Shortness of breath, constant weakness, unexplained swelling, chest pain - grounds for a cardiological examination. The listed phenomena may indicate a risk of chronic heart failure. The first mild symptoms should not be ignored. Without appropriate therapy, the condition will worsen. The IMMA medical clinics provide therapeutic and cardiological appointments.
In our clinics you can:
- Get a consultation with a cardiologist;
- Take an ECG and get a professional interpretation of the results;
- Complete the ABPM procedure;
- Undergo Holter monitoring;
- Take advantage of other services of our clinics.
For more details and any questions, please contact the number listed on the website
Congestive heart failure - decreased contractions of the heart muscle. This pathological condition is not an independent disease, it is a consequence of various disorders of the cardiovascular system.
The prevalence of heart failure among the population is constantly growing, the disease is considered a social problem along with oncology and AIDS. The reasons for the spread are different: poor environmental conditions, sedentary lifestyle, ignoring healthy eating rules, bad habits. Inattention to health leads to various damage to the circulatory system. Heart failure is a common complication.
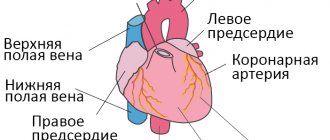
About the structure of the cardiovascular system
The heart is a unique organ on which human life depends. It works without rest, has its own control center, which sends electrical impulses that stimulate muscle contractility.
The structure of the heart is widely known: it has two ventricles and two atria. By contracting, they ensure blood circulation through two vascular systems: the small and large blood circles. To more accurately explain the characteristics of different types of heart failure, it is necessary to mention the characteristics of blood flow.
The systemic circulation involves the flow of blood from the left ventricle into the aorta, oxygenation of all important organs and limbs and the return of venous blood to the right atrium. The pulmonary circulation is the flow of blood from the right ventricle to the lungs and the movement of oxygenated blood into the left atrium.
Symptoms of heart failure depend on which part of the heart is affected. This is reflected in disruption of the functioning of blood circulation.
Heart failure, depending on the nature of its course, can be of two types. The chronic form develops over a long period of time and has several stages. Acute heart failure progresses rapidly. The duration of the process is from an hour to two days. This condition requires urgent hospitalization.
The classification of heart failure based on the localization of the pathology distinguishes several types:
- Left ventricular failure;
- Right ventricular failure
- Total form.
As the disease progresses, isolated variants lead to the formation of a general, total form of the lesion. Damage to the left ventricle causes disturbances in the systemic circulation. Pathology of the right ventricle - affects the lungs or pulmonary circulation.
Chronic heart failure. Pathogenesis.
The consequence and manifestation of HF is a decrease or increase in blood supply, blood flow and/or pressure in certain central and peripheral parts of the blood circulation. These changes arise not only as a direct mechanical consequence of a violation of the pumping function of the heart, but also as a result of inadequacy of adaptive reactions. Such reactions include tachy- and bradycardia, changes in vascular peripheral and pulmonary resistance, “centralization” of blood circulation and other forms of redistribution of blood supply, fluid and sodium retention, hypertrophy and expansion of individual chambers of the heart, etc.
Hemodynamic disorders, in turn, lead to pathological changes both in the heart and blood vessels, and in other organs and systems and are accompanied by disorders that limit the patient’s vital activity and, ultimately, threaten his life.
Symptoms of circulatory failure and their course are different for different forms and stages of heart failure.
Degrees of chronic pathology
There are several degrees of chronic heart failure. The earlier a problem is identified, the easier it is to treat. In the later stages of the disease, mortality is 50%.
The first stage of chronic insufficiency is characterized by shortness of breath and rapid fatigue after active physical work or sports. Treatment at this time is most effective. Early detection of symptoms of chronic deficiency will not only help to cope with it, but also to determine the true cause.
In the second stage of heart failure, symptoms become more pronounced:
- cyanosis, or blue discoloration of the fingertips, nose and nasolabial folds, lips. The reason is a change in blood composition, insufficient oxygen content.
- With low-intensity loads, typical symptoms appear: shortness of breath, rapid heartbeat, weakness.
- Dry cough not associated with a cold.
The second stage is characterized by damage to the pulmonary circulation, the lungs suffer, so a cough occurs, and the blood is poorly saturated with oxygen.
Another variant of the manifestation of the second stage is damage to the systemic circulation. First of all, swelling appears. They can be hidden: fluid accumulates in body cavities, for example, filling the abdominal cavity. Swelling of the legs is more noticeable. This condition is called dropsy.
