Naphthidrine derivatives, quinolones, fluoroquinolones are a large group of synthetic drugs that have an antibacterial effect, which are characterized by the presence of a quinoline core in the molecule.
Drugs in this class are represented by two groups of substances that differ in the presence or absence of a fluorine atom in the molecule - fluorinated and non-fluorinated compounds.
Quinolones (non-fluorinated quinolones) have a narrow spectrum of action, that is, they affect a limited number of pathogens of bacterial infectious diseases and create effective antibacterial concentrations mainly in the urine. In addition, bacteria rapidly develop resistance to quinolones.
Fluoroquinolones are much more active than non-fluorinated quinolones, have a wide spectrum of antibacterial action - they affect a large number of pathogenic bacteria, and also penetrate better into various organs and tissues, creating effective antibacterial concentrations of the drug there.
Indications for use
Quinolon drugs are indicated for bacterial infections of the kidneys and urinary tract - pyelitis, pyelonephritis, cystitis, urethritis.
Fluoroquinolone preparations are used for various severe bacterial infections and infections of moderate severity: infections of the upper respiratory tract and ENT organs (sinusitis, sinusitis, sinusitis, ethmoiditis, tonsillitis, pharyngitis, otitis), lower respiratory tract infections (bronchitis, pneumonia), kidney infections and urinary tract (pyelitis, pyelonephritis, cystitis, urethritis, prostatitis), intestinal infections (typhoid fever, shigellosis), sexually transmitted infections (chlamydia, gonorrhea), infections of the skin, soft tissues, bones and joints, infectious and inflammatory diseases of the eyes (conjunctivitis, keratitis, blepharitis).
Certain fluoroquinolone preparations (lomefloxacin, ofloxacin, levofloxacin, ciprofloxacin) are also used in the complex treatment of drug-resistant tuberculosis.
Naphthidrine derivatives, quinolones
Home Medical encyclopedia Medicines Antimicrobial and antiparasitic medicines
NAPHTHIDRINE DERIVATIVES. QUINOLONES. FLUOROQUINOLONES
NALIDIXIC ACID (Acidumnalidixicum)
Synonyms: Nevigramon, Negram, Cystidix, Nagram, Nalidin, Nilidixan, Nalidixin, Naligram, Nalix, Nalurin, Naxuril, Nogram, Notricel, Specifin, Urodixin, Urogram, Uroneg, Vintomilon, etc.
Pharmachologic effect. It is a synthetic antibacterial drug. Effective against infections caused by gram-negative bacteria, intestinal, dysentery and typhoid bacilli, Proteus (a type of microorganism that, under certain conditions, can cause infectious diseases of the small intestine and stomach), Klebsiella bacillus (Friedlander - bacteria that cause pneumonia and local purulent processes). It acts bacteriostatically and bactericidally (prevents the proliferation and destroys bacteria). Effective against strains resistant to antibiotics and sulfonamides. It is ineffective against gram-positive cocci (staphylococci, streptococci, pneumococci) and pathogenic anaerobes (bacteria that can exist in the absence of oxygen and cause human diseases).
The drug is well absorbed from the gastrointestinal tract. About 80% is excreted unchanged in the urine. The half-life (the time during which 2 doses of the drug is eliminated) is approximately 8 hours, but in case of renal failure it reaches 20 hours or more.
Indications for use. It is used mainly for urinary tract infections: cystitis (inflammation of the bladder), pyelitis (inflammation of the renal pelvis), pyelonephritis (inflammation of the kidney tissue and renal pelvis) - caused by microorganisms sensitive to the drug. Most effective for acute infections. It is also prescribed for the prevention of infections during operations on the kidneys and bladder. Recommended for enterocolitis (inflammation of the small and large intestines), cholecystitis (inflammation of the gallbladder), inflammation of the middle ear and other diseases caused by microorganisms sensitive to the drug, including those resistant to other antibacterial agents.
Method of administration and dose. Adults take 0.5 g orally (1 capsule or 1 tablet), and for more severe infections - 1 g 4 times a day. The course of treatment is at least 7 days. For long-term treatment, use 0.5 g 4 times a day.
Children are prescribed at the rate of 60 mg/kg, dividing the daily dose into 4 equal parts.
Side effect. Nalidixic acid is generally well tolerated; however, nausea, vomiting, diarrhea, headache, and dizziness are possible. Allergic reactions may occur (dermatitis /skin inflammation/, increased body temperature, eosinophilia /increased number of eosinophils in the blood/), as well as increased skin sensitivity to sunlight (photodermatoses). In patients with cerebrovascular accidents, parkinsonism, and epilepsy, seizures may occur. Due to the possibility of convulsive reactions, one should beware of an overdose of the drug in children. Severe adverse reactions require temporary or complete discontinuation of the drug.
