1989, OT Aruoma et al. When studying in vivo and in vitro acetylcysteine, they found its nonspecific activity in neutralizing various free radical groups [5], which is especially important in elderly patients, who are characterized by activation of oxidative processes and a decrease in the antioxidant activity of blood serum. It is well known that inflammatory lung diseases are characterized by a sharp increase in oxidative processes in the lung tissue. Oxidative stress further contributes to damage to the bronchi and lung parenchyma, leads to changes in the local immune response and increases the risk of infection. Acetylcysteine protects cells from the effects of free radicals both by directly reacting with them and by supplying cysteine for the synthesis of glutathione. Some researchers believe that it is the second mechanism of action of the drug that is most important [5]. A decrease in glutathione content is accompanied by impaired surfactant function and increased activity of proinflammatory cytokines. Normally, intracellular glutathione suppresses the production of inflammatory mediators and prevents direct damage to lung tissue under the influence of free radical reactions. There is evidence that the use of acetylcysteine, due to its antioxidant properties, reduces the frequency of exacerbations of COPD [2, 3]. This is relevant for patients with frequent exacerbations (level of evidence B). However, due to the lack of multicenter randomized, placebo-controlled, double-blind studies until recently, almost all modern international and national guidelines for the diagnosis and treatment of COPD do not recommend mucolytic drugs for mandatory treatment (level of evidence D). Nevertheless, ongoing research on the use of acetylcysteine in this area is not without reason, because disorders in the mucociliary link and inflammation are present in bronchopulmonary pathology, and their correction is possible with the help of mucolytics and anti-inflammatory drugs, including antioxidants. By suppressing the formation of free radicals and reactive oxygen-containing substances responsible for the development of inflammation in the lung tissue, this drug also has some anti-inflammatory effects [6–9]. Acetylcysteine protects α1-antitrypsin (elastase inhibitor) from the inactivating effects of HOCl, an oxidizing agent produced by myeloperoxidase of active phagocytes. Thus, its pneumoprotective effect is realized [7, 8]. Due to the increased production of glutathione under the influence of acetylcysteine, its detoxifying effect is realized, i.e. acetylcysteine can be considered a kind of antidote for acute poisoning with aldehydes, paracetamol and phenols [10]. The article by D. Mattin et al. (1990) described the case history of a 32-year-old patient who, 5.5 hours before admission to the intensive care unit, took a potentially lethal dose of one of the arsenic salts for suicidal purposes. Intramuscular administration of dimercaprol and additional detoxification measures were ineffective. The patient's condition worsened. After 27 hours, acetylcysteine was administered intravenously. Over the next 24 hours, the patient's condition improved significantly. A few days later he was discharged in satisfactory condition. One of the reports from the California Center for Disease Control describes a case of recovery of a patient at the age of 42 years after poisoning with toadstool. Acetylcysteine in this case was prescribed orally in high doses. A few days later the patient was discharged in satisfactory condition. No long-term consequences of poisoning were observed. Domestic authors have obtained data on the effective use of acetylcysteine in combination therapy of patients with acute dichloroethane poisoning. Acetylcysteine was used after extracorporeal detoxification (hemosorption) to prevent the development of toxic liver damage [10]. In experimental work using the LLC-PK1 cell line in vitro, the effect of acetylcysteine on the cytotoxicity of cadmium was studied. It has been found that it effectively protects cells from the toxic effects of cadmium, mainly by reducing its penetration into the intracellular space [11]. Acetylcysteine protects cells, in particular oligodendrocytes and fibroblasts, from death due to the influence of various unfavorable factors - programmed cell death (apoptosis), caused by exposure to an inadequate amount of tumor necrosis factor (tumor necrosos factor, TNF). This conclusion was reached by M. Mayer and M. Noble (1994), studying in vitro the properties of acetylcysteine as a cell protector [12]. These data are comparable with the results presented by the team of authors regarding apoptosis of vascular endothelial cells. According to one of the existing pathophysiological models, exposure to peripheral blood mononuclear cells activated by ionizing radiation or bacterial endotoxins (lipopolysaccharides, LPS) blocks the restoration of damaged vascular endothelium and increases apoptosis. This mechanism may underlie various clinical complications involving the internal vascular wall [12]. The results open up prospects for the use of acetylcysteine in pathological processes that have an adverse effect on the inner wall of blood