In addition, stagnation begins in all organs: liver, kidneys, digestive system, brain. Associated pathologies develop and the functioning of these organs is disrupted.
At the third stage, irreversible changes occur. Usually the functioning of the entire circulatory system is disrupted. Lesion of the small circle is characterized by a strong cough with sputum production, the appearance of pink foam not only when coughing, but also at rest. This is explained by a violation of the permeability of numerous vessels, lymphatic fluid fills the lungs, and edema occurs. The condition is fatal and requires urgent hospitalization. Shortness of breath accompanies a person at rest. Worsens when lying down. Periodically there are attacks of suffocation, accompanied by fear of death. They force the patient into a sitting position with his legs down.
At the same time, all vital organs suffer. Signs of congestive liver damage:
- increase in organ volume;
- formation of sclerotic and connective tissue;
- cirrhosis of the liver.
Congestive kidney damage leads to chronic renal failure. At the same time, the amount of urine excreted decreases, swelling increases and no longer goes away under the influence of medications. Intestinal dysfunction occurs, constipation or diarrhea is possible.
The third stage is irreversible. A person completely loses the ability to be active. Even household chores become beyond his power. Usually the patient is assigned a certain form of disability. The survival rate in this case is 50%. Medicine in this case can only offer supportive therapy.
Important! The third stage of the formation of congestive heart failure occurs as a result of the lack of treatment for the disease. If you consult a doctor in a timely manner in the early stages, you can not only stop the progression of the disease, but also be completely cured.
If you notice the following signs of heart failure, you should immediately contact a cardiologist:
- Shortness of breath with minor physical exertion;
- Blueness of fingers, lips, nose;
- Unreasonable dry cough, sometimes accompanied by sputum production;
- Pain in the chest, under the shoulder blade;
- Swelling of the legs, enlargement of the abdomen, which may be hidden edema.
Mild heart failure responds well to treatment, so a preventive examination by a therapist and cardiologist and the necessary diagnostic methods will help avoid serious consequences.
Chronic heart failure (CHF) is a disease in which the heart is unable to pump enough blood to supply the body with oxygen. It can occur as a result of many diseases of the cardiovascular system, among which the most common are coronary heart disease, hypertension, rheumatoid heart defects, and endocarditis. A weakened heart muscle is unable to pump blood, releasing less and less of it into the vessels.
Heart failure develops slowly and in the initial stages appears only during physical activity. Characteristic symptoms at rest indicate a severe stage of the disease. As CHF progresses, it significantly worsens the patient’s condition, leading to decreased performance and disability. The result can be chronic liver and kidney failure, blood clots, and strokes.
Timely diagnosis and treatment can slow down the development of the disease and prevent dangerous complications. An important role in stabilizing the condition is given to a correct lifestyle: weight loss, low-salt diet, limiting physical and emotional stress.
Synonyms Russian
Congestive heart failure, heart failure.
English synonyms
Heart failure, congestive heart failure.
Symptoms
Clinical manifestations of heart failure depend on its duration and severity and are quite varied. The development of the disease is slow and takes several years. If left untreated, the patient's condition may worsen.
The main symptoms of chronic heart failure include:
- shortness of breath during physical exertion, when moving to a horizontal position, and then at rest;
- dizziness, fatigue and weakness;
- lack of appetite and nausea;
- swelling of the legs;
- accumulation of fluid in the abdominal cavity (ascites);
- weight gain due to edema;
- fast or irregular heartbeat;
- dry cough with pinkish sputum;
- decreased attention and intelligence.
General information about the disease
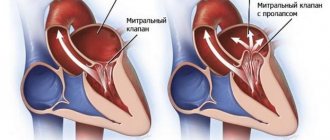
By contracting, the heart ensures continuous circulation of blood through the vessels. Together with the blood, oxygen and nutrients are supplied to all organs and tissues, and the end products of metabolism, including fluid, are removed. This is achieved by alternating two phases: contraction of the heart muscle (called systole) and its relaxation (diastole). Depending on which phase of cardiac activity disrupts its functioning, we speak of systolic or diastolic heart failure.
- Systolic heart failure is a consequence of weakness of the heart muscle and is characterized by insufficient ejection of blood from the chambers of the heart. Its most common causes are coronary heart disease and dilated myocardiopathy. More often observed in men.
