Heart failure is associated with decreased heart function. The heart muscle cannot produce the energy needed to pump the required amount of blood throughout the body.
In Russia alone, about 7 million people suffer from heart failure. In people over 70, one in four people are affected, with men typically affected at a much younger age than women. The risk for men is approximately one and a half times higher than for women. In Russia, diseases of the circulatory system are the most common cause of death.
- What is heart failure?
- What causes heart failure?
- What are the types of heart failure and what are their symptoms? Left-sided heart failure
- Right-sided heart failure
- Global heart failure
- Systolic heart failure
- Diastolic heart failure
- Chronic heart failure
- Acute heart failure
What is heart failure?
With a healthy heart, oxygen-rich blood from the left ventricle is pumped through the body to the organs, providing them with oxygen and nutrients. After supplying the organs, low-oxygen blood returns from the body to the right side of the heart, from where it is transported to the lungs. In the lungs, the blood is enriched with oxygen so that it can again be pumped throughout the body through the left ventricle.
Heart failure is a weakening of the pumping function of the heart. Typically, either the right side of the heart is affected (right-sided heart failure) or the left side of the heart (left-sided heart failure). With advanced heart failure, both sides of the heart can be affected (global heart failure). Heart failure can also be chronic or acute in nature. Chronic heart failure is more common than acute heart failure, which occurs suddenly and unexpectedly. Acute heart failure can occur suddenly against the background of an acute cardiovascular accident and/or decompensated heart failure.
Diagnosis and assistance
When treating pathologies of the cardiovascular system, doctors conduct a thorough diagnosis of the patient and provide qualified assistance according to the identified problems.
Diagnostics
The main diagnostic measures in the development of a pathological condition are aimed at examining the patient, assessing his symptoms and determining the form of deficiency. To give an accurate conclusion, a specialist studies the person’s history and determines what factors could lead to the pathology. After assistance is provided, the patient is sent to a hospital, where examinations of the circulatory and cardiac systems are prescribed:
- ECG;
- phlebography;
- auscultation (listening) of arterial vessels;
- sphygmography, etc.
Our clinic has all the necessary equipment for diagnostics, which allows us to accurately determine the etiology of the pathological process.
First aid
Help for acute vascular insufficiency should be provided without delay. If you faint, do the following:
- the person is laid horizontally;
- loosen the collar of clothing for air access;
- splash your face with water;
- give ammonia to smell;
- call an ambulance.
Upon arrival, the doctor injects the patient with caffeine or adrenaline and then admits him to a medical facility. If shock develops, it is necessary to urgently take the person to the hospital. The faster his resuscitation is performed, the lower the risk of death. If necessary, stop the bleeding and carry out other procedures, focusing on the reasons that led to the attack.
What are the types of heart failure and what are their symptoms?
Each type of heart failure has different symptoms, and the symptoms can vary in intensity. However, the main symptom of heart failure is difficulty breathing during exercise or at rest. Warning signs may include sweating with mild exercise, an inability to lie flat, tightness in the chest, or swelling in the legs.
Left-sided heart failure
The left side of the heart is responsible for pumping oxygen-rich blood throughout the body to the organs. In left-sided heart failure, the pumping function of the left ventricle is limited, resulting in insufficient oxygenated blood to be pumped throughout the body. Instead, the blood remains in the pulmonary circulation, which can lead to fluid in the lungs (pulmonary edema), difficulty breathing, throat irritation, a rattling sound when breathing, weakness, or dizziness.
It is most often caused by coronary artery disease (CHD), high blood pressure or a heart attack, and less commonly by problems with the heart muscle or heart valves.
Left-sided heart failure may present acutely or develop over time. It is usually first noticed by shortness of breath from physical activity. When severe, it can even lead to hypotension (low blood pressure) at rest.
Right-sided heart failure
The right side of the heart is responsible for returning low-oxygen blood back to the lungs. In right-sided heart failure, the right ventricle does not work properly. This causes increased pressure in the veins, forcing fluid into the surrounding tissue. This leads to swelling, especially in the feet, toes, ankles and legs. This can also lead to an urgent need to urinate at night when the kidneys receive better blood circulation.
The cause is most often an acute or chronic increase in pulmonary circulatory resistance. Caused by pulmonary diseases such as pulmonary embolism, asthma, severe emphysema, chronic obstructive pulmonary disease (COPD, most commonly due to tobacco use), or left-sided heart failure. Rare causes include heart valve problems or heart muscle disease.
Global heart failure
When both the left and right sides of the heart are affected, it is called global heart failure. There are symptoms of left and right heart failure.
Systolic and diastolic heart failure
Systolic heart failure is associated with loss of normal functioning of heart muscle cells or external impairment of pumping function. Blood enters the lungs, and the organs do not receive enough oxygen.
In diastolic heart failure, the elasticity of the ventricle is lost, causing it to not relax and fill appropriately. One of the most common causes of diastolic dysfunction is high blood pressure. Due to increased resistance in the arteries, the heart must work harder. The elasticity of the heart muscle decreases, and less blood can be pumped from the ventricles to the body between contractions. This results in the body not receiving enough blood and nutrients.
