Decongestants: from proven remedies to improved combinations
The modern classification of rhinitis still continues to be revised [1,2]. This is due to the fact that the universal clinical signs of rhinitis can have different pathogenesis: infectious, allergic, occupational, hormonal, drug. Doctors often make a diagnosis at their own discretion, continuing to use different and mutually exclusive concepts to define the same conditions: “rhinopathy”, “rhinosinusopathy”, “vasomotor, allergic”, etc. This leads not only to errors when conducting epidemiological analysis, but and to difficulties and difficulties in interpreting the results of clinical studies. According to the report of the International Consensus on the Diagnosis and Treatment of Rhinitis (1996), rhinitis is classified as follows: allergic (seasonal and year-round), infectious (acute and chronic) and other types (idiopathic, occupational, hormonal, drug, caused by irritants, food, psychogenic, atrophic) [1]. A slightly different classification used in Russia distinguishes allergic, infectious, non-allergic eosinophilic, vasomotor, hypertrophic and atrophic rhinitis. Depending on the duration, rhinitis is divided into acute and chronic [3]. According to foreign data, rhinitis is proposed to be classified into allergic and non-allergic, the latter being divided into subtypes not associated with allergens, infectious agents and anatomical defects - non-allergic rhinopathy (vasomotor rhinitis), non-allergic rhinitis with eosinophilia, atrophic rhinitis, drug-induced rhinitis, hormonal-induced rhinitis, including rhinitis of pregnancy, and nasal liquorrhea [4]. The most complete classification of rhinitis according to T.I. Garashchenko (1998), which divides rhinitis into 6 positions: etiology, clinical course, morphological nature of the pathological process, periods of the disease, functional state and age characteristics, but in real clinical practice it is complex and not entirely convenient. However, most current classifications are based on the etiological factor contributing to the occurrence of rhinitis and its morphological characteristics. However, the issue of classification of rhinitis still remains controversial. Thus, the morphological picture of rhinitis can undergo changes as the disease progresses: hypertrophy of the mucous membranes of the nasal turbinates can be the final stage of any form of rhinitis, except atrophic. Post-traumatic or postoperative rhinitis, found in some classifications, is almost always bacterial in nature. We should not forget that rhinitis can be a manifestation of other diseases (sinusitis, adenoiditis, liquorrhea). The exception is allergic rhinitis, for which there is the greatest certainty in both diagnosis and treatment strategy. Thus, according to the Allergic rhinitis and its impact on asthma initiative (ARIA, 2001), allergic rhinitis is classified into intermittent (seasonal) and persistent (year-round) and their severity is determined as mild, moderate or severe [5,20]. According to ICD-10, the following classification is considered for statistical processing: J00 Acute nasopharyngitis (runny nose) J30 Vasomotor and allergic rhinitis • J30.0 Vasomotor rhinitis • J30.1 Allergic rhinitis caused by pollen • J30.2 Other seasonal allergic rhinitis • J30.3 Other allergic rhinitis • J30.4 Allergic rhinitis, unspecified J31 Chronic rhinitis, nasopharyngitis and pharyngitis • J31.0 Chronic rhinitis • J31.1 Chronic nasopharyngitis • J31.2 Chronic pharyngitis. Most often, general practitioners encounter rhinitis of viral and allergic etiology. Infectious diseases of the upper respiratory tract are diagnosed year-round, with a peak incidence in the autumn-winter period and are most often associated with viral infections. According to statistics, acute respiratory viral infection (ARVI) is the most common infectious disease in developed countries. On average, an adult gets ARVI at least 2–3 times per year, and children 2–3 times more often. The duration of acute viral rhinitis is 7–10 days. The danger is posed by complications that can develop against the background of rhinitis: inflammation of the paranasal sinuses (sinusitis, frontal sinusitis, ethmoiditis) and otitis media. As for allergic rhinitis, epidemiological data indicate that it affects, to varying degrees of severity, from 10 to 30% of adults and up to 40% of children [4–7]. The importance of this problem is also due to the fact that allergic rhinitis is closely