vessels (for example, toxemia of any origin) [13, 14]. Research is underway into the therapeutic effect of acetylcysteine in schizophrenia, bipolar disorder, obsessive-compulsive disorder, AIDS, polycystic ovary syndrome and other conditions [15, 16]. In addition, acetylcysteine, as a donor of sulfhydryl groups, can be used to prevent the development of nitrate tolerance in patients with concomitant coronary heart disease, although these properties of the drug require confirmation in clinical studies [16, 17]. An interesting direction is the study of the positive nephroprotective properties of acetylcysteine during coronary angiography. A small study [18] showed that in the group of patients taking acetylcysteine, the likelihood of an increase in serum creatinine (by more than 25%) within 2 days after contrast administration was 68% lower than in the placebo group. In addition, when taking the drug, mean serum creatinine levels were significantly lower (p = 0.006). According to the authors, the administration of acetylcysteine is an effective and safe method for the prevention of renal dysfunction in patients with nephropathies of various origins who undergo coronary angiography. Clearly, larger studies are needed to demonstrate that acetylcysteine therapy before coronary angiography has a nephroprotective effect and even leads to a reduction in morbidity and mortality due to contrast-induced nephrotoxicity [18]. To summarize all of the above, it should be noted that acetylcysteine compares favorably with other mucolytics, which is associated not only with its main positive properties, reducing viscosity and improving sputum drainage, but also with the presence of a number of additional properties. First of all, this is a product with proven antioxidant and detoxifying activity. Its active study continues, and it is likely that we will soon receive new interesting information about the clinical benefits of acetylcysteine preparations, which will open up new possibilities for its use. Literature 1. Zaitseva O. V. Mucolytic therapy in the complex treatment of respiratory diseases in children // Consilium medicum. Pediatrics. 2002. T. 5. No. 10. P. 17–22. 2. Ovcharenko S.I. Mucolytic (mucoregulatory) drugs in the treatment of chronic obstructive pulmonary disease // Breast Cancer. 2002. T. 10. No. 4. P. 153–157. 3. Sinopalnikov A.I., Klyachkina I.L. The place of mucolytic drugs in the complex therapy of respiratory diseases // Russian medical news. 1997. No. 2 (4). pp. 9–18. 4. Andersen LW, Thiis J., Kharazmi A. The role of N-acetylcysteine administration on the oxidative response of neutrophils during cardiopulmonary bypass // Perfusion. 1995. No. 10 (1). R. 21–26. 5. Aruoma OI, Halliwell V., Noey V.M. The antioxidative action of N-acetylcysteine: its reaction with hydrogen peroxide, hvdroxyl radical, superoxide and hypochlorous acid // Free Radic. Biol. Med. 1989. No. 6 (6). R. 593–597. 6. Klyachkina I.L. Mucolytic therapy in the treatment program for chronic obstructive pulmonary disease // Handbook of a polyclinic doctor. 2006. T. 4. No. 9. 7. Novikov Yu.K., Belevsky A.S. Mucolytics in the complex treatment of COPD // Attending physician. 2001. No. 2. 8. Berdnikova N.G., Tsyganko D.V., Demidova G.V. Features of the use of acetylcysteine in clinical practice // RMJ. 2008. T. 16. No. 2. P. 78–82. 9. Barnes PJ, Adcock IM, Ito K. Histone acetylation and deacetylation: importance in inflammatory lung diseases // Eur.Respir. J. 2005. no. 25(3). R. 552–563. 10. Kurashov O.V., Trotsevich V.A. The use of acetylcysteine in the complex treatment of patients with acute poisoning with 1,2-dichloroethane // Medical Affairs. 1992. No. 10. pp. 109–111. 11. Wispriyono V., Matsuoka M., Igisu N. Protection from cadmium cytotoxicity by N-acetylcysteine in LLC-PK1 cells // J. Pharmacol. Exp. Ther. 1998. No. 287 (1). R. 344–351. 12. Mauer M., Noble M. N-acetyl-L-cysteine is a pluripotent protector against cell death and enhancer of trophic factor-mediated cell survival in vitro // Proc. Nat. Acad. Sci. USA. 1994. No. 91 (16). R. 7496–7500. 13. Lindner N., Holier E., Erd V. Peripheral blood mononuclear cells induce programmed cell death in human endothelial cells and mav prevent repair: role of cytokines // Blood. 1997. No. 89 (6). R. 1931–1938. 14. Ostroumova M.N., Kovalenko I.G., Bershtein L.M. Possibility of using N-acetylcysteine in cancer prevention // Experimental Oncology. 1994. No. 16. pp. 96–101. 15. Sule AA, Tai DY, Tze CC Potentially fatal paracetamol overdose and successful treatment with 3 days of intravenous N–acetylcysteine regime - a case report // Ann Acad Med Singapore. 2006. No. 35 (2). R. 108–111. 16. Zuin R., Palamidese A., Negrin R. High-dose N-acetylcysteine in patients with exacerbations of chronic obstructive pulmonary disease // Clin Drug Investig. 2005. No. 25 (6). R. 401–408. 17. Global Initiative for Chronic Obstructive Lung Diseases (GOLD). Global strategy for diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO workshop report. Last updated 2009. www.goldcopd.org. 18. Shamkhalova M.Sh., Zaitseva N.V., Kurumova K.O. Contrast-induced nephropathy in patients with diabetes mellitus // Difficult patient. 2007. No. 4.
RU1310146160