Hypotrophy in a child
Whatever the cause of malnutrition, this disease is always associated with partial starvation. If measures are not taken to stop malnutrition, pathophysiological changes progress. In severe forms of the disease, the body becomes unable to maintain and regulate physiological constants: clearances decrease, blood circulation slows down, and basal metabolism decreases.
In children diagnosed with hypotrophy, the body overheats and cools down excessively due to disruption of the functioning of many systems in the body. In children with the diagnosis in question, susceptibility to hypothermia is recorded. At normal temperatures, the body of a healthy child maintains a standard temperature, and a child with malnutrition cools down in just a few hours.
Children with malnutrition quickly cool down due to increased heat transfer (the ratio of body surface to weight increases, the fat layer disappears) and due to insufficient chemical thermoregulation. Exposure to hypoglycemia is also dangerous for the baby's life. Even 2-3 hours of fasting can lead to severe hypoglycemia.
But the ability to tolerate hypoglycemia in children with malnutrition is very high. Signs of severe hypoglycemia appear only when blood sugar levels become very low. The peculiarity of hypoglycemia during malnutrition is the rarity of seizures.
Before the attack there is pallor, sometimes nystagmus. Then breathing stops for 20-40 seconds and the pulse slows down. After apnea, the child takes 2-4 convulsive breaths. If help is not provided, the child will die due to paralysis of the respiratory muscles. In case of a seizure, a child needs to be given an injection of glucose, then the condition will quickly return to normal.
The ultimate causes of impaired physiological functions during malnutrition are not fully understood today. It is assumed that the loss of somatic stability occurs due to dysfunction of the endocrine glands. It is a well-established fact that fasting reduces the weight of the pituitary gland, thyroid gland, adrenal glands and gonads. Injection of an extract of the pituitary gland of normal animals into hypotrophic ones causes a rapid increase in the weight of those glands that are regulated by pituitary triple hormones. Therefore, it is assumed that in the preterminal phase of prolonged partial fasting a state of pseudohypophysectomy occurs.
Republican Children's Clinical Hospital
Malnutrition in children is a chronic nutritional disorder. Hypotrophy is a type of dystrophy. If dystrophy in a child occurs with a deficiency of body weight, then it is called malnutrition, but if dystrophy occurs with excess body weight, then it is paratrophy.
What could be the reasons?
Hypotrophy is distinguished between prenatal (congenital) and postnatal (acquired). Congenital malnutrition develops during a pathological course of pregnancy, various diseases of the mother, the presence of occupational hazards, smoking, drinking alcohol during pregnancy, etc.
The causes of acquired malnutrition are divided into internal and external.
Internal - caused by pathologies of the body that interfere with food intake and digestion, absorption of nutrients and metabolism: congenital malformations, central nervous system lesions, immunodeficiency, endocrine diseases, metabolic disorders.
In the group of endogenous factors, it is worth highlighting food allergies and three hereditary diseases that occur with malabsorption syndrome - one of the common causes of malnutrition in children:
- — cystic fibrosis — disruption of the exocrine glands, affecting the gastrointestinal tract and respiratory system.
- — celiac disease — gluten intolerance, changes in a child’s intestinal function begin from the moment gluten-containing foods are introduced into the diet — barley, semolina, wheat porridge, rye, oatmeal.
- - lactase deficiency - the digestibility of milk is impaired (lactase deficiency).
External - caused by incorrect actions of parents and unfavorable environment:
- nutritional factor: insufficient supply of breast milk, incorrectly selected formula for artificial feeding, late introduction of complementary foods, low amount of calories in complementary foods, imbalance in proteins, fats and carbohydrates;
- infectious factor: intestinal infections, chronic infections, frequent acute respiratory viral infections and other diseases;
- toxic factor: unfavorable environmental conditions, medication, poisoning, excessive intake of vitamins, especially A and D;
- social factor: inattention of parents to the child, lack of walks in the fresh air, lack of gymnastics and massage.
How does malnutrition manifest itself?
Hypotrophy of the first degree - characterized by thinning of the subcutaneous fat layer on the trunk, limbs, body weight deficiency compared to the norm is 10-20%. Tissue turgor is reduced. The child's height is appropriate for his age. The child does not lag behind in psychomotor development, but is characterized by unstable emotional tone and increased excitability.
Hypotrophy of the second degree - the subcutaneous fat layer is sharply thinned on the trunk, limbs, absent on the abdomen, the weight deficit compared to the norm is 20-30%. There is a delay in growth and psychomotor development. The child is restless, irritable, or has a sluggish response to his surroundings. The skin is pale, dry, “marbled”; tissue turgor is flabby, muscle tone is reduced; appetite is reduced, there may be vomiting, regurgitation, unstable stool, sometimes “hungry” - scanty, dry, discolored, with an unpleasant putrid odor, or dyspeptic.