related to such very common diseases as acute and chronic sinusitis, allergic conjunctivitis, and is one of the decisive risk factors for the development of bronchial asthma or already accompanies and aggravates it. For example, of 2580 patients with bronchial asthma (62% with atopy), 80.7% had indications of seasonal rhinitis, and in 72% of cases, exacerbation of rhinitis was accompanied by worsening asthma. In cases where asthma control was achieved (40.3% of patients), most patients used drugs to treat rhinitis [8]. Regardless of the etiology, the main pathogenetic link in the vast majority of diseases of the nasal cavity, paranasal sinuses and middle ear is swelling of the mucous membrane. It is impossible to consider rhinitis and not take into account its close relationship with the paranasal sinuses and the auditory tube. Swelling of the mucous membrane and hypersecretion in the nasal cavity inevitably complicate ventilation and impair mucociliary clearance, which creates conditions for the development of acute inflammation of the middle ear and paranasal sinuses, which, as a rule, are complicated by the addition of a bacterial infection. In most cases, patients with acute inflammatory diseases of the upper respiratory tract begin treatment primarily with available, over-the-counter and “harmless” symptomatic drugs. The share of medicines aimed at treating runny nose and cough in Russia is about 30% of the entire medicine market (according to DSM Group). Research shows that for 70–80% of patients the greatest problem that worsens the quality of life is the feeling of nasal congestion [8,13,14], so an important task is to restore nasal breathing. And this is due not only to the discomfort that rhinitis causes, but also to the fact that swelling, hypersecretion and a sharp decrease in the activity of the ciliated epithelium create ideal conditions for the attachment of infectious agents. In this regard, it is necessary to facilitate nasal breathing and elimination of secretions from the nasal cavity by prescribing local vasoconstrictors. Rhinorrhea and nasal congestion are natural stages of the inflammatory process, and therefore the rate at which this condition progresses depends on the effectiveness of anti-inflammatory treatment. However, in practice, anti-inflammatory nasal drugs are not often used, because in each case, an individual choice of drug is required depending on the etiology of rhinitis, which presents certain difficulties. Unfortunately, there are no universal anti-inflammatory drugs. At the same time, vasoconstrictor over-the-counter nasal medications, which are suitable for a wide range of patients, quickly alleviate the patient’s condition, although they do not affect the nature of the inflammation. The use of local therapy allows you to quickly stop the pathological process, avoid complications that accompany rhinitis and, in some cases, abandon the use of antibiotics, mucolytics and systemic anti-inflammatory drugs. Local therapy has a number of huge advantages: a quick effect, a direct effect on the mucous membrane, the creation of a high concentration of the drug in the area of inflammation, the ability to use small concentrations of the drug, the absence of a systemic effect. The form of release of the drug is also of great importance. Nasal drops are difficult to dose, since most of the instilled drug flows down the bottom of the nasal cavity into the pharynx. In this case, the required therapeutic effect is not achieved, and there is a risk of overdose. Therefore, it is more preferable to use nasal sprays that allow uniform irrigation of the nasal mucosa in small concentrations [15]. There are a huge variety of decongestants on the domestic market: “Naftizin”, “Xymelin”, “Nazol”, “Dlyanos”, “Tizin”, “Nazivin”, “Otrivin”. They all differ in composition, duration of action, and have advantages and disadvantages, but the mechanism of action of all drugs is fundamentally the same. Decongestants, being α-adrenergic agonists, constrict the vessels of the nasal mucosa, as a result of which swelling and hyperproduction of mucus by goblet cells are reduced. All drugs according to their duration of action can be divided into short-acting, medium-acting and long-acting. Short-acting derivatives include naphazoline and tetrizoline derivatives - their effect lasts no more than 4-6 hours, which requires their use 4 times. They negatively affect the ciliated epithelium of the nasal cavity. Medium-lasting