The main groups of drugs that are used to treat cough:
- Drugs that improve sputum discharge: expectorants,
- mucolytics.
- central action,
The choice of medication should be individual for everyone. Before you start taking the drug, be sure to consult your doctor.
Causes of cough in children
Coughing is a protective reaction to irritation of the mucous membrane of the respiratory tract.
Thanks to coughing, the airways are cleared of secretions that are formed during inflammation of the bronchi, as well as when any irritants enter: allergens, viruses, bacteria. The main causes of cough in children:
- Infectious and inflammatory processes in the upper parts of the respiratory system (ARVI, tonsillitis, laryngitis, sinusitis, pharyngitis).
- Infectious and inflammatory processes in the lower parts of the respiratory system (tracheitis, bronchitis, pneumonia).
- Allergic diseases, bronchial asthma.
- Drying of the mucous membranes due to dry air in the room.
- Entry of a foreign body.
- Drainage of nasal mucus down the back of the throat and towards the larynx. Occurs when lying on your back.
- The release of gastric juice from the esophagus (gastroesophageal reflux).
- Whooping cough.
- Heart failure.
- Neurotic disorder.
Antitussives
Central action
narcotic drugs suppress the cough reflex in the medulla oblongata and depress the respiratory center. They are addictive.
- codeine (Codelac), morphine, ethylmorphine hydrochloride, dextromethorphan (Grippex).
Non-narcotic - have an antitussive and antispasmodic effect, without depressing breathing and without causing addiction.
- butimirate (Intussin, Sinekod), glaucine (Broncholitin, Glauvent), oxeladine (Tusuprex, Paxeladin).
Peripheral action
They act as mild analgesics on the receptors of the respiratory mucosa and reduce the cough reflex. One of the most important effects of medications in this group is hydration of the mucous membranes. They are used in the form of aerosols and steam inhalations to reduce the viscosity of secretions and against irritation of the mucous membrane.
Local anesthetics are used mainly in hospitals to stop the cough reflex during bronchoscopy.
- benzocaine, tetracaine, lidocaine, prenoxdiazine (Libexin).
Enveloping preparations of plant origin are used for irritation of the mucous membrane of the upper respiratory tract. They create a protective layer for the mucous membrane of the nasopharynx and oropharynx, which reduces the cough reflex.
- extracts of eucalyptus, acacia, wild cherry, various infusions, syrups, teas, lozenges, lozenges, honey.
Inhalation of water vapor with the addition of various components (sodium chloride, sodium bicarbonate, ammonium chloride, plant extracts) is the most common way to moisturize the mucous membranes.
Dry cough in a child
A dry cough usually occurs against the background of a respiratory disease and is localized in the upper part of the respiratory tract. With this type of cough, no sputum is produced.
At the beginning of an acute respiratory infection (ARI), the cough is dry, debilitating, and the general condition of the body worsens. At this stage, complete cleansing of the respiratory tract does not occur, but after a few days, sputum gradually begins to be released from the bronchi.
However, this does not always happen. In some cases, a dry cough can last up to 3 weeks or more. The likely cause of this cough is inflammation . A reflex urge to cough leads to an intensification and spread of the inflammatory process of the throat or larynx.
A prolonged dry cough that lasts for weeks without any fever or weakness is most often a sign of an allergic reaction to animal hair, dust, or tobacco smoke.
Heated discussions continue among pediatricians regarding treatment tactics for the most common and prominent symptom in children with acute respiratory infection (ARI) – cough. And if the theoretical aspects of this phenomenon are well studied, many pathogenetic mechanisms are clear and thoroughly studied, then there are sometimes fundamental disagreements regarding the rational treatment of cough in children against the background of viral respiratory infections [1, 2]. Despite the fact that in Cochrane reviews, from the perspective of evidence-based medicine, we are provided with the results of scientific works that are recommended for use by the doctor, in practice, the choice of a treatment regimen each time causes great difficulties and controversy, especially for the pediatrician. This is quite understandable, because... Each doctor has extensive personal practical experience of successful and controversial clinical cases, his own observations and the opinions of colleagues. The list of medications that exists today is huge, which often leads to polypharmacy and unreasonable prescription of drugs. However, we must make a decision in accordance with approved treatment standards and federal clinical guidelines.