Hypotrophy III degree. The subcutaneous fat layer is absent on the trunk and limbs, facial features are pointed. Body weight deficiency compared to the norm is more than 30%. The skin is pale gray, dry, flaky, the skin fold almost does not straighten out (the elasticity of the skin is sharply impaired). The mucous membrane of the lips is bright, dry, and there are “seals” in the corners of the mouth. Dry cornea. Hypertonicity of the muscles of the arms and legs is often observed. Shallow breathing, muffled heart sounds, arterial hypotension. The stomach is swollen. The stool is unstable with a tendency to constipation. Urination is reduced. Children are lethargic and indifferent to their surroundings. As a result of a sharp violation of immunoreactivity, complications develop (otitis media, pneumonia, pyelonephritis, meningitis), which are sluggish and asymptomatic.
What are the principles of treatment?
In a polyclinic, stage I malnutrition is treated in young children, and stage II and III malnutrition is treated inpatient settings.
The main activities are aimed at: normalizing nutrition; diet therapy (gradual increase in calorie content and volume of food consumed by the child + fractional, frequent feeding); compliance with the daily routine; organizing proper child care; correction of metabolic disorders; drug therapy (enzymes, vitamins, anabolic hormones); in the presence of a severe form of the disease, intravenous administration of glucose, protein hydrolysates, vitamins, and saline solutions is prescribed; Ural Federal District; massage with elements of exercise therapy.
With timely treatment of stage I and II disease, the prognosis is favorable, but with grade III malnutrition, up to 50% of cases are fatal!
What is prevention?
Prevention of malnutrition in children involves regular examination by a pediatrician, constant anthropometry and nutritional correction. During pregnancy, the mother must: maintain a daily routine; eat in a timely manner; promptly treat existing diseases; eliminate all possible unfavorable factors. maintain a daily routine; eat in a timely manner; promptly treat existing diseases; eliminate all possible unfavorable factors. After the birth of a child, an important role is played by: high-quality and balanced nutrition of the nursing mother; timely and correct introduction of complementary foods; body weight control; rational, competent care for a newborn; treatment of any, even spontaneously occurring, concomitant diseases.
Having heard a diagnosis such as malnutrition, parents should understand that the child needs the help of a qualified doctor, and not postpone examination and treatment for the future. If you provide your child with normal conditions of routine, care and nutrition in a timely manner, quick and effective treatment of possible infections and concomitant pathologies - severe forms can be avoided!
head Pediatric Department, pediatrician of the highest category G.D. Levchenko
Consequences of malnutrition
With timely seeking medical help and adequate therapy, the prognosis is favorable, however, if the main symptoms of the disease are ignored for a long time, the child may develop the following complications:
- impairment of mental and physical development;
- deficiency conditions (rickets, anemia, etc.);
- prolonged colds, more severe course of various inflammatory diseases (pneumonia, otitis media, enterocolitis, etc.).
With third degree malnutrition, even with treatment, the mortality rate is about 50%.
Signs
There are several stages of muscle wasting:
- The amount of subcutaneous tissue throughout the body decreases. A person loses up to 20% of body weight. He has pallor, weak appetite, muscle tone decreases;
- Subcutaneous tissue on the abdomen and chest practically disappears. The skin becomes gray, the muscles become flabby, and the liver increases in size. Mental health disorders and irritability occur;
- Severe wasting (cachexia) occurs when the patient loses 30% of muscle mass. The condition requires intensive therapy.
Common symptoms of muscle wasting include the following:
- Constant muscle pain;
- Weakness;
- Inability to perform normal movements;
- Significant loss of body weight.
If areas of muscle wasting are located symmetrically, this raises suspicion of myopathy or spinal amyotrophy. With progressive muscular dystrophy, relatively isolated wasting of the quadriceps femoris or biceps brachii is observed. If malnutrition is located in the distal limbs, we are talking about polyneuropathy (with impaired sensitivity and loss of reflexes in the distal limbs) or Steinert’s myotonic dystrophy.
Unilateral acquired isolated muscle wasting is always a consequence of damage to the root, plexus or peripheral nerve. Decisive for the topical diagnosis is the characteristic distribution of the process of malnutrition and sensory disturbances or prolonged inactivity of the muscle. Hypotrophy of the quadriceps muscle occurs with arthrosis of the knee joint and with sarcoma of the hip. Focal wasting of individual muscles or muscle groups, isolated and sometimes symmetrical, can slowly progress over many years. This is a sign of focal damage to the ganglion cells of the anterior horns or ischemia in the area of the blood supply of the artery.
Hypotrophy of the calf muscles often occurs. With progressive muscular dystrophy, sometimes in significantly hypotrophied muscles areas with intact muscle fibers are identified, which look like nodules. Doctors at the Yusupov Hospital distinguish them from a muscle roll, which is formed when the short head of the biceps brachii muscle is ruptured and is noticeable on the flexor surface of the shoulder.