decongestants (up to 8–10 hours) include xylometazoline derivatives. Oxymetazoline derivatives are long-acting vasoconstrictor drugs - 10-12 hours. Thanks to this, it is enough to use them 2-3 times a day. The long-term effect of these α2-adrenergic agonists is explained by their slow elimination from the nasal cavity due to a decrease in blood flow in the mucous membrane. The severity of the anti-edematous effect of all imidazoline derivatives is approximately the same. In 20 minutes. after their use, approximately 60% of their maximum effect develops, which manifests itself after 40 minutes. However, the duration of their action is very different: after 4 hours, the decongestant effect of indanazoline, naphazoline and tetrizoline is no longer present, but is retained by xylometazoline, oxymetazoline, and tramazoline. 8 hours after application to the mucous membrane, only oxymetazoline retains a pronounced effect [16]. The undoubted advantages of oxymetazoline are the absence of toxic effects on ciliated epithelial cells, which preserves mucociliary clearance [17,18]. All decongestants have class-specific undesirable effects: burning sensation, sneezing, congestion (reactive hyperemia), dry mucous membranes. The development of reactive hyperemia and dry mucosa can be avoided by using additional components in decongestants, such as menthol, camphor, and eucalyptol. These natural components not only have moisturizing and anti-inflammatory effects, but also contribute to a more uniform distribution of the main vasoconstrictor drug and are perfectly combined with it. An additional benefit is the anti-inflammatory effects of these substances. Thus, eucalyptol is a strong inhibitor of the production of cytokines such as TNF-α and interleukin-1, and thus reduces excess secretion of the mucous membranes of the respiratory tract, which enhances the effect of the main substance - oxymetazoline [19]. In addition, eucalyptol and camphor have antimicrobial and antifungal activity, in particular against Cl. perfringens and C. albicans [21]. As for the evidence base for the effectiveness of decongestants, Taverner D. et al. The meta-analysis included 7 randomized placebo-controlled studies assessing the effectiveness of oral and local decongestants in adults and children for ARVI (The Cochrane Library, MEDLINE, OLDMEDLINE, EMBASE). A statistically significant 6% reduction in nasal congestion was demonstrated after a single dose of decongestants compared to placebo. With repeated use of vasoconstrictors, the reduction in nasal congestion was reduced to 4%. Two studies demonstrated safety and few side effects. The authors concluded that a single dose provided relief of nasal breathing with continued effectiveness for 3–5 days. No studies have been conducted in children [9]. Previously, the same authors showed that 286 patients significantly - by 13% - noted a subjective decrease in symptoms of nasal congestion after using decongestants compared to placebo; with repeated use, the effect decreased slightly [10,11]. In the EPOS guidelines, the category of evidence for the use of decongestants for acute sinusitis is assessed as Ib(–), and the strength of recommendation is assessed as D (evidence category IV, the lowest). Therefore, topical corticosteroids are recommended as primary therapy (recommendation A). However, this cannot be excluded, and in the case of a purulent form, the simultaneous administration of decongestants is actively recommended [12]. According to the ARIA concept, decongestants are indicated for any form and severity of allergic rhinitis as symptomatic therapy, but not more than 10 days [5]. Today, Noxprey has appeared on the market - oxymetazoline in combination with eucalyptol, camphor, menthol in the form of a spray and characterized by all the advantages of its constituent substances: the duration of action of oxymetazoline along with a minimal toxic effect on the function of the ciliated epithelium, antimicrobial and immunostimulating properties of essential oils, preservation of natural moisture of the nasal mucosa. Noxprey is available in the form of a spray that evenly irrigates the nasal cavity and eliminates accidental overdose and can be used only 2 times a day. Currently, in the arsenal of general practitioners and otorhinolaryngologists there is a sufficient number of effective and safe pathogenetic drugs for the treatment of diseases of the upper respiratory tract. The main goals of such therapy are not only to alleviate the patient’s condition and shorten the duration of the disease, but also to prevent the development of complications. When choosing a drug intended for the symptomatic treatment of rhinitis, sinusitis, otitis, preference should be given to drugs with a good safety profile, long-term action and additional auxiliary effects. Literature 1. Russian rhinology. 