The relevance of the problem remains to this day. Respiratory diseases in children still lead in frequency, reaching 50–73% in the structure of childhood morbidity. Thus, according to the chief freelance pulmonologist of Moscow, Professor A.B. Malakhov, the overall incidence of respiratory diseases among children in recent years remains at a high level and has no tendency to decrease. There are 50 thousand cases of ARI per 100 thousand children (Table 1) [3–6].
The most common manifestation of a respiratory disease is a cough. This type of complaint is most often addressed to a pediatrician. Should he be “treated” against the background of ARI? How often are antitussive drugs used in pediatrics? Drugs that eliminate the cough reflex include the so-called. narcotic antitussives based on codeine and its derivatives and a group of non-narcotic antitussives. The active ingredients for centrally acting agents are oxeladin citrate, pentoxyverine, dextromethophan, butamirate citrate, glaucine hydrochloride. Active substances of peripheral action include prenoxadiazine hydrochloride. The use of such drugs in children may be unsafe. In case of ARI, which is accompanied by the presence of viscous sputum and a wet cough, it is absolutely unacceptable to suppress the cough center and block the cough as the main protective mechanism for clearing the airways. These drugs can cause undesirable effects in children such as increased drowsiness, respiratory depression, constipation, and many others. etc. Therefore, in this clinical situation they are contraindicated.
In pediatrics, there are quite strict indications for the use of antitussive drugs. This is a cough caused by an identified cause of infection: either whooping cough or measles tracheitis. A pediatrician can use an antitussive drug once if a paroxysmal painful cough significantly disrupts sleep and eating, causes vomiting, and the child’s well-being suffers catastrophically. There are also surgical causes of cough, where immediate suppression is really required, for example in thoracic surgery or in acute pneumothorax. For children with severe forms of pathology of the central nervous system, if there is a high risk of aspiration, it is also possible to periodically prescribe drugs that suppress the cough reflex [7].
The simultaneous prescription of mucolytic and antitussive drugs remains a rather serious and frequent medical error. This is where one of the myths about “swamping the lungs” arises. It is impossible, on the one hand, to liquefy sputum, and on the other hand, to simultaneously block the mechanism of its evacuation [8]. Practice shows that expectorants are often used for coughs due to acute respiratory infections and are not only prescribed by pediatricians, but are also actively purchased at the pharmacy by parents. Expectorants, or so-called. secretomotor, drugs should enhance coughing. They differ not only in their mechanism of action, but also in the composition of the active substance. Preparations of plant origin (marshmallow, istoda, thermopsis and other medicinal herbs), terpinhydrate and lycorine, as well as essential oils have a weak thinning effect and stimulate the formation of mucus in the bronchi.
Unfortunately, they also affect the salivary glands, which is an undesirable effect. Preparations based on various salts, such as sodium iodide, potassium iodide and ammonium chloride, can stimulate bronchial secretion and slightly dilute sputum. However, the pediatrician must take into account that this group of drugs has side effects that are significant for the child, for example, the ability to increase the gag reflex, cause various allergic reactions, moreover, these drugs significantly increase the volume of sputum. Many herbal products have a multicomponent composition, and it is impossible to predict how all these components will interact [9]. In addition, the period of action of these drugs is quite short (usually 2–3 hours), there is a need for repeated administration, which in general can lead to an overdose and certain complications [10].
The effectiveness of over-the-counter medications for ARI in children and adults was shown in a 2014 Cochrane review. 29 studies were analyzed: 19 (3799 patients) in adults and 10 (1036 patients) in children [11]. It has been shown that no evidence-based studies have been conducted for expectorants. Antitussives that suppress cough have not been shown to be superior to placebo. And only the group of mucolytic drugs was proven effective compared to placebo.
