If a bacterial infection develops, it is imperative to take antibiotics, which are prescribed in a short course for no more than 7 days, so that resistance does not develop. Doctors often recommend Ciprofloxacin or Levofloxacin, but the patient may be intolerant, then they use analogues.
Comparison of the effectiveness of Levofloxacin and Moxifloxacin
Moxifloxacin is more effective than Levofloxacin - this means that the ability of the drug substance to provide the maximum possible effect is different.
For example, if the therapeutic effect of Moxifloxacin is more pronounced, then it is impossible to achieve this effect with Levofloxacin, even in large doses.
Also, the speed of therapy is an indicator of the speed of therapeutic action; Moxifloxacin and Levofloxacin are also different, as is bioavailability - the amount of a drug substance reaching the site of its action in the body. The higher the bioavailability, the less it will be lost during absorption and use by the body.
Efficacy of treatment with analogues
Ciprofloxacin and Levofloxacin are high-quality antibacterial agents. They are used for infectious and inflammatory pathologies. With the correct course of application and dosage, a quick effect occurs. If there are contraindications for use, it is better to buy analogues.
The therapeutic effect of analogues is observed in the case of using the drug prescribed by a doctor. Only he knows what is better to use, Amoxiclav, Sumamed or Azithromycin. It is advisable to first carry out a bacteriological culture of the separated organ (for example, the nasopharynx) in order to know which active substance will affect the body, eliminating the infection.
If the condition continues to worsen, the drug may have been prescribed incorrectly. It is recommended to conduct a general blood and urine test to determine the condition of the body. Thanks to the selection of analogues, doctors will be able to continue treating infectious pathologies, even if the first medicine did not lead to positive dynamics. Improvements are evidenced by a decrease in body temperature, appearance of appetite, elimination of pain and redness, and body activity. Before choosing a substitute, look at whether the drug is approved during pregnancy, lactation, and childhood.
Comparison of the safety of Levofloxacin and Moxifloxacin
The safety of a drug includes many factors.
At the same time, with Levofloxacin it is quite similar to Moxifloxacin. It is important where the drug is metabolized: drugs are excreted from the body either unchanged or in the form of products of their biochemical transformations. Metabolism occurs spontaneously, but most often involves major organs such as the liver, kidneys, lungs, skin, brain and others. When assessing the metabolism of Levofloxacin, as well as Moxifloxacin, we look at which organ is the metabolizing organ and how critical the effect on it is.
The risk-benefit ratio is when the prescription of a drug is undesirable, but justified under certain conditions and circumstances, with the obligatory observance of caution in use. At the same time, Levofloxacin does not have any risks when used, just like Moxifloxacin.
Also, when calculating safety, it is taken into account whether only allergic reactions occur or possible dysfunction of the main organs. In other matters, as well as the reversibility of the consequences of the use of Levofloxacin and Moxifloxacin.
What is Levofloxacin?
Levofloxacin is a broad-spectrum antibiotic based on the active substance of the same name. The drug is produced in the form of tablets, injection solution, and eye drops. The following pharmacological action is determined:
- bactericidal effect due to blocking DNA gyrase and topoisomerase 4;
- suppression of bacterial cell DNA synthesis, preventing the formation of a membrane, as a result it dies;
- destruction of gram-positive and gram-negative bacteria, anaerobes.
The drug is indicated for use in infectious and inflammatory diseases. Eliminate bacterial infection of the nasopharynx, respiratory tract, urinary system, skin and soft tissues, and abdominal area. The drug is effective against tuberculosis, but in complex therapy.
The medicine is not approved for use in children, with the exception of complex therapy for cystic fibrosis and pneumonia.
There are many side effects. They arise from the digestive system, cardiovascular and nervous systems, metabolism, sensory organs, musculoskeletal system, urinary system, and immunity. The drug is prohibited for individual intolerance, epilepsy, pregnancy and lactation. Use with caution in old age. Patients are interested in Levofloxacin and alcohol, whether there is compatibility, and what the consequences are. It is prohibited with any drink containing ethyl alcohol.