- Diastolic heart failure occurs when the heart muscle loses its ability to stretch. As a result, much less blood enters the atria. The most common causes: arterial hypertension, hypertrophic myocardiopathy and stenotic pericarditis.
The human heart can be roughly divided into right and left halves. Pumping blood into the lungs and saturating it with oxygen is ensured by the work of the right parts of the heart, and the left ones are responsible for delivering blood to the tissues. Depending on which departments fail to cope with their task, they speak of right ventricular or left ventricular heart failure. When the functioning of the left sections is impaired, shortness of breath and cough come to the fore. Right-sided failure manifests itself as systemic edema.
To select the necessary medications, it is very important to determine the mechanism of heart failure and its type.
Who is at risk?
The presence of at least one of the following risk factors is sufficient for the development of chronic heart failure. The combination of two or more factors significantly increases the likelihood of disease.
Patients at risk include:
- high blood pressure;
- coronary heart disease;
- myocardial infarction in the past;
- heart rhythm disturbances;
- diabetes mellitus;
- congenital heart defect;
- frequent viral diseases throughout life;
- chronic renal failure;
- alcohol addiction.
Diagnostics
The diagnosis of chronic heart failure is made based on the medical history, characteristic symptoms and results of laboratory and other tests.
Laboratory research
- There are most often no changes in the general blood test. In some cases, moderate anemia may be detected.
- The erythrocyte sedimentation rate (ESR) may be elevated, especially when heart failure is the result of rheumatic heart disease or infective endocarditis.
- A general urinalysis is important to diagnose renal complications and exclude the renal origin of edema. One of the possible manifestations of chronic heart failure is high levels of protein in the urine.
- Total protein and protein fractions in the blood may be reduced due to their redistribution into the edematous fluid.
- Blood glucose. Important for excluding diabetes mellitus as a risk factor for heart failure.
- Cholesterol, high and low density lipoproteins. There is a clear relationship between elevated cholesterol levels and the development of atherosclerosis, coronary heart disease, and hypertension. High levels of cholesterol and lipoproteins in heart failure may indicate a more severe course of the disease.
- Sodium and potassium in the blood. In chronic heart failure, their level in the blood serum can change significantly due to edema. Monitoring blood composition is especially important when prescribing diuretics.
- Brain natriuretic propeptide (NT-proBNP) is a protein produced in the heart muscle in response to excessive stretching and overload. It circulates in the blood for quite a long time and can be easily determined during laboratory testing. The stronger the cardiac overload, the more active its secretion, therefore, an increase in the level of brain natriuretic propeptide in the blood reflects the severity of heart failure and helps to predict the disease. In addition, the higher the NT-proBNP level, the more severe the cardiac dysfunction. That is why this analysis is considered the “gold standard” in the diagnosis of chronic heart failure.
Additional Research
The scope of additional examination is determined by the attending physician.
- Chest X-ray. X-ray images allow you to assess the position and size of the heart, exclude or confirm concomitant changes in the lungs.
- Electrocardiography (ECG). Shows heart rhythm disturbances, as well as the consequences of a myocardial infarction.
- An echocardiogram allows you to differentiate systolic and diastolic heart failure, see the work of all parts of the heart, evaluate its size, muscle thickness, and examine the valves. The most important parameter is the ejection fraction. It reflects the efficiency of the heart and is expressed as the percentage of blood volume entering the aorta during contraction and remaining in it. Normally, this figure corresponds to 60-70%; in case of heart failure, it can decrease to 40%. The lower the ejection fraction, the more severe the degree of cardiac dysfunction. An indicator below 35% indicates a high risk of rhythm disturbances.
- Load tests. Designed to study the heart's response to increased physical activity.
- Coronary angiography. An X-ray examination in which a special contrast agent is injected through a catheter directly into the vessels of the heart. Helps establish the diagnosis of coronary artery disease.
Treatment
Heart failure is a chronic disease in which patients require constant medication. Properly selected therapy can slow down the progression of the process, and most often improve the condition. In some cases, surgical treatment is required.
An effective treatment method is the placement of pacemakers, or artificial heart rate regulators.
In the treatment of chronic heart failure, lifestyle also matters:
- complete cessation of alcohol and smoking,
- weight control,
- following a salt-free diet rich in protein and vitamins
- walks in the open air.
Prevention
- Lifestyle that prevents coronary heart disease:
- blood pressure control,
- regular physical activity,
- hardening procedures,
- normalization of metabolism (loss of excess weight, control of cholesterol levels, limited salt intake),
- quitting smoking, alcohol, coffee.
