Arrhythmia - symptoms and treatment
First aid for an arrhythmia attack
First aid measures depend on the specific arrhythmia, and its type can only be determined by a doctor. Therefore, you should not self-medicate, you need to seek medical help.
Is it possible to cure arrhythmia?
Cardiac arrhythmias vary greatly in prognosis. Some are completely harmless, and some are dangerous. Treatment of cardiac arrhythmias is not always required. First, treatment is appropriate when arrhythmia reduces quality of life. Secondly, it makes sense to treat those arrhythmias that worsen the prognosis, that is, they can lead to premature death or other complications (and the reality of such complications must be proven in clinical studies). Accordingly, asymptomatic cardiac arrhythmias that do not lead to any sensations are not treated in most cases.
In addition, the doctor must try to establish what caused the arrhythmia, and then prove the connection between the suspected causative factor and the arrhythmia itself.
When the decision about the need to treat a particular cardiac arrhythmia is made, the question arises of how to treat it.
Surgery
For many decades, the doctor had no other treatment options for heart rhythm disorders other than medication. Rare exceptions include electrical shock therapy, which delivers a shock using an external defibrillator in a critical situation to eliminate a life-threatening arrhythmia, and transesophageal electrical stimulation of the heart to eliminate some supraventricular tachyarrhythmias.
Since the 90s of the last century, and in Russia since the 2000s, a new treatment method has appeared that is effective for many cardiac arrhythmias - radiofrequency ablation (RFA). The method allows in many cases to permanently relieve the patient of the need to take medications to treat arrhythmias. The essence of the method is a local radiofrequency effect on the source of arrhythmia or on the pathological path of electrical impulse circulation in the heart. The procedure is carried out using a catheter passed to a specific area in the heart through a puncture in a vessel (usually in the thigh). Due to the effect through the tip of the catheter, local heating of the heart muscle area occurs up to 70 °C. As a result, in this place there is a local death of cells involved in the unwanted generation of impulses or in their unwanted conduction. Thus, the conditions for the occurrence and maintenance of certain cardiac arrhythmias, for example, ventricular tachycardia, disappear.
Almost all supraventricular tachyarrhythmias can be treated with RFA: atrioventricular nodal tachycardia, tachycardias involving accessory pathways, atrial flutter, focal atrial tachycardia, and, with less success, atrial fibrillation.[9] In addition, this method treats many types of ventricular tachycardia and ventricular extrasystoles, if it is very frequent (tens of thousands of extrasystoles per day) and comes from one focus.[10]
Another high-tech treatment for potentially fatal ventricular arrhythmias is implantation of a cardioverter defibrillator.[10] This device is capable of eliminating already developed ventricular tachycardia or ventricular fibrillation in two ways: by electrical stimulation of the ventricles at a rhythm exceeding the tachycardia rhythm, or by applying a fairly powerful electrical discharge, which is quite painful, but saves lives. Thus, a cardioverter-defibrillator is used in cases where there is a real risk of sudden death due to ventricular arrhythmias.[13]
Electrocardioversion
Electrical cardioversion (defibrillation) is used when the arrhythmia sharply worsens the patient's condition and is accompanied by a significant drop in blood pressure. It is also sometimes performed routinely to restore sinus rhythm if atrial fibrillation persists.
Pharmacotherapy
However, in many cases, cardiac arrhythmias are treated with medications. Most often, antiarrhythmic drugs are prescribed in the case of atrial fibrillation (atrial fibrillation), in which case the effectiveness of RFA is not so high. Another situation in which antiarrhythmic drugs are often used is frequent premature beats (thousands or tens of thousands of untimely heartbeats per day) accompanied by symptoms. Less commonly, the drug method is used to treat other arrhythmias - for example, ventricular tachycardia, supraventricular tachyarrhythmias.
Unfortunately, few antiarrhythmic drugs are registered in Russia compared to Europe or the USA. Available in our country are “Novocainamide” (still used for intravenous administration in the emergency treatment of paroxysms of atrial fibrillation and rarely ventricular tachycardia), “Lidocaine” (for intravenous administration for ventricular tachycardia), “Etatsizin”, “Allapinin” and “Propafenone”. " These drugs exist in the form of tablets and are prescribed for long-term use in order to prevent the occurrence of a wide range of ari in the form of tablets and solution is also used to eliminate paroxysms of atrial fibrillation - a universal antiarrhythmic drug, but is used mainly as a backup antiarrhythmic. But it can be prescribed for organic damage to the heart (previous myocardial infarction, low cardiac contractility, severe left ventricular hypertrophy, etc.), while Etatsizin, Propafenone and Allapinin cannot be used in these conditions.[11]
Sotalol is an antiarrhythmic drug to prevent attacks of atrial fibrillation, as well as ventricular arrhythmias. Available in tablets.
Another class of drugs for arrhythmia are calcium antagonists - Verapamil and Diltiazem. They are used for some supraventricular tachyarrhythmias, both for long-term use in tablets and to eliminate developed attacks of arrhythmias with a high heart rate.
Beta-blockers form an independent class of antiarrhythmic drugs, although their direct antiarrhythmic activity is low. Their main effect is their ability to reduce the risk of sudden cardiac death, mainly in people with low cardiac contractility and associated heart failure.[11] The most studied in this regard are Metoprolol succinate, Bisoprolol, Carvedilol and Nebivolol.