Comparison of addiction between Levofloxacin and Moxifloxacin
Like safety, addiction also involves many factors that must be considered when evaluating a drug.
So, the totality of the values of such parameters as “syndrome o” for Levofloxacin is less than the similar values for Moxifloxacin. Withdrawal syndrome is a pathological condition that occurs after the cessation of intake of addictive or dependent substances into the body. And resistance is understood as initial immunity to a drug; in this it differs from addiction, when immunity to a drug develops over a certain period of time. The presence of resistance can only be stated if an attempt has been made to increase the dose of the drug to the maximum possible.
Characteristics of Ciprofloxacin
Ciprofloxacin is a broad-spectrum antibiotic. Its price is not expensive, but its effectiveness is high. It is based on the active substance of the same name, which causes the following pharmacological action:
- suppression of bacterial DNA gyrase;
- disruption of DNA synthesis, which prevents the growth and reproduction of bacterial cells;
- bactericidal effect on gram-negative and gram-positive microorganisms;
- low toxicity to the human body and its tissues.
The drug is produced in injections for intravenous infusion, tablets, and eye drops. Therefore, the drug is suitable for the treatment of many diseases. It is recommended to use it for infectious and inflammatory pathologies of the following parts of the body:
- upper and lower respiratory tract;
- organs of vision;
- urinary system, genitals;
- circulatory system during the development of sepsis;
- digestive tract;
- nasopharynx.
Ciprofloxacin is one of the latest generation antibiotics. It is allowed to be used by both adults and children. Its effectiveness is high, so it is possible to treat even such pathologies as sepsis, anthrax, cystic fibrosis (in complex therapy). There are many side effects, they occur in almost every system of the body. Therefore, the drug is used only under the supervision of a doctor in limited dosages.
Comparison of side effects of Levofloxacin and Moxifloxacin
Side effects or adverse events are any adverse medical event that occurs in a subject after administration of a drug.
Levofloxacin has more adverse effects than Moxifloxacin. This implies that the frequency of their occurrence is low with Levofloxacin and low with Moxifloxacin. Frequency of manifestation is an indicator of how many cases of an undesirable effect from treatment are possible and registered. The undesirable effect on the body, the strength of influence and the toxic effect of drugs are different: how quickly the body recovers after taking it and whether it recovers at all. When using Levofloxacin, the body's ability to recover faster is higher than that of Moxifloxacin.
The place of levofloxacin in the pharmacotherapy of community-acquired pneumonia
P
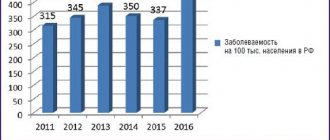
According to current estimates, in our country there are 1.5 million cases of pneumonia annually [1], which allows us to consider this disease as one of the most problematic for domestic healthcare.
The need to regularly address the topic of pharmacotherapy for community-acquired pneumonia (CAP)
can be explained by at least two reasons: changes in the spectrum and resistance of CAP pathogens and the emergence
of new antibacterial drugs (ABPs)
.
In particular, in recent years there has been a decrease in the sensitivity of the main causative agent of CAP – S.pneumoniae
to ABPs, often used in routine practice. Thus, according to the PeGaS-1 study, the proportion of pneumococcus resistant to tetracycline and co-trimoxazole is 34% and 38%, respectively. Approximately 4% of strains of this microorganism are resistant to macrolides (including azithromycin). The greatest concern is the increase in the resistance of this pathogen to penicillin (and at the same time a decrease in the effectiveness of other b-lactams) - 7.5% in children and up to 9% in adults, and the maximum level of resistance to penicillin (up to 20% in some hospitals) is observed in Moscow and large cities [2].
On the other hand, pharmacotherapy for CAP in our country is still far from optimal. According to a large (778 outpatients in 7 cities of Russia, including Moscow and St. Petersburg) pharmacoepidemiological study [3], general practitioners most often use gentamicin (29.3%), co-trimoxazole (22.7%) in the treatment of CAP. ), ampicillin (20.3%) and ciprofloxacin (17.2%).