Clear and consistent implementation of the cardiologist’s recommendations can significantly slow down the pathological process and improve the patient’s quality of life.
Recommended tests
- Erythrocyte sedimentation rate (ESR)
- General blood analysis
- General urine analysis with microscopy
- Total protein in urine
- Serum albumin
- Total protein in whey
- Protein fractions in whey
- Total bilirubin
- Serum creatinine
- Urea in serum
- Rheumatoid factor
- C-reactive protein, quantitative (highly sensitive method)
- Potassium, sodium, chlorine in serum
- Serum calcium
- Serum magnesium
- NT-proBNP (quantitative)
The mechanism of pathology formation
Chronic cardiovascular failure develops slowly due to the body's compensatory mechanisms.
At the compensatory stage of the myocardium, the heart muscle begins to hypertrophy. The vessels expand, causing their walls to become more fragile and permeable over time. Hormones are produced that change the composition of the blood, which becomes more liquid, its volume increases due to increased work of the bone marrow and an increase in the amount of water due to retention.
Compensatory possibilities dry up, and the decompensatory stage begins, which is characterized by a weakening of the functions of the entire cardiovascular system.
As the muscle mass of the myocardium grows, its small vessels lag behind in development, as a result, the heart muscle lacks oxygen and nutrients. Pathological changes occur: the proliferation of connective and sclerotic tissue. The heart becomes unable to pump the increasing volume of blood. Extensive oxygen starvation begins, which covers all organs.
Along with this, the walls of blood vessels become more fragile and permeable. Lymph leaks from the vessels. Swelling begins. These phenomena are especially dangerous in the lungs. They quickly fill with liquid and stretch. A person is tormented by a severe cough, and the discharge of sputum does not provide relief.
Methods of treating the disease
The main goal of treating patients is to eliminate the factors that cause heart failure. Among them are rheumatism, ischemia, hypertension, etc. In some cases, surgery is required, this happens with heart defects, aneurysm, and other problems that cause a mechanical barrier to the functioning of the organ.
If the patient has severe or acute cardiovascular failure, the specialist prescribes him to adhere to bed rest. In addition, complete rest is recommended for him. If the condition is not so serious, the load may be moderate and will not affect your well-being.
It is not advisable for the patient to consume more than 600 ml of liquid per day; salt should be either completely excluded from the diet or limited to 1-2 grams. Food should be easily digestible, with plenty of vitamins.
Pharmacotherapy brings good results; it makes it possible to significantly improve the condition of patients and improve their quality of life. Treatment of heart failure involves taking several groups of medications:
- Cardiac glycosides. They are needed to improve myocardial contractility. As a result, its pumping function and diuresis increase. The products help to tolerate physical activity normally. Among the drugs are strophanthin, digoxin, etc.
- ACE inhibitors, vasodilators. Their effect is a decrease in vascular tone. The drugs cause the blood vessels to dilate. Thus, as the heart contracts, its resistance decreases, therefore, cardiac output becomes greater.
- Nitrates. The purpose of the funds is to improve the filling of blood in the ventricles. Their use allows you to increase cardiac output and make the coronary arteries wider. Among them are sustak, nitroglycerin, etc.
- Diuretics. Prevents the retention of excess water in the body. This is furosemide, etc.
- Beta blockers. Their use leads to a decrease in heartbeats, improvement in its filling with blood, and an increase in cardiac output.
- Anticoagulants. Prevents the formation of blood clots in blood vessels. This is, in particular, aspirin.
- Means leading to improvement of myocardial metabolism. These are vitamins B, C, riboxin.
If a patient develops pulmonary edema, he should be admitted to a hospital where he will receive emergency treatment. He will need to take diuretics and nitrates. The patient is given drugs that increase cardiac output. In addition, he is prescribed oxygen inhalations.
When water accumulates in the abdominal cavity, it is removed using punctures. If pneumothorax occurs, pleural puncture is necessary. If a patient has a low oxygen content in the tissues, oxygen therapy is recommended. That is, if there is heart failure with symptoms, treatment - tablets, other drugs - should be prescribed by a specialist.
Causes of the disease
The causes of congestive heart failure are pathologies of the cardiovascular and endocrine systems. They can be congenital or acquired:
- genetic predisposition;
- ischemic disease.
- myocarditis
- diseases resulting in thickening of the walls of the myocardium and pericardium;
- thyroid diseases;
- diabetes.