1996, No. 4. https://www.rhinology.ru. 2. Russian rhinology. 1997, No. 2. https://www.rhinology.ru. 3. Rational pharmacotherapy of respiratory diseases. – M.: Litterra, 2004. – P. 261–289. 4. Tran NP, Vickery J, Blaiss MS Management of rhinitis: allergic and non-allergic. // Allergy Asthma Immunol Res. 2011 Jul;3(3):148–56. 5. Bousquet J., van Cauwenberge P., Khaltaev N. Allergi. rhinitis and its impact on asthma. ARIA workshop report. // J. Allergy Clin. Immunol 2001;108:147–S334. 6. Ilyina N.I. Epidemiology of allergic rhinitis. // Ross. rhinol. – 1999. – No. 1. – P. 23–24. 7. Rhinitis. Mechanisms and management. Edited by Ian Mackay. 1989. 8. Florou A., Vakali S., Vlasserou F., Gratziou C. Epidemiology of allergic rhinitis in asthmatic patients in Greece. ERS2011. // Clin Ther. 2008 Apr;30(4):573–86. 9. Taverner D., Latte GJ WITHDRAWN: Nasal decongestants for the common cold. Cochrane Database Syst Rev. 2009 Apr 15;(2):CD001953. 10. Taverner D., Latte J., Draper M. Nasal decongestants for the common cold. Cochrane Database Syst Rev. 2004;(3):CD001953. 11. Schroeder K., Fahey T. Over–the–counter medications for acute cough in children and adults in ambulatory settings. Cochrane Database Syst Rev. 2004 Oct 18;(4):CD001831). 12. Ryazantsev S.V. Comparison of Russian standards for the treatment of acute sinusitis with the international EPOS program. // Consilium Medicum. – 2008. – T. 10. – No. 10. 13. Roper Public Affairs Group of NOP World. Impact of nasal congestion among allergic rhinitis sufferers. May–June 2004. 14. Nathan RA The pathophysiology, clinical impact, and management of nasal congestion in allergic rhinitis. // Clin Ther. 2008 Apr;30(4):573–86. 15. Ryazantsev S.V. Modern decongestants in the complex therapy of acute and chronic diseases of the ENT organs. https://www.medicusamicus.com. 16. Hochban W., Althoff H., Ziegler A. Nasal decongestion with imidazoline derivatives: acoustic rhinometry measurement // Eur J Clin Pharmacol. 1999 Mar;55(1):7–12. 17. Zaplatnikov A.L., Ovsyannikova E.M. Rational use of nasal decongestants for acute respiratory viral infections in children. // Russian medical journal. – 2004. – T. 12. – No. 1. 18. Deitmer T., Scheffler R. The effect of different preparations of nasal decongestants in ciliary beat frequency in vitro. // Rhinology 1993; 31: 151–3. 19. Juergens UR, Engelen T., Racke K., Stober M., Gillissen A., Vetter H. Inhibitory activity of 1,8-cineol (eucalyptol) on cytokine production in cultured human lymphocytes and monocytes. // Pulm Pharmacol Ther. 2004;17(5):281–7. 20. Lopatin A.S., Gushchin I.S., Emelyanov A.V. and others. Clinical recommendations for the diagnosis and treatment of allergic rhinitis // Consilium medicum. – 2001. – Appendix: 33–44. 21. Sokmen A., Vardar-Unlu G., Polissiou M., Daferera D., Sokmen M., Donmez E. Antimicrobial activity of essential oil and methanol extracts of Achillea sintenisii Hub. Mor. (Asteraceae). // Phytother Res. 2003 Nov;17(9):1005–10.
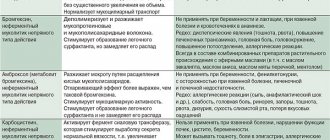
Side effects and contraindications
Side effects that occur with long-term use and overdose of drugs with a vasoconstrictor effect include dryness of the nasal mucosa. Rarely, urinary retention, signs of tachycardia, and decreased clarity of vision may occur. Persons participating in sports competitions are not recommended to use drugs based on phenyephrine, ephedrine and pseudoephedrine, as they have an stimulating effect and, during exercise, negatively affect the state of the cardiovascular system.
If rhinitis, runny nose and nasal congestion begin in children, you should consult a doctor before starting use. He will help you choose the safest and most effective drug, based on the degree of development of symptoms. Without a doctor's recommendation, children are not recommended to use medications containing the following substances:
- naphazoline at a concentration of 0.05 – for children under 12 years of age;
- tetrizoline at a concentration of 0.1% – for children under 6 years of age;
- phenylephrine 0.25% – children under 6 years of age;
- naphazoline 0.025 – up to 6 years.