In the treatment of atrial fibrillation and flutter, the most important place is occupied by antithrombotic drugs, which reduce blood clotting and thereby reduce the risk of blood clots (in these cardiac arrhythmias it is increased). These are Warfarin, Dabigatran, Rivaroxaban, Apixaban, Edoxaban. Accordingly, taking these medications reduces the risk of stroke associated with thromboembolism.
Lifestyle
Some arrhythmias are provoked by stress, abuse of coffee and caffeine-containing drinks, smoking, lack of sleep, physical activity and taking certain medications. Therefore, the doctor first of all looks for a cause-and-effect relationship between lifestyle factors and the occurrence of arrhythmia. Sometimes the patient himself notices this connection. In such cases, if you eliminate the provoking factor, you can get rid of the arrhythmia. However, it is not always possible to detect such a connection.
Folk remedies
If you suspect an arrhythmia, you should consult a doctor, get diagnosed and adhere to the prescribed treatment. Traditional methods of therapy are not scientifically substantiated and can be hazardous to health. Without adequate treatment, arrhythmia can cause serious complications: angina pectoris, myocardial infarction and ischemic stroke.
How to notice the first signs of abnormal heart function
At first glance, it seems that it is impossible not to notice the development of cardiac pathology. But in reality, arrhythmia is often asymptomatic. The person continues to feel healthy, and if occasional attacks occur, he attributes them to overwork.
The pathological condition is accompanied by the following manifestations:
- changes in heart rate for no particular reason;
- chest tightness, pain;
- nausea, dizziness;
- loss of consciousness.
People experience these symptoms differently. For some, this is a reason to stay in bed, while others do not pay attention to poor health and risk their lives.
The presence of arrhythmia is easily confirmed by hardware diagnostics. If a doctor suspects a patient has this disease, he may prescribe a chest ultrasound, echocardiography, or electrocardiography.
Arrhythmia comes in different types. Modern medicine knows the following subtypes:
- atrial fibrillation (heart contractions are chaotic);
- paroxysmal tachycardia (pulse is regular, but very frequent - up to 240 beats/min);
- blockade (the pulse temporarily or completely disappears);
- extrasystole (out of sequence of contractions, which leads to an increase or fading of the rhythm);
- respiratory arrhythmia (blood pulses alternate incorrectly, this happens in adolescents or even children).
The most dangerous condition is considered to be erratic heartbeats. They are often accompanied by hoarse breathing, convulsions, and loss of consciousness.
Causes of pathology
- Alcohol abuse, smoking, drug use
- Including plenty of caffeine-containing foods and drinks in your diet
- Side effects of certain medications
- Psycho-emotional stress and hard physical labor
- Somatic diseases (coronary heart disease, consequences of myocardial infarction, arterial hypertension, diseases of the adrenal glands and thyroid gland)
- Traumatic brain injuries
- Menopause
Clinical symptoms
Clinically, various rhythm disturbances may not manifest themselves in any way, that is, the patient himself does not complain, or predictors of arrhythmia are identified during a preventive or any other examination (during ECG registration, examination by a therapist). With a clinically pronounced course, a number of symptoms can be identified:
- tachycardia (increased heart rate)
- bradycardia (slow heart rate)
- feeling of heart failure
- sensation of a foreign body, heaviness in the chest
- change in the frequency and depth of breathing movements
- general weakness
- loss of consciousness (in extremely severe clinical cases)
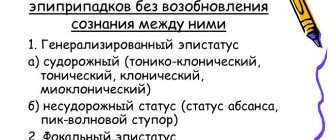
Classification
All rhythm and conduction disorders are classified as follows:
- Heart rhythm disturbances.
- Conduction disorders in the heart.
In the first case, as a rule, there is an acceleration of the heart rate and/or irregular contraction of the heart muscle. In the second, the presence of blockades of varying degrees with or without slowing of the rhythm is noted.
In general, the first group includes disorders of the formation and conduction of impulses:
- In the sinus node, manifested by sinus tachycardia, sinus bradycardia and sinus arrhythmia - tachyarrhythmia or bradyarrhythmia.
- According to the tissue of the atria, manifested by atrial extrasystole and paroxysmal atrial tachycardia.
- At the atrioventricular junction (AV node), manifested by atrioventricular extrasystole and paroxysmal tachycardia.
- Along the fibers of the ventricles of the heart, manifested by ventricular extrasystole and paroxysmal ventricular tachycardia.
- In the sinus node and along the tissue of the atria or ventricles, manifested by flutter and fibrillation (fibrillation) of the atria and ventricles.
The second group of conduction disorders includes blockades in the path of impulses, manifested by sinoatrial block, intraatrial block, atrioventricular block of 1, 2 and 3 degrees and bundle branch block.
AV block
AV block occurs when the heart partially or completely stops conducting impulses from the atria to the ventricles. Because of this, the heart rate is disrupted, and organs and tissues do not receive enough blood and oxygen.
Symptoms . When the disease develops:
- weakness, shortness of breath;
- angina pectoris – pain in the sternum;
- dizziness, darkening of the eyes;
- bradycardia - a decrease in heart rate to 30-50 beats per minute.
Diagnosis and treatment . AV block is diagnosed by ECG and echocardiography. If the problem appears due to taking certain medications (for example, papaverine or drotaverine), to eliminate it, it is enough to stop taking the medications. If there are concomitant heart diseases, beta-agonists are prescribed; in severe cases, a pacemaker is implanted.