Myocardial infarction
Diabetes
Atherosclerosis
9437 16 February
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Myocardial infarction: causes, symptoms, diagnosis and treatment methods.
Definition
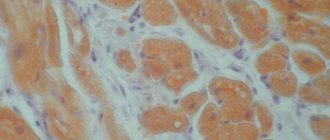
Myocardial infarction (MI) is the necrosis of an area of the heart muscle due to insufficient blood supply with the development of a characteristic clinical picture.
Causes of myocardial infarction
The heart is a hollow muscular organ shaped like a cone. The walls of the heart consist of three layers. The inner layer - the endocardium - lines the cavities of the heart from the inside, and its outgrowths form the heart valves. The middle layer, the myocardium, consists of cardiac muscle tissue. The outer layer is the pericardium. The human heart has four chambers: two atria and two ventricles. The right atrium receives blood from the tissues of the heart itself and all parts of the body (through the superior and inferior vena cava). Four pulmonary veins flow into the left atrium, carrying arterial blood from the lungs. The pulmonary trunk emerges from the right ventricle, through which venous blood enters the lungs. The aorta emerges from the left ventricle, carrying arterial blood to the vessels of the systemic circulation. Oxygen is delivered to the myocardium of the heart through the coronary arteries.
The heart is very sensitive to lack of blood supply (oxygen deficiency). In the case of blockage of a large coronary artery and in the absence of effective alternative blood circulation through other vessels, within 30 minutes the death of cardiomyocytes (muscle cells of the heart) begins in the affected area.
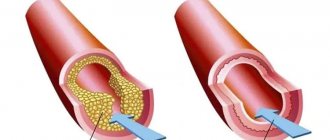
Poor circulation due to atherosclerotic lesions of the coronary arteries in 97-98% of cases is of primary importance in the occurrence of myocardial infarction.
Atherosclerosis can affect either one coronary artery or all three. The degree and extent of narrowing of the artery can vary. When blood pressure increases, the sclerotic inner layer of the vessel (endothelium) is easily damaged, blood penetrates into the plaque, the blood clotting process is activated and a blood clot is formed, which can partially or completely block the vessel.
Where a blood clot can form:
- at the site of rupture of a vulnerable (unstable) atherosclerotic plaque;
- on a defect (erosion) of the endothelium of the coronary artery, not necessarily localized on the surface of the atherosclerotic plaque;
- at the site of hemodynamically insignificant narrowing of the coronary artery.
Coronary artery thrombosis occurs with complete or incomplete parietal occlusion. A thrombus located proximally (closer to the center) in the coronary artery tends to be transported with the blood flow more distally (closer to the vessel wall) and lead to the formation of small foci of necrosis and/or contribute to the expansion of the main area of necrosis.
Great importance in the development of myocardial infarction is attached to the development of spasm of the coronary arteries both with atherosclerosis and with unchanged vessels.
Developing myocardial necrosis can be of various sizes, and necrosis passing through all layers of the heart (transmural) can cause myocardial rupture.
The formation of foci of necrosis in the myocardium is accompanied by changes in the size, shape and thickness of the heart wall, and the remaining myocardium experiences increased stress and undergoes hypertrophy with an increase in volume and mass.
Concomitant conditions such as anemia, inflammation, infection, fever, metabolic or endocrine disorders (in particular, hyperthyroidism) can provoke or aggravate myocardial ischemia.
Risk factors for developing myocardial infarction include:
- hyperlipidemia (violation of the normal ratio of blood lipids);
- smoking,
- diabetes,
- arterial hypertension,
- abdominal obesity,
- psychosocial reasons (stress, depression, etc.),
- low physical activity,
- unbalanced diet and alcohol consumption.
Recurrent myocardial infarction occurs within 28 days of the initial myocardial infarction.
If myocardial infarction develops at a later date, they speak of recurrent myocardial infarction. Classification of myocardial infarction
I. Acute myocardial infarction.
- Acute transmural infarction of the anterior myocardial wall.
- Acute transmural infarction of the lower myocardial wall.
- Acute transmural myocardial infarction of other specified locations.
- Acute transmural myocardial infarction of unspecified localization.