Factors that provoke the occurrence of pathological processes include:
- bad habits, smoking and alcoholism;
- sedentary lifestyle;
- excessive body weight;
- severe infections (usually viral);
- heavy physical activity;
- frequent stress, improper daily routine, lack of sleep.
Congestive heart failure is more common in old age, occurring in 10% of people after sixty years of age. However, the disease also affects young people. In adolescence, it is necessary to carefully monitor the state of the cardiovascular system. The rapid growth of bone and muscle tissue, hormonal changes increase the load on the heart, which does not have time to grow with such rapid growth of the body as a whole.
Young athletes are at risk. Typically, training for teenagers is more gentle; children undergo annual examinations. If signs of congestive heart failure are detected, not only urgent treatment is necessary, but also a temporary refusal to exercise. Doctors recommend taking a break for about a year.
Preventive measures
For preventive purposes, to prevent the occurrence of such a disease, it is necessary to prevent the development of diseases that lead to it. Among them is ischemia, hypertension, heart defects. In addition, it is necessary to prevent as much as possible the emergence of factors that favor the appearance.
If you have heart failure, the symptoms of which have already appeared, you must first of all try to prevent its progression. To do this, you should not exceed the recommended physical activity, take all medications prescribed by your doctor, and be regularly examined by a cardiologist. The doctors of the Clinical Hospital “RZD-Medicine” in Nizhny Novgorod will help you monitor your health.
Acute form
Along with chronic, there is an acute form of heart failure. The reasons for its occurrence are:
- myocardial infarction;
- major stroke;
- structural defects of the heart, congenital and acquired;
- hypertension.
A distinctive feature of acute cardiovascular failure is the suddenness of the attack and the absence of the listed stages of development. The person's condition quickly deteriorates and death is possible within a few minutes. The occurrence of pathology is indicated by a sharp deterioration in condition, suffocation, severe cough with foam or red sputum, blue discoloration of the skin, and cold sweat.
In such cases, first aid is to call an ambulance. Then the victim should be taken out into the open air, the collar and other tight clothing should be unbuttoned. The best pose is considered to be sitting, with legs down. A nitroglycerin tablet should be given under the tongue. Repeat the dose every 10 minutes until the ambulance arrives.
Important! In acute heart failure, you should not take a supine position.
Types of vascular insufficiency
Based on localization, vascular insufficiency can be divided into: regional (affecting a specific part of the body) and systemic (affecting the vessels of the whole body).
According to the speed of formation and progression, acute and chronic vascular insufficiency are distinguished.
- Acute failure develops when there is a sharp drop in the level of pressure in the vessels, for example, with cardiogenic shock due to myocardial infarction. Characterized by the development of collapse due to a pronounced drop in blood pressure.
- Chronic failure develops over time when blood pressure drops below 100/60 mmHg. This concept includes a wide group of diseases: thrombophlebitis, vertebrobasilar insufficiency, coronary heart disease, mesenteric vascular insufficiency and other conditions accompanied by ischemia. Chronic vascular insufficiency can be primary (develops when the activity of the autonomic nervous system is disrupted) and secondary (due to various diseases).
Age and gender factor
Statistical studies prove the connection between the spread of the disease and the gender and age of the patient.
In the age group up to 65 years, women suffer from congestive heart failure to a lesser extent; above this age, the rates become equal. Death as a result of acute heart failure is recorded in men after 45 years.
In old age, symptoms of congestive heart failure are more common, this is explained by chronic diseases, poor lifestyle, and reduced immunity.
Diagnostics
Symptoms of congestive heart failure are observed by the therapist when examining the patient and listening to heart sounds. He refers the patient to a cardiologist. A number of studies are being carried out:
- ECG;
- ECHOCG
- HMEKG
- Radiography
- Coronary angiography
- MRI, MSCT
Research is being conducted on the characteristics of the heartbeat during physical activity. To do this, the patient is asked to perform a series of simple exercises, such as squats. After this, monitor the change and restoration of the pulse. More in-depth examinations of this kind are performed using a treadmill or exercise bike.
What awaits patients
Half of all patients diagnosed with heart failure live more than five years. It is difficult to talk about maximum life expectancy; this indicator is determined by many factors. These include the severity of the disease, concomitant background, and the effectiveness of the prescribed treatment. The kind of life the patient leads and much more is of great importance.
If the disease is detected in the initial stage, with the help of therapy the patient’s condition can be completely compensated. At stage 3 of the disease, experts talk about a worse prognosis.