A 2013 Cochrane Collaboration review of mucolytics (acetylcysteine and carbocysteine) for ARI in children under 13 years of age demonstrated their safety based on 34 (2064 patients) studies using clinical, biological, radiographic and respiratory function parameters . Efficacy was assessed in 6 placebo-controlled studies (497 patients). It has been clearly established that the drugs are effective and have a high safety profile for children over two years of age. It should be noted that in clinical studies there were not a single case of the so-called. swamping of the lungs syndrome and not a single case of bronchospasm, which is sometimes feared by practicing pediatricians [12].
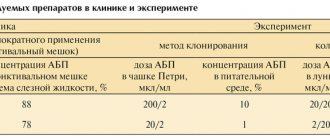
Modern mucolytics are created on the basis of various chemical formulas, which explains their different mechanisms of action (Table 2). Looking at the information in the table, you can decide which mucolytic is advisable to use in a specific clinical situation and choose not by name, but by the mechanism of action of the active substance.
Acetylcysteine and ambroxol are included in the list of vital and important medications, and dornase alfa according to the “7 nosologies” program is included in the basic therapy of cystic fibrosis. In order to assess the effectiveness, tolerability and safety of mucolytics for children with ARI, a study was conducted on 259 children with acute and chronic bronchopulmonary pathology under the age of 15 years. Children received treatment for 5–15 days: 92 children received acetylcysteine, 117 - ambroxol, 30 - bromhexine and 20 - mucaltin. The authors showed that the best clinical effect in children with acute bronchitis was obtained with the use of acetylcysteine. When prescribing bromhexine and ambroxol, a pronounced mucolytic effect was also noted, but at a later date from the start of treatment.
In the attacking period of bronchial asthma, when acetylcysteine was prescribed in complex therapy, the best effect was achieved by children of the younger age group [7, 13]. In addition to the mucolytic effect, the acetylcysteine molecule has two additional effects. Thanks to its triple effect - mucolytic, antioxidant and anti-inflammatory - the use of acetylcysteine in ARI helps reduce the duration of cough, reduce the intensity of the inflammatory reaction and shorten the duration of the disease. The mucolytic effect of acetylcysteine is due to the presence of an SH group in the acetylcysteine molecule, which breaks the disulfide bonds of acidic mucopolysaccharides of sputum, directly changes the rheological properties of sputum, reduces its viscosity and adhesiveness. The direct antioxidant effect of the acetylcysteine molecule is explained by the fact that reactive SH groups bind to free radicals and thus neutralize them. And the indirect antioxidant effect occurs due to the ability of acetylcysteine to influence the synthesis of glutathione. The anti-inflammatory effect is associated with the ability of this molecule to increase cell protection from the damaging effects of free radical oxidation inherent in the inflammatory response. The practical significance of this triple action for patients is shown in a research work in which 60 children aged 2 to 10 years were observed with clinical manifestations of acute respiratory disease and with difficult to separate sputum (acute bronchitis, including with obstructive syndrome, acute stenosing laryngotracheitis, pneumonia).
As a result of observation, it was shown that the use of acetylcysteine in the complex treatment of acute respiratory diseases in children contributes not only to a more rapid achievement of a productive cough with improved bronchial drainage function and a reduction in the duration of cough, but also to a more rapid relief of symptoms of intoxication and fever, which contributed to a reduction in hospitalization time children with acute respiratory diseases [14].
The safety and good tolerability of the drug can be judged by how it is tolerated in chronic conditions, for example, chronic bronchitis, when therapy is carried out in long courses. A 2015 Cochrane review found that studies involving 9367 patients showed a reduction in exacerbations when mucolytics were used for more than 10 months. All mucolytics used (including acetylcysteine, carbocysteine, ambroxol and bromhexine) turned out to be safe, and all were well tolerated [15]. However, this review included studies from adults. In children, long-term use of mucolytics for 12 months was shown in 4 studies involving 149 children over two years of age with cystic fibrosis. The results obtained did not reveal significant clinical differences between acetylcysteine and ambroxol; there were no serious side effects with both inhalation and oral administration; the drugs were well tolerated [16, 17].