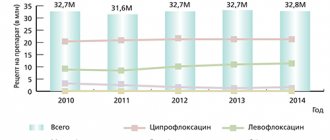
At the same time, the most promising drugs for outpatient treatment of respiratory infections - respiratory fluoroquinolones - did not find a place in the list of prescriptions at all.
Meanwhile, since the mid-90s, respiratory fluoroquinolones
(levofloxacin, sparfloxacin) have taken a strong place in the algorithms for choosing ABPs, built on the principles of evidence-based medicine (recommendations of the Society of Infectious Diseases, USA, 1998 [4]; Guidelines of the American Thoracic Society, 2001 [5]; recommendations of the British Thoracic Society, 2001 [6] ). As an example, we can point to a significant increase in the use of fluoroquinolones in the United States (Fig. 1), where since the late 90s, these ABPs have been used in clinical practice much more often than third-generation cephalosporins and aminoglycosides.
Rice.
1. Trends in the use of antibiotics in the USA (1989-99) [7] The widespread use of respiratory fluoroquinolones in the treatment of CAP
is due to several main reasons:
- respiratory fluoroquinolones are broad-spectrum drugs that are potentially active against all the most common pathogens of CAP (see Table 1) - gram-positive microorganisms (pneumococci, staphylococci), most gram-negative and intracellular pathogens, as well as mycobacterium tuberculosis and some anaerobes;
- resistance S. pneumoniae
and other common causative agents of CAP to drugs in this group has remained virtually unchanged over the past decade (although this trend still occurs - see Fig. 2). At the same time, the proportion of penicillin-resistant pneumococcal strains in a number of countries has increased 5–10 times. In addition, there is no reason to predict a rapid increase in the number of microorganisms that are immune to the action of fluoroquinolones, since the emergence of resistance is determined by mutation of two different sections of microbial DNA at once [2], and the probability of such an event is quite low;Rice. 2. Dynamics of resistance of S. pneumoniae to fluoroquinolones (data from the Cross-Canada Surveillance Study)
- many respiratory fluoroquinolones are available both in forms for intravenous (IV) administration and for oral administration, which allows for so-called step therapy ( Step therapy is a two-step use of ABP, that is, a transition from parenteral to oral route of administration.
) [8]; - Most respiratory fluoroquinolones have advantageous pharmacokinetic properties that allow them to be used once or twice daily.
But at the same time, we have to admit that the cost of respiratory fluoroquinolones is significantly higher than the cost of antibacterial drugs used in routine practice; in addition, there remains a ban on the use of drugs from this group for the treatment of children and pregnant women.
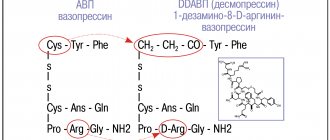
Of the third generation fluoroquinolones on the domestic market, levofloxacin (Tavanic)
Forms for intravenous administration and for oral administration are registered. This is the most common drug among third generation fluoroquinolones. This review aims to show the place of this ABP in modern pharmacotherapy of community-acquired pneumonia.
Pharmacokinetics/pharmacodynamics of levofloxacin
Levofloxacin is almost completely absorbed in the intestine (bioavailability after oral administration is 99%). Its half-life is 6-8 hours, which allows the use of levofloxacin once a day (daily dose - 500 mg). The equilibrium concentration in plasma when taken once a day is established 48 hours after the start of treatment. The drug penetrates well into tissues (volume of distribution - 89–112 l); after a single dose, the concentration in the lung tissue is 2–5 times higher than the concentration in the blood [9]. In the fluid on the surface of the epithelium of the lower respiratory tract, levofloxacin accumulates in a concentration 12 times higher than the minimum inhibitory concentration (MIC) for S. pneumoniae
(see Fig. 3).
Rice. 3. The ratio of the concentration of fluoroquinolones in the liquid on the surface of the bronchial epithelium to the MIC value for S. pneumoniae [9]
In general, the pharmacokinetic parameters of levofloxacin are not inferior to those of other third-fourth generation fluoroquinolones - gatifloxacin and moxifloxacin.