Contraindications. Impaired liver function, depression of the respiratory center. Great care is required in case of insufficient renal function. It should not be prescribed to women in the first 3 months. pregnancy and children under 2 years of age.
The drug should not be used simultaneously with nitrofurans, as this reduces the antibacterial effect.
Release form. In capsules or tablets of 0.5 g.
Storage conditions. List B. In a dry place, protected from light.
NORFLOXACIN (Norfloxacin)
Synonyms: Nolicin, Bactinor, Girablok, Negaflox, Norbactin, Norilet, Normax, Noroxin, Sophasin, Spectrama, Urobacil, Yutibid.
Pharmachologic effect. An antimicrobial drug from the quinolone group, a uroantiseptic (a drug that disinfects the urinary tract), which has a wide spectrum of action. Acts bactericidal (destroys bacteria). Norfloxacin is active against most gram-negative microorganisms: Es-cherichiacoli, Salmonellaspp., Shigellaspp., Proteusspp., Morganellamorganii, Klebsiellaspp., including Klebsiellapneumoniae; Enterobacterspp., Serratiaspp., Citrobacterspp., Yersiniaspp., Providencia, Haemophilusinfluenzae, Pseudomonasaeruginosa; as well as against microorganisms producing beta-lactamases (enzymes that destroy penicillins).
Indications for use. Acute and chronic urinary tract infections (uncomplicated and complicated) caused by pathogens sensitive to the drug.
Method of administration and dose. Before prescribing a drug to a patient, it is advisable to determine the sensitivity to it of the microflora that caused the disease in this patient. The usual dosage is 0.4 g 2 times a day. The maximum daily dose is 1.5 g. Duration of treatment is 7-14 days; If necessary, longer treatment is carried out.
For patients with impaired renal function with creatinine clearance (the rate of blood purification from the final product of nitrogen metabolism - creatinine) of more than 20 ml/min, norfloxacin is prescribed at the usual dose. When creatinine clearance is below 20 ml/min (or at a serum creatinine level of more than 5 mg/100 ml), half the usual dose of norfloxacin is prescribed 2 times a day or a full dose 1 time a day. Patients on hemodialysis (a blood purification method) are prescribed half the usual dose of the drug.
The simultaneous use of norfloxacin and antacids (reducing gastric acidity) reduces the intensity of absorption of norfloxacin. In this regard, norfloxacin should be prescribed 1-2 hours before or no less than 4 hours after taking these medications.
Side effect. Nausea, anorexia (lack of appetite), diarrhea, headache, feeling tired, drowsiness.
Contraindications. Liver failure, pregnancy, breastfeeding, hypersensitivity to quinolone drugs.
Patients with epilepsy, a history of seizures (previous), and severe renal impairment should prescribe norfloxacin with caution. It is not recommended to prescribe the drug to prepubertal children (age from 7 to 12-13 years). During treatment with the drug, patients should receive a sufficient amount of fluid (under the control of diuresis/urination/).
Release form. Tablets of 0.4 g in a package of 20 pieces.
Storage conditions. List B. In a dry place, protected from light.
OXOLINIC ACID (Acidumoxolinicum)
Synonyms: Gramurin, Dioxol, Emirenil, Nephroclar, Nevopax, Nidantin, Oxabide, Oxol, Pietil, Prodoxol, Urbid, Uribid, Urigram, Uristatic, Uritrate, Uropax, Dioxacin, etc.
Pharmachologic effect. According to the antibacterial spectrum of action, oxolinic acid is not significantly
different from nalidix. The drug is most effective against gram-negative bacteria (Proteus, Escherichia coli, Staphylococcusaureus). It is effective when microorganisms are resistant to other chemotherapeutic drugs, with the exception of quinolones, since cross-resistance is observed when using drugs in this group.
In in vitro experiments, oxolinic acid is 2-4 times more active than nalidixic acid. However, oxolinic acid is more neurotoxic (has a more pronounced damaging effect on the nervous system).
Indications for use. Oxolinic acid is used mainly for urinary tract infections: cystitis (inflammation of the bladder), pyelitis (inflammation of the renal pelvis), pyelonephritis (inflammation of the kidney tissue and renal pelvis), prostatitis (inflammation of the prostate gland), as well as to prevent infection during cystoscopy (with examination of the bladder), catheterization (insertion of a tube or tubular-shaped medical instrument) of the urinary tract.