An important practical question for a pediatrician: how do mucolytics work for upper respiratory tract infections? In the indications for the use of acetylcysteine and carbocysteine, unlike other mucolytics, their use is also prescribed for upper respiratory tract infections, such as catarrhal and purulent otitis media, acute and chronic sinusitis. This is understandable, since the mucous membrane of the respiratory tract begins with the nasal cavity and ends deep in the bronchioles. Therefore, the laws of inflammation during infection, the pathogenesis of the development of acute bronchitis and acute rhinitis are similar throughout the respiratory tract. The acetylcysteine molecule will exhibit its mucolytic and anti-inflammatory properties equally in the lower respiratory tract and in the upper. Otorhinolaryngologists widely use acetylcysteine in their practice [18–20].
During an acute infection, inflammation occurs on the mucous membrane of the respiratory tract and a viscous secretion is formed, which leads to blocking of mucociliary transport, mucostasis develops and, as a result, microbial colonization. ARIs are usually caused by viruses, but bacterial complications may require antibiotic therapy. The review showed that all mucolytics, if necessary, combine well with antibiotics (Table 3) [21, 22].
In some studies, it was shown in relation to the acetylcysteine molecule that it increases the clinical effectiveness of antibacterial therapy by suppressing the growth and destruction of bacterial biofilms [23, 24]. A comparative study was carried out on the effectiveness of mucoactive drugs in reducing the viability of biofilms produced by S. aureus strains [25]. It was found that the activity of acetylcysteine was 5.5 times higher than that of ambroxol and bromhexine.
The combination of acetylcysteine with penicillin antibiotics for acute bronchitis and pneumonia helps to reduce the intensity of cough already by the third day from the start of treatment, and with cephalosporins (for example, cefuroxime) increases effectiveness for bacterial infections of the respiratory tract [26–29].
Each time, the pediatrician must choose not only the drug itself, but also the most effective route of administration. Today, acetylcysteine and ambroxol have dosage forms in the form of solutions for nebulizer therapy, unlike carbocysteine. This is definitely an innovative technology. But the nebulizer method of administration also has its drawbacks. First of all, the presence in the family of a sick child of the device itself - modern and of good quality. The psychological characteristics of the child do not always allow the inhalation procedure to be carried out. It takes a lot of time and requires complete physical and emotional commitment. There is no systemic effect with this route of drug administration. This can be considered a positive fact [30]. But, in the case when it is necessary to influence not only the lower respiratory tract, but also the upper, to relieve the symptoms of intoxication, you will need to take a mucolytic orally. Nebulizer therapy is deservedly widely used both in hospitals and in outpatient practice. But in most cases there is no need for inhalation delivery, because The bioavailability of drugs when taken orally is sufficient. It is necessary to rationally balance decision-making depending on the specific clinical situation of the patient.
In normal practice, it is not advisable to prescribe multiple mucolytics at the same time. There is no need to enhance the mucolytic effect with drugs from one drug group. Moreover, this can be considered a medical error, because in a child with ARI, excessive sputum production can be caused, which the baby will not be able to effectively evacuate, and complications may arise in the form of “swamping of the lungs syndrome,” obstruction with respiratory failure, and even pneumonia. When treating patients with chronic bronchitis, for example, against the background of cystic fibrosis or severe congenital malformations of the bronchi with severe mucostasis, this practice, on the contrary, is successfully used. Using different properties of active molecules, it is possible to create the most effective combinations of mucolytics, as well as use different routes of their administration (for example, alternating inhalation with oral administration) [31].
It should be noted that acetylcysteine is recommended by the Standards of Primary Health Care for ARI and Sinusitis; acetylcysteine and ambroxol are included in the standards of outpatient care for acute bronchitis. These regulatory documents enable the practitioner to use these medications reasonably [32].