To assess the pharmacodynamics and effectiveness of fluoroquinolones, the ratio of the area under the pharmacokinetic curve (AUC) to the minimum inhibitory concentration MIC90% of the pathogen is crucial (Fig. 4) [10]. The effect of the use of drugs should be expected only if the AUC/MIC value is 90%
- Rice. 4. The ratio of pharmacokinetic (Cmax, AUC24) and pharmacodynamic (MIC90%) parameters that determine the effectiveness of fluoroquinolones [10]
- >25–30 for S.pneumoniae
(or >15 [11]) - > 100 for gram-negative pathogens [10].
It should be noted that levofloxacin is effective against most pathogens of respiratory infections, although against S. pneumoniae
its predicted effectiveness is less than that of fourth generation fluoroquinolones.
In addition, due to its high blood concentration, levofloxacin demonstrates very high efficacy in patients with bacteremia. The spectrum of antimicrobial action of levofloxacin is presented in Table 2.
Clinical studies of levofloxacin
In a large multicenter randomized clinical trial (RCT) [12], the effectiveness of intravenous administration and oral administration of levofloxacin was assessed in 590 patients with CAP compared with third-generation cephalosporins (ceftriaxone IV and cefuroxime orally). Eradication of pathogens with the use of levofloxacin was achieved in 98% of cases (with the use of cephalosporins - 85%). The studied drugs did not differ in effectiveness against pneumococcus, but levofloxacin was more effective in patients with H. influenzae
and atypical pathogens (Table 3).
In a large multicenter randomized clinical trial (RCT) [12], the effectiveness of IV and oral levofloxacin was assessed in 590 patients with CAP compared with third-generation cephalosporins (IV ceftriaxone and oral cefuroxime). Eradication of pathogens with the use of levofloxacin was achieved in 98% of cases (with the use of cephalosporins - 85%). The studied drugs did not differ in effectiveness against pneumococcus, however, levofloxacin was more effective in patients with and atypical pathogens (Table 3).
In another study in hospitalized patients with CAP (moderate to severe pneumonia) [13], levofloxacin (500 mg IV twice daily) and ceftriaxone (4.0 g IV once daily) demonstrated equal microbiological efficacy (pathogen eradication in 83% when using both ABPs).
A recent study (2002) compared intravenous levofloxacin in patients with severe CAP treated in hospital with a combination of intravenous azithromycin and ceftriaxone (The combination of third-generation cephalosporins and macrolides is supported by guidelines for the treatment of CAP published American Thoracic Society and European Pulmonary Society, and is one of the standards for the treatment of severe pneumonia in a hospital setting.
) i/v [14].
The results of this study (a total of 236 patients) were somewhat surprising, since levofloxacin monotherapy was at least as effective ( In the levofloxacin and clarithromycin/ceftriaxone groups, clinical effectiveness was estimated to be 94.1% and 92.3%, and microbiological effectiveness - 89.5% and 92.3%, respectively 3
) as the combination treatment, in addition, levofloxacin was better tolerated by patients.
Levofloxacin did not differ statistically significantly from modern macrolides (clarithromycin) in both clinical and microbiological effectiveness [15].
According to the results of one RCT [16], levofloxacin and gatifloxacin are equally effective in the treatment of mild and moderate CAP, but gatifloxacin was slightly more effective in the treatment of severe CAP (Table 4).
In general, a meta-analysis of 5 large RCTs (1067 patients with CAP) showed that
the effectiveness of levofloxacin in pneumonia is 83–100%
(for comparison drugs – 90–95%) [17].
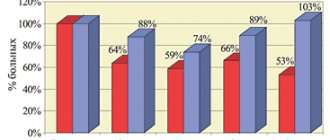
Safety
The main adverse drug reaction (ADR) of levofloxacin is its proarrhythmogenic effect, manifested by prolongation of the QT interval on the ECG (on average, according to RCT data, by 5 ms). However, in this regard, levofloxacin appears to be safer than sparfloxacin (similar value 13–15 ms) or erythromycin (8–15 ms). In terms of the overall incidence of ADRs and the frequency of drug withdrawal due to ADRs (Fig. 5, 6), levofloxacin is one of the safest fluoroquinolones [18,19].
Rice. 5. Frequency of ADRs when taking fluoroquinolones (%) [18,19]
Rice.