Diagnosis of malnutrition
The diagnosis of malnutrition is based not only on determining the presence of underweight in a child, but also on identifying the immediate cause of the development of this pathological condition. An obligatory stage is an examination of the child by a pediatrician, as well as a conversation with the parents, during which the doctor learns all the necessary anamnestic data. After a thorough physical examination of the child and analysis of the life history and illness, additional laboratory and instrumental tests and consultations with specialized specialists (pediatric endocrinologist, gastroenterologist, etc.) are prescribed.
Laboratory diagnostics must necessarily include general clinical tests (general blood and urine tests), coprograms, biochemical blood tests with determination of glucose, total protein (as well as its fractions), liver tests and other indicators.
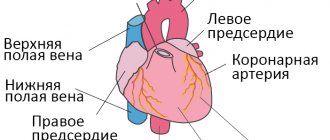
Of the instrumental diagnostic methods, ultrasound of the abdominal organs, electrocardiography (ECG), and echocardiography (ultrasound of the heart) are mandatory.
If necessary, if indicated, other studies , which help determine the underlying disease against which the malnutrition occurred.
Treatment
Neurologists at the Yusupov Hospital prescribe complex treatment to patients suffering from muscle dystrophy, aimed at eliminating the cause of the disease, influencing the mechanisms of development of the pathological process, and reducing the manifestations of the disease. To improve blood flow in peripheral vessels, angioprotectors (trental, pentoxifylline, chimes), low molecular weight dextran, and prostaglandin E preparations (vasaprostan) are used. After dilating blood vessels with no-shpa and papaverine, the supply of muscle fibers with oxygen and nutrients improves.
B vitamins (thiamine hydrochloride, pyridoxine hydrotartrate, cyanocobalamin) normalize metabolic processes and the conduction of nerve impulses. Biological stimulants stimulate the regeneration of muscle fibers and restore muscle volume: aloe, actovegin, plasmol. To restore muscle conduction, prozerin, galantamine, and armin are used.
Factors leading to development
The causes accompanying the disease can be external and internal. The first group, characterized by disorders in the body, includes:
- encephalopathy, due to which not only the functioning of the nervous system is disrupted, but also secondary changes occur in the functioning of other organs;
- pathological development of lung tissue, due to which the body does not receive the required amount of oxygen, slowing down its internal processes;
- congenital pathological changes in the functioning of the gastrointestinal tract, leading to insufficient absorption of food;
- surgical operations on the intestines, leading to its shortening;
- diseases of the immune system, leading to the inability to fight infections;
- endocrine changes (most often hypothyroidism or pituitary dwarfism);
- hereditary diseases that disrupt the absorption of certain nutrients (galactosemia, fructosemia, etc.).
The second category includes:
- insufficient nutritional value of breast milk;
- underfeeding;
- the impact of toxic factors on the body;
- frequent infectious infections.
Symptoms
Symptoms of malnutrition in a child depend on the stage of the disease.
At stage I , the doctor can determine the signs by carefully examining the small patient. Pay attention to insufficiently intense staining and decreased skin turgor, lack of fat in the abdominal area.
At stage II, disturbances in motor activity and appetite are evident. The patient's skin becomes flabby, peels, and does not straighten on its own with mild deformities. The layer of subcutaneous fat remains only on the face. Frequent deviations in the functioning of other systems, attacks of tachycardia or too low blood pressure are recorded.
At stage II , a poor reaction to external stimuli is revealed, the face also loses a layer of subcutaneous fat, and muscle atrophy is noted. Characteristic signs are retraction of the eyeballs and the fontanel area. Disturbances in stool and urination appear, and vomiting is common.
Methods of treating malnutrition
In the presence of an underlying pathology that caused the development of malnutrition, first of all, therapeutic measures are carried out aimed at treating the underlying disease.
Treatment of malnutrition is complex , step-by-step, it is based on the gradual removal of the child from this pathological condition. It is mandatory to organize a proper daily routine and nutrition for the child. The basis of treatment is diet. At the first stage, tolerance to food is established, then they gradually move on to intensive feeding (a period of increasing food loads), after which the child is completely removed from malnutrition. Children with the first degree of pathology can be treated on an outpatient basis, under the dynamic supervision of a doctor; with moderate and severe forms of pathology, the child should be hospitalized in a hospital. Daily monitoring of the patient’s body weight is mandatory, as well as keeping a food diary and hydrobalance sheet.
Drug treatment consists of prescribing enzyme preparations to improve digestion, vitamins, probiotics, and, if necessary, infusion therapy.
Treatment of this disease is a rather complex process, where many nuances must be taken into account to achieve the desired effect, so self-medication of such a child at home is unacceptable and can be extremely dangerous to his life and health.
Classification
There are three degrees of malnutrition in children, each of which is characterized by its own characteristics:
- I degree - 20% of the required body weight is missing, while growth and neuropsychic development are maintained within normal limits;
- II degree - the deficiency is 25–30% of the required indicators, the first signs of growth retardation and neuropsychic disorders appear;
- III degree - weight loss is more than 30% of normal, stunted growth and pathological changes in the neuropsychic sphere become clearly visible.
Read also: Food poisoning in a child