Thus, the main practical conclusions and recommendations for selecting therapy for ARI for children include the following:
- for uncomplicated ARI in children, acetylcysteine and ambroxol, which have the same proven effectiveness and have a high level of safety, can be equally used for mucolytic purposes. It should be borne in mind that acetylcysteine will act somewhat faster, because is a direct mucolytic, but not “stronger”;
- in case of acute infection, which occurs with symptoms of bronchitis and rhinosinusitis, it is advisable to use acetylcysteine, which will dilute not only bronchial, but also nasal secretions, and also reduce inflammation in the paranasal sinuses. For children over two years of age, ACC® (acetylcysteine 20 mg/ml) can be recommended in a child-friendly form - syrup without sugar, alcohol and dyes;
- if ARI occurs in addition to cough with severe symptoms of intoxication (high fever, severe weakness), you should choose acetylcysteine, not only due to its mucolytic, but also antioxidant and anti-inflammatory properties, which will neutralize these symptoms;
- in case of prolonged or chronic inflammation in the respiratory tract, it is advisable to use ambroxol, using its property to stimulate the synthesis of surfactant, which decreases with prolonged bronchitis;
- if there are indications for prescribing antibiotics, a combination with acetylcysteine is preferable, which has the property of destroying bacterial biofilms and thus can enhance the effect of the antibiotic;
- for children under two years of age, ambroxol remains the drug of choice (any dosage forms, including solutions for inhalation, but you must remember about drainage);
- it is possible to combine the ways of administering mucolytics depending on the situation: ½ of the daily dose should be prescribed in the form of nebulizer inhalation, and ½ as a daily dose orally.
Wet cough in a child
Cough with sputum is characteristic of a number of serious diseases: from acute respiratory viral infections to pneumonia and tuberculosis. Foreign particles, toxins, and bacteria are removed from the respiratory tract with sputum. It is important to pay attention to the color and consistency of the mucus coming out:
- white thick is characteristic of ARVI;
- clear mucus is characteristic of bronchial asthma, allergic reactions, heart diseases;
- yellow mucus occurs during purulent processes;
- a rusty color indicates damage to small capillaries in the lungs, which is typical for pneumonia;
- a greenish tint indicates pneumonia, purulent bronchitis;
- brown color is characteristic of tuberculosis and lung tumors.
Of course, it is impossible to make a diagnosis based solely on the type of sputum. Competent consultation with a specialist (pediatrician, pulmonologist, otolaryngologist) and tests are always necessary.
ACC
The mucalytic effect that this drug has on the body allows ACC to be proven as an active medicine. In addition, ACC has an anti-inflammatory effect, reducing chest and throat pain.
The drug has contraindications: it is not recommended for use by pregnant women and nursing mothers. Experts also note that the drug should not be combined with other antitussives and paracetamol. Otherwise, you will also have to deal with congestion of the respiratory tract.
Pros:
- Quickly removes mucus and relieves cough
- Does not irritate mucous membranes
- Delicious
- Versatility (suitable for many diseases)
- Convenient packaging
Minuses:
- There are many contraindications, it is better to consult a doctor
- Possible exacerbation of allergies
Cough and fever
An increase in temperature when coughing indicates a reaction of the immune system to the occurrence of an inflammatory process in the body.
Dry cough with fever
The most common causes of a dry cough with an elevated temperature in the range of 37–37.5 0C are infectious and inflammatory diseases in the initial stage.
- Flu, ARVI . In the first days of the disease, the cough is irritating, painful, and dry.
- Laryngitis . With the development of inflammation of the larynx, the cough is convulsive, barking, and there is a feeling of obstruction in the throat when swallowing.
- Pharyngitis . Noticeable redness of the back of the throat with persistent cough and rapid rise in temperature.
- Dry pleurisy . Chest pain worsens with sharp inspiration or coughing.
- Pneumonia of atypical form . Inflammation of the lungs is accompanied by a dry cough, chills, the condition worsens sharply, and shortness of breath may occur.
- Whooping cough . Most often children of the first year of life and school age become ill. A paroxysmal cough at the beginning is unproductive; as the disease progresses, the attacks intensify and end with vomiting or spitting out thick, viscous sputum, followed by a characteristic wheezing inhalation.