Heart valve disease can also cause the heart muscle to thicken. The heart muscles become stiffer and less elastic due to the accumulation of proteins. Symptoms range from cough to shortness of breath.
Chronic and acute heart failure
Chronic heart failure is a progressive disease that takes months or years to develop and is more common than acute heart failure. In chronic heart failure, symptoms are often not taken seriously because the body is able to compensate over a long period of time or symptoms are associated with increasing age. Symptoms reflect either left- or right-sided heart failure.
Acute heart failure occurs suddenly, minutes or hours after a heart attack, when the body can no longer compensate. Some symptoms include:
- severe difficulty breathing and/or coughing;
- Gurgling sound when breathing;
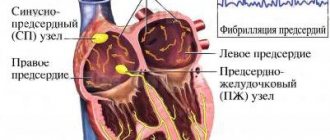
- Heart rhythm disturbances;
- Pallor;
- Cold sweat.
Clinical manifestations
The syndrome usually develops suddenly
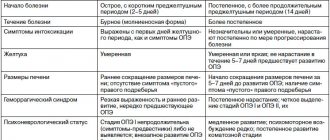
The clinical picture of AHF is always accompanied by a decrease in blood pressure and directly depends on the severity of the condition; this is presented in more detail in the table.
Table 1. Clinical forms of pathology
| Name | How does it manifest clinically? |
| Fainting woman fainting | The patient suddenly feels weak, dizzy, and has “floaters” flashing before his eyes. Consciousness may be preserved or absent. If after 5 minutes the patient does not come to his senses, then fainting is accompanied by convulsions; as a rule, this rarely happens and with properly organized help the person’s condition quickly normalizes |
| Collapse Retardation during collapse | This condition is much more severe than fainting. The patient's consciousness can be preserved, but there is severe inhibition and disorientation in space. Blood pressure is sharply reduced, the pulse is weak and thready, breathing is shallow and rapid. The skin is pale, acrocyanosis and sticky cold sweat are observed. |
Shock State of shock | Clinically, shock is not much different from collapse, but in this condition a sharp depression of the heart and other vital organs develops. Due to severe hypoxia, the brain suffers, against the background of which degenerative changes can develop in its structure |
What classes is heart failure divided into?
There are several classifications of heart failure:
- Classification according to V. Kh. Vasilenko, N. D. Strazhesko, G. F. Lang;
- Classification of acute heart failure according to the Killip scale;
- And the most common is the New York Heart Association classification.
According to the New York Heart Association (NYHA) functional classification, heart failure is classified into classes I-IV depending on the severity of symptoms and limitation of physical activity.
Heart failure is divided into four classes depending on the severity of symptoms:
- NYHA I: heart disease without any restrictions on physical activity. Normal activity does not cause increased fatigue, palpitations, or difficulty breathing.
- NYHA II: Heart disease causing moderate limitation in daily activities. No symptoms at rest.
- NYHA III: Heart disease causing marked limitation in daily activities. Simple activities such as brushing your teeth, eating, or talking cause fatigue, palpitations, or difficulty breathing. There are no symptoms at rest.
- NYHA IV: Heart disease that causes symptoms at rest (and with any degree of light physical activity).
Heart failure significantly reduces quality of life. Patients often experience great frustration with physical limitations and tend to withdraw from social life. For this reason, psychological disorders such as depression are often present in addition to the expected physical symptoms.
Therapeutic measures
Assistance for vascular insufficiency of any type should be provided to the patient immediately:
- the patient is placed in a horizontal position so that his limbs are slightly elevated;
- clothing that can compress the chest and abdomen is either removed altogether or unbuttoned;
- moisten a cotton swab with ammonia and wave it a little near the victim’s nose.
Treatment of vascular insufficiency involves the administration of the following synthetic medications:
- orciprenaline sulfate;
- sodium benzoate;
- mesatone;
- caffeine;
- ascorbic acid;
- glucose;
- strychnine.
How is heart failure diagnosed?
Diagnosis begins with a comprehensive assessment of a person's medical history, paying particular attention to symptoms (onset, duration, manifestation). This helps classify the severity of the symptom. The heart and lungs are examined. If a heart attack or rhythm disorder is suspected, a 12-lead resting ECG is performed. In addition, echocardiography and complete blood count. The need for catheterization is determined individually.
Treatment
First medical aid for AHF directly depends on the type of pathology.
Fainting
First aid for fainting
As a rule, treatment of fainting occurs without the use of medications.
Emergency care for fainting type of fainting consists of the following actions:
- place the patient in a horizontal position with the leg end raised;
- unbutton the buttons of your shirt and free yourself from clothing that is constricting your chest;
- provide access to fresh cool air;
- Spray your face with water or wipe your forehead and cheeks with a wet cloth;
- give warm sweet tea or weak coffee to drink if the patient is conscious;
- in the absence of consciousness, pat your cheeks and apply cold to your temples.
Cup of hot sweet coffee
If the above actions are ineffective, you can inject vasoconstrictor drugs, for example, Cordiamin.