Method of administration and dose. Prescribed orally for adults and children over 12 years old, 2 tablets (0.5 g) 3 times a day, for children from 2 to 12 years old - 1 tablet (0.25 g) 3 times a day. Take immediately after meals. The course of treatment is at least 7-10 days (up to 2-4 weeks).
Side effect. When using oxolinic acid, nausea, vomiting, diarrhea, heartburn, headache, anxiety, tachycardia (rapid heartbeat), sleep disturbance, and weakness are possible. These phenomena usually go away on their own. However, in case of individual intolerance, the drug should be stopped.
Contraindications. Contraindicated during pregnancy and breastfeeding, as well as in children under 2 years of age.
Due to the stimulating effect on the central nervous system, caution should be exercised when prescribing the drug to patients with epilepsy and other diseases of the central nervous system. Caution is needed when prescribing the drug to patients with insufficient liver and kidney function (reduce doses!), and elderly people.
Release form. Tablets of 0.25 g in a package of 50 pieces.
Storage conditions. List B. In a place protected from light.
OFLOXACIN (Ofloxacinum)
Synonyms: Tarivid, Flobocin, Mefokacin, Oflozet, Oxoldin, Tabrin, Vizeren, Zanotsin, Quiroll, Sanflux.
Pharmachologic effect. Like other fluoroquinolones, ofloxacin has a broad antibacterial spectrum of action. Affects mainly gram-negative bacteria. Effective against microorganisms resistant to most antibiotics and sulfonamides. Has a bactericidal (bacteria-destroying) effect.
Effective when taken orally. It is quickly and almost completely (over 95%) absorbed from the gastrointestinal tract and enters in high concentrations into organs and tissues, as well as into sputum, saliva, bile, skin, tissue and prostate secretions. Peak plasma concentrations are observed after 30-60 minutes; half-life (time during which 2 doses of the drug are eliminated) is about 6-7 hours. The drug is practically not metabolized (does not change); 75-90% is excreted in the urine, and even after a single dose the drug is detected in the urine within 20-24 hours.
Indications for use. Ofloxacin is used for infections of the respiratory tract, ear, throat, nose, skin, soft tissues, osteomyelitis (inflammation of the bone marrow
and adjacent bone tissue), infectious diseases of the abdominal organs, kidneys, urinary tract, prostatitis (inflammation of the prostate gland), infectious gynecological diseases, gonorrhea.
There is evidence of the activity of ofloxacin against Mycobacterium tuberculosis and the advisability of its use in the complex therapy of tuberculosis.
Method of administration and dose. Prescribed orally for adults. For infections of the respiratory tract, skin and soft tissues: wounds, boils (purulent inflammation of the hair follicle of the skin, spreading to surrounding tissues), carbuncles (acute diffuse purulent-necrotic inflammation of several nearby sebaceous glands and hair follicles), phlegmon (acute, not clearly limited purulent inflammation), etc.; infectious diseases of the abdominal cavity, upper urinary tract - 0.2 g (1 tablet) 2 times a day; for infections of bones and joints - 0.2-0.4 g (1-2 tablets) 2 times a day; for urethritis (inflammation of the urethra) and prostatitis (inflammation of the prostate gland) - 0.3-0.4 g 2 times a day.
For severe respiratory tract infections and other severe infections, the dose is increased to 0.3-0.4 g per day.
Take ofloxacin tablets without chewing, with a small amount of water, before or after meals.
Treatment, as with the use of other chemotherapy drugs, is carried out until the signs of the disease disappear and for the next 2-3 days or more. Usually the course of treatment is 7-10 days. In uncomplicated cases, the course of treatment may be shorter. Do not take the drug for more than 4 weeks.
Side effect. The drug is usually well tolerated. In some cases, allergic reactions (itching, rash) are observed; possible development of swelling of the face and vocal cords; anorexia (lack of appetite), abdominal pain, nausea, vomiting, diarrhea; sleep disturbances, headache, anxiety, general depression; changes in the blood picture: leukopenia (decrease in the level of leukocytes in the blood), agranulocytosis (sharp decrease in the number of granulocytes in the blood), thrombocytopenia (decrease in the number of platelets in the blood). In rare cases, the perception of smell and taste is impaired. When using ofloxacin, as well as other fluoroquinolones, you should not be exposed to ultraviolet rays due to possible photosensitization (increased sensitivity to sunlight) of the skin.