- Bronchial asthma . Choking and loud wheezing may occur. Clearing the throat, inhaling and especially exhaling is difficult.
- Worm infestation . The appearance of a cough is associated with the entry of helminth larvae into the lungs. Breathing becomes whistling and audible at a distance.
Wet cough with fever
Typically, a cough becomes productive in the later stages of the same acute respiratory infections: viral and bacterial. It is often accompanied by fever - a high temperature of up to 38 0C. Cases requiring special attention:
- Bronchitis . May develop as a complication of acute respiratory infections. High temperature and cough with sputum indicate an active inflammatory process in the bronchi.
- Pneumonia is typical . A wet cough appears due to the proliferation of microorganisms, which provoke copious mucus secretion in the bronchi.
- Lung abscess . It is characterized by the formation of a hollow area in the lung tissue that is filled with pus. When the cavity ruptures, purulent sputum comes out, it has an unpleasant odor, and may contain blood impurities.
- Tuberculosis . The temperature is kept up to 38 and rarely up to 39 degrees. The cough is severe and blood may be released. The sputum of a patient with tuberculosis contains mycobacteria and is infectious to others.
Cough without fever
The most common causes of cough at normal temperature in a child are:
- The onset of viral and bacterial infections while the immune response has not yet developed and the temperature has not risen.
- Allergic reaction to plant pollen, dust, mold, animal hair, etc.
- A reflex reaction to dust, smoke, and aerosols entering the bronchial mucosa.
- Entry of a foreign body into the respiratory tract.
- Diseases of the nasopharynx, impaired flow of mucus from the nose.
- After illnesses as a residual phenomenon.
How to deal with dry and wet cough?
When treating cough, an integrated approach
to therapy. Therefore, it is important to follow the following recommendations.
- Take cough medicine as prescribed by your doctor. Depending on the type of cough, the age of the patient and other factors, drugs with different effects and different forms of release may be prescribed (children's antitussive syrups, herbal lozenges, etc.).
- One of these products is Doctor MOM® syrup. The “FITO BRONHO 10 formula”1 included in its composition facilitates the removal of mucus, preventing its stagnation, and also fights inflammation - the cause of cough.
- Control the humidity level in the room. Sufficient humidity (not lower than 60%) will prevent drying out of the mucous membranes of the nose and throat, which will ease coughing attacks.
- Do chest massage. It stimulates mucus secretion and relieves cough.
Cough medicines for children
How to treat cough in children
First of all, treatment is carried out to combat the causative agent of the disease and to alleviate the general condition of the child.
- If the cough is caused by a bacterial infection, then antibacterial drugs are prescribed.
- For a viral cause of the disease, antiviral drugs are prescribed, for a fungal infection of the lungs, antifungal drugs are prescribed.
- The allergic form of the disease requires the use of antihistamines.
- If sputum is poorly separated from the bronchi, then the prescription of mucolytic drugs is required.
- If your body temperature is elevated (above 38 degrees), you need to take antipyretics.
Cough preparations by group
What cough remedies should not be used by children?
In childhood, the cough reflex is not complete; it is formed by 5-6 years. It is important for both pediatricians and parents to remember that the use of drugs that suppress the cough reflex is contraindicated, especially in young children. It is also necessary to limit the use of expectorants, as they increase the volume of mucus secreted, which can lead to stagnation and further reinfection.
What can you give children for cough?
Mucolytics are the most promising for the treatment of diseases of the upper and lower respiratory tract. They are used for non-productive or productive cough with sputum that is difficult to separate. Today, the following mucoactive drugs are widely used in pediatric practice: bromhexine, ambroxol and acetylcysteine (ACC).
The main methods of using medicines in children are oral and inhalation. Depending on the disease, age and preference of the child, the choice of form is considered individually.