When taking vasoconstrictors on your own without a doctor’s prescription, it is worth remembering that the duration of the course should not exceed 5–7 days, and if there is no improvement in the condition within three days of taking the drugs, you must stop taking them and consult a doctor.
How to prepare a natural decongestant
Thanks to the properties of its ingredients, this natural anticongestant helps reduce the amount of mucus and swelling of the mucous membrane; breathing becomes easier.
Rainy and cold autumn is the right time to learn how to prepare a good natural decongestant at home, a remedy for relieving congestion and swelling of the mucous membranes .
In such weather, many suffer from colds or flu; in this case, the nose and respiratory tract are usually stuffy. The remedy we offer helps relieve these symptoms of the disease.
It is simple and effective, and - very importantly - does not give the negative side effects that some medications do. Do you want to try it? Write down our recipe!
Beneficial properties of a natural anti-congestant
This natural decongestant is good for the whole family, including very young members. Its natural ingredients are readily available, inexpensive and help the body fight disease thanks to the following beneficial properties:
Subscribe to our INSTAGRAM account!
- Antivirus action
- Antibacterial and anticongestive (vasoconstrictor) properties
- Stimulating the immune system
- Anti-inflammatory effect
This anticongestant reduces the production of mucus, which reduces swelling of the mucous membrane and makes breathing easier. It helps with flu and colds, as well as allergic rhinitis.
Ingredients
- Half a spoon of ground turmeric (5 g)
- Lemon juice
- 3 spoons of honey (90 g)
- 3 spoons of apple cider vinegar (60 ml)
- Half a glass of water (100 ml)
- Pinch of cayenne pepper
- 3 eucalyptus leaves
How to cook it?
- Add eucalyptus leaves to half a glass of water and start heating it. Then add a pinch of cayenne pepper and ground turmeric.
- When the water boils, turn off the heat. After this, add honey, apple cider vinegar and lemon juice. Mix well. The drink should not be too thick.
- Now we carefully filter the natural anti-congestant so that, for example, eucalyptus leaves do not remain in it.
- We take it in two spoons: two spoons in the morning and two spoons before bed. Children can be given one spoon, also in the morning and evening.
Subscribe to our Yandex Zen channel!
This product can be stored in the refrigerator for a couple of days. It should be taken neither cold nor too hot, but slightly warm. Almost room temperature.
Other means for cleansing the nose and nasopharynx
In addition to this natural anti-congestant, other remedies can be used to relieve colds. Write down:
Aloe vera infusion with honey and lemon
It is very good to take it in the morning when we have a cold. You need to take a spoonful of aloe vera gel and drop it into boiling water to make a decoction. Very simple. Then add the juice of half a lemon and a spoonful of honey. Take this infusion warm, it helps a lot with colds.
Onion inhalations
This is an old, traditional remedy. Many people find it effective. How it's done? Cut the onion into four parts and leave it overnight on the table next to the bed. The smell of onions (so characteristic), its evaporation acts as a natural anti-congestant and antibiotic.
Mint infusion
Easy to prepare, tasty and effective. It is good to take it in the afternoon. How to cook it? Bring a glass of water to a boil and add five mint leaves. It should be a decoction. Then this decoction cools down for about five minutes, and you can drink it. You need to pour it into a large cup, and, covering it with your palms, bring it to your face.
Before drinking this infusion, inhale the mint vapor so that it reaches the nasal cavity. Relax and feel the exquisite and relaxing aroma of mint. You will feel rested. When the drink has cooled down a little, start drinking it. This is another excellent anti-congestant.
Salty water
This is also a well-known procedure that helps reduce inflammation of the nasopharynx and speed up recovery. Heat a glass of water and dissolve a spoonful of salt in it. There is no need to drink this water. It is necessary to gargle and throat and spit out this water.
The water should not be hot. In addition to the saline solution, you can use a baking soda solution (one spoon per glass of water). You can drink the soda solution in small sips throughout the day. This remedy is also very effective. Published by econet.ru.
on the topic of the article here
The materials are for informational purposes only. Remember, self-medication is life-threatening; consult a doctor for advice on the use of any medications and treatment methods.
PS And remember, just by changing your consumption, we are changing the world together! © econet
Source: https://econet.ru/articles/kak-prigotovit-naturalnyy-antikongestant