- Acute myocardial infarction, unspecified.
II. Repeated myocardial infarction.
- Repeated infarction of the anterior myocardial wall.
- Repeated infarction of the lower myocardial wall.
- Repeated myocardial infarction of another specified location.
- Repeated myocardial infarction of unspecified localization.
III. Some current complications of acute myocardial infarction.
- Hemopericardium.
- Atrial septal defect.
- Ventricular septal defect.
- Rupture of the heart wall without hemopericardium.
- Rupture of the tendinous chord.
- Rupture of the papillary muscle.
- Thrombosis of the atrium, atrial appendage and ventricle of the heart.
- Other current complications of acute myocardial infarction.
IV. Other forms of acute coronary heart disease.
- Coronary thrombosis not leading to myocardial infarction.
- Dressler's syndrome is post-infarction sclerosis.
- Other forms of acute coronary heart disease.
- Acute coronary heart disease, unspecified.
V. Previous myocardial infarction.
Symptoms of myocardial infarction
During myocardial infarction, as a result of circulatory disorders, metabolic products accumulate in the affected area of the heart, which irritate the receptors of the myocardium and coronary vessels, which is manifested by acute pain. A painful attack leads to the release of adrenaline and norepinephrine from the adrenal cortex.
Pain in the typical course of myocardial infarction is its main symptom. It arises behind the sternum, sometimes it can radiate to the left arm, left shoulder, throat, lower jaw, and to the epigastric region.
In intensity and duration, such pain significantly exceeds a regular angina attack. The pain is not relieved by taking nitroglycerin. The duration of the pain syndrome can vary - from 1 hour to several days. Sometimes myocardial infarction is accompanied by severe weakness, dizziness, headache, vomiting, and loss of consciousness. The patient looks pale, lips turn blue, and sweating occurs.
On the first day of myocardial infarction, tachycardia (rapid heartbeat), rhythm disturbance, and temperature rise to 37-38℃ may be recorded.
In 30% of cases, myocardial infarction in the first hours of its development may manifest itself atypically.
The following clinical options are distinguished:
- asthmatic - occurs as an attack of bronchial asthma (there is shortness of breath, difficulty breathing, a feeling of lack of air);
- gastralgic - characterized by pain in the stomach spreading to the retrosternal space, there may be belching, hiccups, nausea, repeated vomiting, bloating;
- arrhythmic - life-threatening heart rhythm disturbances occur;
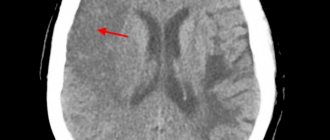
- cerebral – characterized by impaired cerebral circulation (nausea, dizziness, impaired consciousness with the development of fainting are observed);
- asymptomatic - myocardial infarction without a typical pain attack. Due to non-compliance with bed rest and lack of proper treatment, the course is unfavorable.
Diagnosis of myocardial infarction
There are clear criteria for diagnosing myocardial infarction:
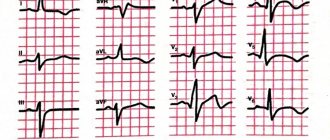
- clinical picture of myocardial infarction;
- picture of myocardial infarction according to ECG data;
- the presence of new areas of the myocardium with reduced blood circulation or impaired myocardial contractility according to instrumental studies;
- detection of coronary artery thrombosis according to angiography.
To confirm the diagnosis, the following laboratory tests are performed:
- determination of the level of biochemical markers of cardiomyocyte damage in the blood;
Myocardial infarction (heart attack) - symptoms and treatment
A patient with an acute heart attack must be promptly transported to the hospital to prevent complications and increase the chances of survival. The system of care for patients with myocardial infarction includes the following stages:
- Pre-hospital stage. Ambulance teams provide assistance and transport the patient to the hospital.
- Hospital stage. Help is provided in specialized vascular departments.
- Rehabilitation stage. Rehabilitation is carried out in special departments of hospitals or specialized cardiological sanatoriums.
- Dispensary observation and outpatient treatment. Clinical examination in the post-infarction period is carried out in regional or city cardiology centers or in cardiology offices of clinics [6].