Contraindications. Hypersensitivity to quinolones, epilepsy. The drug should not be prescribed to pregnant, lactating women, children and adolescents with incomplete skeletal formation (under 15 years of age). In case of impaired renal function, the usual doses are first given, and then they are reduced taking into account creatinine clearance (the rate of blood purification from the final product of nitrogen metabolism - creatinine).
Ofloxation should not be taken simultaneously with antidepressants (that reduce stomach acidity) (including alkaline waters) to avoid a decrease in effectiveness.
Release form. Tablets of 0.2 g in a package of 10 pieces.
Storage conditions. List B. In a dry place, protected from light.
PEFLOXACIN (Pefloxacinum)
Synonyms: Abaktal, Peflacin, Pepocin, Perti, Peflobid, Pinaflox.
Pharmachologic effect. The drug has a wide antibacterial spectrum of action. Mainly affects gram-negative bacteria, but gram-negative anaerobic (capable of existing in the absence of oxygen) bacteria are resistant
to his action. The drug is effective when administered orally (by mouth) and parenterally (bypassing the digestive tract). When taken orally, it is quickly absorbed, the maximum concentration in the blood is observed 90 minutes after administration. The half-life is about 8 hours. The drug penetrates well into organs and tissues, including the brain, bones, mucous membranes, etc. It is excreted mainly by the kidneys in unchanged form, partially in the form of metabolites (metabolic products).
Indications for use. Pefloxacin is used for infections of the respiratory tract, ear, throat, nose, skin, infectious diseases of the kidneys, urinary tract, abdominal organs, infectious gynecological diseases, osteomyelitis (inflammation of the bone marrow and adjacent bone tissue) and other infections caused by bacteria sensitive to the drug.
Method of administration and dose. Adults are prescribed 1 tablet (0.4 g) orally 2 times a day (morning and evening) with meals.
The duration of treatment is usually 7-14 days. Parenterally (slow intravenous infusion) administer 400 mg (contents of 1 ampoule with a capacity of 5 ml), diluted in 250 ml of 5% glucose solution. This dose is administered over 1 hour 2 times a day (morning and evening). Do not dilute the drug with sodium chloride solution or other solvent containing chlorine ions.
In case of particularly severe disease, you can start with the administration of 800 mg (2 ampoules) of the drug.
Side effects and contraindications are the same as for other 6-fluoroquinolones (see Ofloxacin.
Release form. Tablets 0.4 g; in ampoules of 5 ml containing 0.4 g of pefloxacin (as mesylate dihydrate).
Storage conditions. List B. In a dry room.
PIPEMIDIC ACID (Pipemidicacidum)
Synonyms: Palin, Alipem, Balurol, Histomid, Filtrax, Naril, Pimidel, Pipefort, Pipram, Pipurin, Pimadel, Pipem, Septidron, Solupemide, Uripan, Urizan, Urixin, Urodipin, Uromidin, Uropimid, Urosetik, Urotractin, Uroval, etc.
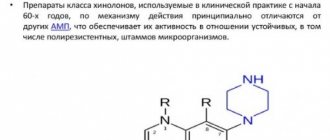
Pharmachologic effect. The drug has antibacterial activity. It is active against Pseudomonas, which is associated with the presence of a piperazine core in the molecule.
Indications for use. In clinical practice, pipemidic acid is especially effective for acute and chronic urinary tract infections.
Method of administration and dose. Adults take 0.04 g orally (1 tablet 0.4 g or 2 capsules 0.2 g) 2 times a day (morning and evening). The course of treatment is 10 days or more, depending on the course of the disease.
Children from 1 year to 15 years are prescribed at a rate of 15 mg/kg, divided into 2 doses.
For women with relapses (reappearance of signs of the disease) of infection, it is recommended that, simultaneously with oral administration, 1 vaginal suppository is prescribed daily for 7-10 days.
Children taking the drug should be under close medical supervision. During treatment, it is recommended to maintain increased diuresis (urination) - drinking plenty of fluids.
Side effect. When using the drug, allergic skin reactions, nausea, pain in the stomach are possible; the phenomenon of photosensitivity (increased sensitivity of the body to sunlight).
Contraindications. Contraindicated during pregnancy. Caution should be exercised in case of renal failure.
Release forms. In capsules 0.1; 0.2 g and 0.4 g; tablets 0.4 g; vaginal suppositories 0.2 g; suspension (for children) in 100 ml bottles containing 100 mg (0.1 g) per 5 ml.