Collapse
The woman in the photo suddenly felt ill
First aid for collapse is aimed at eliminating the causes that provoked the development of this condition. First aid for collapse consists of immediately placing the patient in a horizontal position, raising the leg end and warming the patient.
If the person is conscious, then you can give him hot sweet tea. Before transport to the hospital, the patient is given an injection of a vasoconstrictor drug.
Syringe for intravenous injection
In a hospital setting, the patient is administered medications that eliminate both the symptoms of vascular insufficiency and the causes of this pathological condition:
- drugs that stimulate the respiratory and cardiovascular centers - these drugs increase the tone of the arteries and increase the stroke volume of the heart;
- vasoconstrictors - adrenaline, Dopamine, Norepinephrine and other drugs that quickly increase blood pressure and stimulate the heart are administered intravenously;
- infusion of blood and red blood cells - required in case of blood loss to prevent shock;
- carrying out detoxification therapy - droppers and solutions are prescribed that quickly remove toxic substances from the blood and replenish the volume of circulating fluid;
- Oxygen therapy – prescribed to improve metabolic processes in the body and saturate the blood with oxygen.
Possible nursing problems with AHF of the collapse type are the difficulty of giving the patient something to drink if his consciousness is impaired, and of administering the drug intravenously at low pressure - it is not always possible to immediately find a vein and get into the vessel.
Important! Saline solutions are not effective if the collapse is caused by the deposition of blood into the intercellular space and internal organs. In such a situation, to improve the patient's condition, it is necessary to inject colloidal solutions into the plasma.
Shock
Treatment of shock consists of taking measures aimed at improving the systemic functions of the body and eliminating the causes of this condition.
The patient is prescribed:
- painkillers – in case of injuries and burns, before carrying out any actions, it is necessary to administer painkillers to the patient, which will help prevent the development of shock or stop it in the erectile stage;
- oxygen therapy – the patient is given humidified oxygen through a mask to saturate the blood with oxygen and normalize the functioning of vital organs; if consciousness is depressed, the patient is given artificial ventilation;
- normalization of hemodynamics - medications are administered that improve blood circulation, for example, red blood cells, colloidal solutions, saline solutions, glucose and others;
- administration of hormonal drugs - these drugs help to quickly restore blood pressure, improve hemodynamics, and relieve acute allergic reactions;
- diuretics - prescribed for the prevention and elimination of edema.
Important! With the development of AHF, all medications should be administered intravenously, since due to impaired microcirculation of tissues and internal organs, the absorption of medications into the systemic bloodstream changes.
How is heart failure treated?
For chronic heart failure, medications (such as ACE inhibitors, beta blockers and diuretics) are used. Medicines are used to prevent complications and improve quality of life. ACE inhibitors and beta blockers can prolong life, but they must be taken regularly to achieve a beneficial effect.
In addition, rhythm therapy (to treat cardiac arrhythmias) and implantation of a three-chamber pacemaker are used. The latter ensures timely activation of the atria and both ventricles. A defibrillator is also often implanted as part of a pacemaker to counteract dangerous heart rhythm disturbances in the setting of severe heart failure. This treatment is also known as resynchronization therapy. An important part of successful treatment is physical therapy.
Prevention of vascular insufficiency
Preventive measures to prevent vascular insufficiency consist of preventing diseases that can cause the pathological condition. It is necessary to adhere to a healthy diet, control blood pressure, and if you have hypertension, take medications prescribed by your doctor. It is advisable to give up bad habits and foods rich in cholesterol. Regular walks and exercise are recommended.
If symptoms of heart or vascular diseases appear, you should immediately contact a specialist to diagnose and treat them. The Euromedprestige clinic is ready to conduct a comprehensive examination and help you avoid the development of pathology.
First aid for AHF
A patient with AHF must immediately receive emergency care, since cardiogenic shock may occur during a heart attack. At the same time, his skin turns pale, his blood pressure drops sharply, severe pain appears, and his pulse is practically not palpable. If you do not respond in time, swelling of the kidneys and lungs can quickly develop, which can lead to death.
In case of AHF, first aid is provided at the scene of the incident, while it is necessary to reduce the load and ensure the redistribution of blood flow by performing the following actions:
- Place the patient in a comfortable sitting position; to do this, lower his legs to the floor and raise his back.
- It is better to immerse your feet in a basin of hot water, reducing the flow of blood to the heart.
- Remove the patient from clothing and open the windows, ensuring maximum flow of fresh air.
- Call emergency doctors and report the symptoms of an attack.
- Apply a tourniquet in the groin area to each leg alternately (20 minutes), which will reduce the flow of blood into the myocardium.
- Provide the patient with emotional and physical peace; he is strictly forbidden to get up and walk.
If there are signs of AHF, you need to measure your blood pressure. If the upper reading is more than 90 mmHg, then 1 tablet of nitroglycerin should be placed under the patient’s tongue. After this, you need to monitor the pressure all the time. If necessary, you can give 1 more tablet after 7 minutes, but not more than 4 times.
Patients suffering from heart disease or hypertension with severe swelling of the legs and shortness of breath should always carry a first aid kit with medications prescribed by the attending physician. Then, at the first signs of AHF, people around you will be able to provide emergency assistance.