At the prehospital stage, the following tasks are solved:
- an accurate diagnosis is established. If this fails, it is permissible to establish a tentative syndromic diagnosis as soon as possible;
- The patient is given a nitroglycerin tablet under the tongue (or use a nitro-containing spray) and 0.25-0.35 g of aspirin;
- pain is relieved by administering painkillers;
- acute circulatory failure and heart rhythm disturbances are eliminated;
- the patient is brought out of the state of cardiogenic shock;
- in case of clinical death, resuscitation measures are performed;
- transport the patient to the hospital as soon as possible.
Further therapy is determined by the stage (period) of myocardial infarction. In the acute and very acute period, the goal of treatment is to prevent an increase in the focus of myocardial necrosis, eliminate pain and other symptoms. It is important to restore blood flow through the heart arteries and relieve pain. The intensity of pain during this period is so great that the patient may die due to cardiac arrest. It is necessary to prevent severe complications. When the disease passes into the subacute stage and in the post-infarction period, the goal of therapy is to reduce the risk of attack recurrence and possible complications.
For the treatment of acute myocardial infarction, drugs from various pharmacological groups are used:
Painkillers. Analgesics from the group of narcotic painkillers (morphine, promedol, omnopon) in combination with analgin, antihistamines (diphenhydramine). Neuroleptanalgesia is most effective when a combination of the analgesic fentanyl with the strong antipsychotic droperidol is used. The effectiveness of these drugs is noticeable within a few minutes. Not only pain disappears, but also fear of death, unmotivated anxiety and psychomotor agitation. Tranquilizers (diazepam) can be used to relieve psychomotor agitation. To reduce hypoxia (decreased oxygen in tissues), oxygen inhalation is used using a nasal catheter.
Thrombolytic therapy. It is important to restore blood flow and dissolve blood clots so that the death of the heart muscle does not spread further. The smaller the area of necrosis, the higher the patient’s chances of successful rehabilitation and the lower the risk of life-threatening complications. Immediate use of drugs (preferably within the first hour after an attack) allows you to achieve maximum effectiveness of treatment. A time limit of three hours is allowed. To dissolve a blood clot, thrombolytic drugs are administered intravenously, for example, streptokinase, urokinase, alteplase. The dose depends on the patient's weight.
Restoration of coronary blood flow is also possible with the help of surgical treatment - stenting or coronary artery bypass grafting. A balloon catheter is inserted into a narrow section of the artery under fluoroscopic guidance. In this case, the atherosclerotic plaque is “crushed”, and the lumen of the heart artery increases. Then a stent (metal frame) can be installed into the lumen of the vessel.
Antiplatelet agents. Drugs from this group affect blood cells (platelets and red blood cells). The action of antiplatelet agents prevents platelet aggregation, improving blood flow. The main drug used is aspirin (acetylsalicylic acid). Contraindications to the use of aspirin: bleeding from the gastrointestinal tract, exacerbation of gastric or duodenal ulcers.
P2Y12 platelet receptor inhibitors are also used , which block platelet activation. The main blockers are ticagrelor, prasugrel and clopidogrel.
Intravenous/subcutaneous anticoagulants. , unfractionated heparin intravenously, is used to prevent deep vein thrombosis (DVT) and pulmonary embolism (PE) . Enoxaparin , which is also used to prevent venous thromboembolism, is administered subcutaneously.
To limit the area of myocardial ischemia and necrosis, it is necessary, in addition to restoring blood flow in the arteries of the heart, to reduce the hemodynamic load on the heart. Nitrates and beta blockers are used for this purpose.
Nitrates. They have an analgesic effect, reduce myocardial oxygen demand, increase coronary and collateral (bypass) blood flow, reduce the load on the heart muscle, and limit the size of the myocardial lesion. Their combination with beta blockers is especially effective, leading to rapid positive ECG dynamics and reducing the risk of sudden death [10].
Beta-blockers have an antiarrhythmic effect. The purpose of using beta-blockers (propranolol, metoprolol, atenolol) is to reduce the frequency and force of heart contractions, which will help reduce the load on the heart and the myocardial oxygen demand. Beta blockers continue to be used indefinitely in the absence of side effects and contraindications [1].