Storage conditions. List B. In a place shielded from light.
CIPROFLOXACIN (Ciprofloxacinum)
Synonyms: Quintor, Cipro, Ciprobay, Arflox, Ciplox, Tsiprinol, Ciprobid, Ciproran, Ciproxin, Ciprova, Ciprolak, Ciprolet, Cipromid, Cipropan, Ciprosan, Afenoxime, Medociprin, Tsifobak, Ciprocinal, Citeral, Cifran, etc.
Pharmachologic effect. According to the antibacterial spectrum of action, ciprofloxacin is generally similar to other fluoroquinolones, but it has relatively high activity; approximately 3-8 times more active than norfloxacin.
The drug is effective when administered orally and parenterally (bypassing the digestive tract). When taken orally, especially on an empty stomach, it is well absorbed. Peak plasma concentrations are observed 1-2 hours after oral administration and 30 minutes after intravenous administration. The half-life (the time during which one-half of the dose of the administered drug is eliminated from the body) is about 4 hours. It is little bound by plasma proteins. Penetrates well into organs and tissues, passes through the blood-brain barrier (barrier between blood and brain tissue). About 40% is excreted unchanged in urine within 24 hours.
Indications for use. Indications for use are basically the same as for ofloxacin, pefloxacin and other fluoroquinolones (infections of the respiratory tract, skin and soft tissues, bones and joints, gastrointestinal tract, including infections caused by salmonella, shigella, campylobacter and other pathogens ; gonococcal infections, meningitis/inflammation of the meninges/, postoperative infectious complications, sepsis/blood poisoning by microbes from the focus of purulent inflammation/ and other purulent-inflammatory processes).
The drug is highly effective against urinary tract infections; when taken orally, it quickly penetrates the kidneys, is released for a long time, and has a bactericidal (bacteria-destroying) effect on Pseudomonasaeruginosa (the dominant pathogenic pathogen in complicated urinary tract infections).
The drug is indicated for the treatment of infections in cancer patients.
Method of administration and dose. Ciprofloxacin is prescribed to adults orally for uncomplicated urinary tract infections at 0.125-0.5 g 2 times a day, for complicated urinary tract infections and respiratory tract infections - 0.25-0.5 g 2 times a day; in more severe cases - up to 0.75 g 2 times a day (if parenteral treatment is not carried out). The course of treatment is usually 5-15 days.
In case of particularly severe infectious diseases and the impossibility of taking tablets orally, they begin with intravenous administration of the drug, preferably in the form of a short-term infusion (about 30 minutes). The prepared solution (in bottles) can be administered without dilution or diluted in an isotonic sodium chloride solution or 5% glucose solution. The infusion solution concentrate (in ampoules of 10 ml of 1% solution) must be diluted before administration.
For acute gonorrhea and uncomplicated cystitis (inflammation of the bladder) in women, ciprofloxacin is prescribed orally in a single dose of 0.25 g and intravenously in a dose of 0.1 g.
Doses for intravenous administration for uncomplicated urinary tract infections: 0.1 g 2 times a day, in
in other cases - 0.2 g 2 times a day. If the patient's condition improves, they switch to taking the drug orally.
Side effects and contraindications are the same as for ofloxacin.
Like other drugs in this group, shrofloxacin should not be prescribed to children and adolescents with incomplete skeletal formation (under 15 years of age).
Elderly people are given smaller doses (depending on the severity of the disease).
Release form. Film-coated tablets, 0.25; 0.5 and 0.75 g; 0.2% solution in infusion bottles of 50 and 100 ml (100 or 200 mg); 1% solution in ampoules of 10 ml (concentrate to be diluted).
Storage conditions. List B. In a place protected from light.
| print version | This information is not a guide to self-treatment. A doctor's consultation is required. |
Side effects of fluoroquinolones
Undesirable effects of fluoroquinolones (class effects):
- inhibition of the development of cartilage tissue in immature animals, therefore contraindicated for pregnant and nursing mothers; can be used in children only for special indications;
- in rare cases, it is possible to develop tendonitis (inflammation of the tendons, especially Achilles), which can lead to ruptures during physical activity;
- prolongation of the QT interval on the electrocardiogram, which can provoke the development of ventricular arrhythmias;
- photodermatitis.
Classification and generations of antibiotics from the group of fluoroquinolones
There are 4 generations of fluoroquinolone antibiotics.
First generation - non-fluoridated
- Nalidixic acid.
- Oxolinic acid.
- Pipemidic acid.