Antitussives for various types of cough
It is a mistake to believe that only a dry, non-productive cough needs treatment. It should be understood that without proper therapy, including without taking a properly selected cough remedy, an unproductive wet cough can quickly transform into an unproductive one. Therefore, with an unproductive wet cough, the doctor may recommend means that facilitate the separation of sputum in order to prevent it from becoming unproductive and to improve the removal of infected mucus from the body. And for dry conditions, drugs that stimulate the secretion of mucus, its dilution and/or removal from the bronchi, in order to prevent the development of congestion in the respiratory organs and the complications caused by this.
Bromhexine for children
The drug bromhexine is actively used in pediatric practice and has various release forms suitable for children: syrup, mixture (solution), low-dose tablets (4 mg).
The effect of bromhexine is based on the drug’s ability to thin mucus and facilitate its removal from the child’s respiratory tract.
Cough syrup for children
syrup is very easy to use, has a fruity taste and children drink it with pleasure. The syrup is prescribed to children from two years of age. This is due to the fact that children under one year old cannot cough on their own and they may experience stagnation of sputum in the bronchi. The accumulation of sputum can lead to a deterioration in the child’s condition and a protracted course of the disease.
Can children take cough drops?
The administration of tablets with a pediatric dosage of 4 mg is permitted from 3 years of age. Bromhexine is also available in a drinking solution and drops, which contain medicinal plant oils. These forms are used only for children over 12 years of age, since the composition contains ethanol.
During treatment with bromhexine, the child should be given enough fluids. To improve the removal of mucus from the bronchi, it is useful to massage the chest, especially for young children. And be sure to consult a doctor before using the drug.
Expectorants
This group of drugs stimulates the secretion of bronchial glands and the movement of the epithelium, increases the volume of sputum and slightly reduces its viscosity.
Direct action
Resorptive (direct) action drugs directly affect bronchial secretion. They are used in the form of tablets, solutions and mixtures.
- potassium iodide, sodium iodide, sodium bicarbonate, ammonium chloride.
Reflex action
Reflex (indirect) action drugs irritate the stomach receptors, causing a reflex increase in gland secretion and stimulating muscle contraction when coughing. Used in the form of infusions, powder, tablets, dry extract, collections, etc.
- thermopsis herb (Codesan), terpinhydrate (Coldrex), licorice root (Doctor MOM), marshmallow (Mukaltin), guaifenesin (Tussin), ammonia-anise drops and others.
Herbal remedies
Essential oils of medicinal plants have expectorant, anti-inflammatory and weak antiseptic effects.
- thyme herb (Bronchicum), eucalyptus leaf (Pectussin), ivy leaves (Gedelix), licorice (Glyceram), oregano, coltsfoot, elecampane and other plants in various combinations.
A prerequisite for the development of the therapeutic effect of any expectorant medications is regular drinking of water to prevent dehydration.
Side effects and contraindications
The use of some drugs is limited in pediatrics, pregnancy and lactation, carbohydrate metabolism disorders, as well as in the acute period of certain diseases. A complete list of contraindications and restrictions is indicated in the instructions for the drug.
- Stomach. When taken orally, they irritate the gastrointestinal mucosa and increase the secretion of gastric juice, therefore they are not used for gastritis and peptic ulcers.
- Allergy. Plant extracts often cause allergic reactions and are contraindicated in bronchial asthma.
- Vomit. Reflex-action drugs strengthen not only the cough reflex, but also the gag reflex. Large doses cause nausea and vomiting. Young children, as well as those with central nervous system damage, should not use them, as respiratory arrest may occur.
- For children. Medicines from these groups significantly increase the volume of secretions. But small children are not able to fully expectorate sputum themselves. This can lead to congestion in the bronchi and re-spread of infection.
Doctor Mom
Doctor Mom is a whole line of drugs in lozenges, ointments and syrups. Causes expectoration, removes phlegm, reduces inflammation and relieves pain when coughing. The composition includes many beneficial herbs (aloe, basil, ginger, etc.). Designed for both adults and small children.
Pros:
- Pleasant to the taste
- Relieves cough
- Affordable prices
- Used for prevention
- Suitable for long-term use
Minuses:
- Manifestation of an allergic reaction
- Not effective for severe cough