Why does myocardial infarction develop?
Our heart is a tireless worker. In one minute it pumps more than five liters of blood and makes about one hundred thousand beats. The heart performs the most important functions for the human body:
- due to rhythmic contractions, it ensures blood flow through the blood vessels;
- saturates organs and tissues with oxygen;
- removes carbon dioxide and other harmful substances from the body.
With the development of myocardial infarction, the heart loses its ability to function normally, which often leads to disability and death.
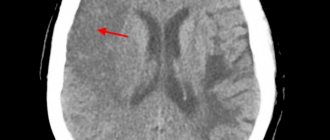
The main cause of myocardial infarction is atherosclerosis, a chronic vascular pathology caused by impaired lipid and protein metabolism. During the disease, atherosclerotic plaques form in the lumen of blood vessels - dense formations of cholesterol, covered with fibrous tissue on top.
With certain changes in the body (stress, increased blood pressure), vascular spasm occurs, which often leads to rupture of an atherosclerotic plaque with the formation of blood clots. If this occurs in the heart muscle, then acute myocardial infarction develops. If in the intestines, then intestinal infarction, etc.
People with chronic diseases have an increased likelihood of developing myocardial infarction:
- diabetes mellitus;
- hypertension;
- coronary heart disease;
- varicose veins of the lower extremities.
What could cause it to appear?
The main cause of the pathology is damage to the inner lining of the coronary artery. This is a vessel that nourishes the tissues of the heart. As long as its diameter does not narrow and the walls remain elastic, no negative changes occur. Reducing the lumen limits blood flow. A similar picture emerges when:
- atherosclerosis;
- spasm of the coronary arteries;
- increased blood viscosity;
- formation of blood clots - thrombi.
The disease can be triggered by the influence of negative factors, which include:
- hormonal disorders;
- long-term treatment with corticosteroids;
- hypertonic disease;
- obesity;
- smoking;
- alcohol consumption;
- sedentary lifestyle;
- emotional overload.
In rare cases, myocardial infarction can be triggered by other internal pathologies: rheumatism, cancer, severe allergic reactions.
Clinical options for the development of myocardial infarction
The classic form of myocardial infarction is accompanied by a severe pain syndrome of a compressive, tearing, burning nature. The pain is most often localized behind the sternum, but can also radiate to the left arm, left shoulder, lower jaw, and interscapular area. As a rule, the pain lasts more than 20 minutes and is not relieved by nitroglycerin within 5 minutes.
Other symptoms of classic myocardial infarction:
- increased sweating;
- psychomotor agitation;
- feeling of fear of death.
There are also atypical options for the development of myocardial infarction:
- abdominal form. In this case, the patient experiences heartburn, nausea, vomiting, pain in the upper abdomen;
- arrhythmic form. Characteristic signs are heart rhythm disturbances, a feeling of interruptions in the heart;
- asthmatic form. The main symptoms are shortness of breath, suffocation;
- painless form. It is characterized by the absence of pain or the presence of mild pain that occurs at varying frequencies. This form especially often develops in patients with diabetes mellitus and in people who have already suffered a myocardial infarction in the past.
Why is the painless form dangerous? First of all, the development of sudden cardiac death. In addition, if in the acute period a myocardial infarction occurs without clear clinical symptoms, then in the future this can lead to the development of chronic heart failure.
The painless form of myocardial infarction can be recognized by other signs. For example, a person may experience shortness of breath, increased fatigue, and exercise intolerance.
Pre-hospital emergency room
The standard for the arrival of an EMT team in the city is 10 minutes, outside the city limits - 20 minutes after registering a call with the dispatch service. If we take into account weather conditions, the epidemiological situation and the traffic situation, it is possible that the time may be exceeded (no longer than 10 minutes).
According to the protocol, the algorithm of the team’s actions upon arrival to the patient includes:
- Anamnesis collection (if possible).
- If necessary, perform resuscitation measures (ventilation, chest compressions, defibrillation).
- Conducting an examination and physical examination to assess the condition of the cardiovascular and respiratory systems.
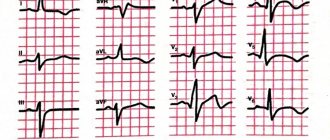
- Registration of 12 leads ECG with repeat after 20 minutes.
Pulse oximetry (if saturation is below 95% - oxygen support by mask or through nasal cannulas 3-5 l/min.).- Determine the level of troponins I, T in the blood (if a portable test is available).
- Providing venous access.
- Actually emergency medical care:
- Nitroglycerin 0.5-1 mg every 10 minutes. In case of severe pain, intravenous drip administration under the control of SBP (not lower than 90 mm Hg);
- relief of an anginal attack with narcotic analgesics. Preferably, Morphine 2-5 mg every 10-15 minutes until the pain stops (total dose not exceeding 20 mg);
- "ASA" 150-325 mg chewed, if the patient did not take it before the ambulance arrived;
- conducting dual antiplatelet therapy - Ticagrelor 180 mg, in its absence, Clopidogrel is prescribed at a dose of 300 mg;
- short-acting beta blockers - Propranolol, Metoprolol;
- reduce the load on the myocardium by lowering blood pressure and correcting hemodynamic disturbances.