Second generation - “gram-negative”
- Ciprofloxacin.
- Norfloxacin.
- Ofloxacin.
- Pefloxacin.
- Lomefloxacin.
Third generation - “respiratory”
- Sparfloxacin.
- Levofloxacin.
Fourth generation – “respiratory” + “antianaerobic”
- Moxifloxacin.
Contraindications and special conditions
Absolute contraindications for treatment with fluoroquinolones are pregnancy and lactation. The limitation is due to pharmacokinetic properties - the active ingredients cross the placenta and enter breast milk, contributing to the development of neurotoxic effects in the fetus or newborn child. Any quinolone drug is also contraindicated for children under 18 years of age (prescribed only for complicated pathology, in the absence of an alternative therapeutic plan).
The reason for refusing to prescribe such drugs is hypersensitivity or individual intolerance to the components. There are other contraindications for prescribing these medications:
- organic disorders of the central nervous system (with cerebrovascular accidents);
- Parkinson's disease;
- convulsive syndrome;
- epilepsy;
- liver failure.
Patients with renal failure require dose adjustment. In case of glucose-6-phosphate dehydrogenase deficiency, it is necessary to assess the risk and expected benefit of introducing such drugs into the therapeutic plan.
Side effects
Like all antimicrobial agents, fluoroquinolones exhibit several multidirectional negative reactions. There are several known side effects, especially pronounced with long-term use or non-compliance with the recommended dosage:
- allergic reactions (urticaria, Quincke's edema);
- dyspeptic disorders (nausea, vomiting, diarrhea, flatulence);
- headaches and abdominal pain;
- convulsions;
- cytopenia;
- development of neurotoxic processes;
- hemolytic anemia;
- slowing of cardiac conduction (development of arrhythmia).
With long-term use, blood pressure control is necessary in patients with arterial hypertension, since derivatives can increase blood pressure. Fluoroquinolones cause increased sensitivity to light (photosensitivity). Since the constituent components increase sensitivity to the UV spectrum, patients with porphyria develop a porphyrinogenic effect.
Drug interactions of fluoroquinolones with other drugs
- The absorption of fluoroquinolones in the gastrointestinal tract sharply worsens when taking antacids, sucralfate, and drugs containing cations Ca, Mg, Al, Fe, Zn.
- Fluoroquinolones (especially ciprofloxacin, norfloxacin and pefloxacin) may inhibit the metabolism of theophylline in the liver and increase its concentration in the blood.
- When combined with nonsteroidal anti-inflammatory drugs, the risk of neurotoxicity increases, including the development of seizures.
General characteristics of fluoroquinolones
Drugs of the second group have a number of significant advantages over first-generation fluoroquinolones.
According to pharmacodynamics:
They have a wider spectrum of activity, including:
- staphylococci (including PRSA);
- gram-negative cocci (gonococcus, meningococcus, M. catarrhalis);
- gram-positive rods (listeria, corynebacteria, anthrax pathogens);
- gram-negative bacilli of the Enterobacteriaceae family, including multidrug-resistant (E.coli, Salmonella, Shigella, Proteus, Enterobacter, Klebsiella, Serration, Providence, Citrobacter, Morganella), P.aeruginosa, and Campylobacter.
- certain drugs (ciprofloxacin, ofloxacin, lomefloxacin, etc.) are active against M. tuberculosis;
- act on some intracellular microorganisms (legionella).
Another advantage of second generation fluoroquinolones is that they:
- create high concentrations in the blood and tissues when taken orally, and bioavailability does not depend on the time of food intake;
- penetrate well into various organs and tissues: lungs, kidneys, prostate;
- have a long half-life and are prescribed 1-2 times a day.
According to portability:
- Side effects on second-generation fluoroquinolones from the gastrointestinal tract and central nervous system are less common;
- Second generation fluoroquinolones can be used for renal failure.
Microbiological features of second generation fluoroquinolones:
- most streptococci (including pneumococcus), enterococci, chlamydia, mycoplasma are insensitive;
- have no effect on spirochetes, listeria and most anaerobes.
Microbiological features of third generation quinolones:
- have higher activity against pneumococci (including penicillin-resistant) and atypical pathogens (chlamydia, mycoplasma).
Microbiological characteristics of fourth generation quinolones:
- in terms of antipneumococcal activity and effect on atypical pathogens, they are superior to quinolones of previous generations;
- have high activity against non-spore-forming anaerobes (B.fragilis, etc.), which makes it possible to use them for intra-abdominal and pelvic infections as monotherapy.