If possible, it is recommended to carry out thrombolysis therapy TLT (streptokinase, alteplase, actilyse) at the prehospital stage. If thrombolysis can be carried out within 2 hours from the onset of ischemic changes (optimally within 60 minutes), this can interrupt the development of necrosis during MI, reduce the affected area and significantly reduce mortality. TLT is not effective if more than 12 hours have passed since the onset of the painful attack. Also, the procedure is not performed in the presence of absolute contraindications: intracranial bleeding or hemorrhagic stroke over the past 3 months, malignant brain tumor, abdominal aortic aneurysm with a tendency to dissection, bleeding from the gastrointestinal tract during the last month, disorders of the hemostatic system.
All patients with ACS are hospitalized in the intensive care unit of a specialized cardiology hospital with the ability to perform emergency angiography and reperfusion interventions.
First aid for myocardial infarction
In providing first aid, the principle of the “golden hour” is very important, from the moment the symptoms of the disease appear until the patient is admitted to the hospital. In critical situations, even more rapid action is required. The severity of the condition during a heart attack depends on how much the lumen of the vessel is blocked by a thrombus. If occlusion (complete obstruction) of a vessel occurs, a critical condition develops. The patient has 20–40 minutes left, after which necrosis of the cardiac tissue occurs.
It is very important not to wait for the pain to subside or for the work day to end. If symptoms characteristic of a heart attack appear, you should immediately take the necessary medications and call an ambulance.
Before doctors arrive, a person with coronary syndrome should be provided with first aid.
Correct algorithm of actions:
- Place the person in a semi-sitting position. For example, you can put the patient in bed and place pillows under his back. A semi-sitting position reduces the load on the heart.
- Provide the patient with complete physical and mental rest, try to calm him down. Physical and emotional stress increases myocardial ischemia and increases the need for oxygen in the heart muscle.
- Free your body from constrictive elements of clothing - remove your tie, belt, unbutton your shirt collar.
- Create an influx of fresh air - open a window or vent.
- Give the patient half a tablet of aspirin to chew. This will reduce the area of the heart attack and reduce the risk of death.
- If possible, you need to measure the person's blood pressure.
- If you have high blood pressure, be sure to give a drug for hypertension, as well as nitroglycerin. Nitroglycerin capsules are placed under the tongue and sprayed under the root of the tongue as a spray.
Complications
Complications of myocardial infarction are early and late. As a rule, early complications develop in the first hours of a heart attack during hospitalization or for several days after the attack. The occurrence of complications is significantly influenced by the timeliness of first aid and hospitalization.
The most common early complications include:
- disturbances in the rhythm and conduction of the heart, which in most cases are fatal;
- rupture of the heart muscle;
- development of acute left ventricular failure, which is accompanied by pulmonary edema.
The last stage of left ventricular failure is cardiogenic shock, in which myocardial contractility sharply decreases and the blood supply to all organs is disrupted. The condition is accompanied by a strong drop in blood pressure, a decrease in body temperature, pale skin, difficulty breathing, oliguria, and loss of consciousness. The probability of death with cardiogenic shock is 90%.
Late complications of myocardial infarction:
- early post-infarction angina. A person who has such a complication does not tolerate even the slightest physical activity. Any activity causes squeezing pain behind the sternum. Even simple self-care activities lead to pain. The pain is less severe than during a heart attack itself, but quite painful;
- chronic heart failure, which is accompanied by shortness of breath, edema of the lower extremities, enlarged liver, and the development of chronic left ventricular aneurysm.
What it is
Myocardial infarction, or heart attack, most often occurs in older patients. The risk group includes women over 55 years of age and men over 45 years of age.
Doctors classify pathology according to the time of its occurrence:
- primary infarction – occurring for the first time;
- recurrent infarction – diagnosed within 1.5 months after the first attack;
- repeated heart attack – occurring after 6 weeks from the date of the first incident.
Several departments can be affected at once. In this case, we are talking about an extensive heart attack. Pathology can only affect the left ventricle - its septum or walls. The tissue of the right ventricle dies less often.
Rehabilitation
a cardiologist twice a month . During the second year after the attack, it is necessary to visit a general practitioner once every four months. If necessary, each of these specialists can refer the patient to a rehabilitation center or sanatorium.
For successful rehabilitation, it is important for the patient to strictly follow all the doctors’ recommendations:
- take necessary medications. These may be statins, anticoagulants, antihypertensive drugs;
- maintain a balance between sleep, work and rest;
- walk in the fresh air more often;
- avoid stress. After a heart attack, a person should receive only positive emotions.