6. The need to discontinue fluoroquinolones due to the development of ADRs (%) [18,19] Foreign recommendations for the use of levofloxacin
Respiratory quinolones are considered by a number of authors as the drugs of choice for the treatment of pneumonia caused by penicillin-resistant strains of pneumococcus (PRP) [20–23]. The US Food and Drug Administration (FDA) approved levofloxacin as a treatment for respiratory infections caused by PRP, based on cumulative data from 8 RCTs involving more than 3900 patients [24]. Of this large number of patients, PRP was the causative agent of pneumonia in 18 cases, and the effectiveness of levofloxacin could be assessed only in 15 patients. In all these cases, levofloxacin was clinically effective.
Respiratory quinolones are considered by a number of authors as the drugs of choice for the treatment of pneumonia caused by penicillin-resistant pneumococcal strains (PRP) [20–23]. The US Food and Drug Administration (FDA) approved levofloxacin as a treatment for respiratory infections caused by PRP, based on cumulative data from 8 RCTs involving more than 3900 patients [24]. Of this large number of patients, PRP was the causative agent of pneumonia in 18 cases, and the effectiveness of levofloxacin could be assessed only in 15 patients. In all these cases, levofloxacin was clinically effective.
The widest indications for the use of levofloxacin and the fourth generation drug, moxifloxacin, exist in the USA [25], where the proportion of penicillin-resistant pneumococcal strains ranges from 17.9% to 33.8% for different states (2001). According to these recommendations (see Table 5), levofloxacin is a second-line drug for patients with mild pneumonia who do not require hospitalization and hospitalized patients without severe comorbidities. In other cases, levofloxacin is prescribed as a first-line drug for empirical therapy, and there is a tendency to use it in combination with ceftriaxone4, which provides greater effectiveness in the treatment of severe CAP (see Table 6).
Experts from the UK, where the level of pneumococcal resistance remains the lowest in Western Europe (only 6.7%; 2001), have a more restrained approach to prescribing levofloxacin [6]. In the British Thoracic Society recommendations, levofloxacin5 is assigned the role of a second-line drug for the treatment of CAP in a hospital setting (in the treatment of severe CAP, it is recommended to be prescribed in combination with penicillin).
conclusions
Based on the above, the use of levofloxacin in our country is justified due to its high efficiency and can be effectively used for:
A) treatment of CAP on an outpatient basis
(taking levofloxacin orally as monotherapy) –
- in patients with ineffective initial treatment (penicillins, macrolides, oral cephalosporins, etc.).
- in patients at high risk of infection with resistant pneumococcus:
– age > 65 years
– treatment with b-lactam antibiotics during the last 3 months.
– alcoholism
– immunosuppressive conditions, including glucocorticosteroid therapy
– severe combined diseases [5].
B) treatment of CAP in a hospital
–
When treating CAP in a hospital, levofloxacin should be prescribed intravenously; a stepwise approach to treatment seems rational [8]: transition to oral administration of the drug after clinical improvement of the patient’s condition and microbiological eradication of the pathogen [6].
Combined use of levofloxacin with other antibacterial drugs:
- levofloxacin IV + III generation cephalosporins IV – in the treatment of pneumonia caused by S. pneumoniae
resistant to penicillin (MIC for penicillin >2 μg/ml) and macrolides. - levofloxacin IV + III generation cephalosporins IV +/– aminoglycosides – in patients with bronchiectasis and patients with severe pneumonia (in ICU conditions).
Literature:
1. Chuchalin A.G., Tsoi A.N., Arkhipov V.V. et al. Pneumonia from the point of view of evidence-based medicine, M., 2000, p. 111.
2. Strachunsky L.S., Bogdanovich T.M. The state of antibiotic resistance in Russia. In the book: Antibacterial therapy. Practical guide. Edited by L.S. Strachunsky, Yu.B. Belousova, S.N. Kozlova; Moscow, 2000, p. 7–11.
3. Kozlov S.N., Rachina S.A., Domnikova N.P. et al., Pharmacoepidemiological analysis of the treatment of community-acquired pneumonia in an outpatient setting. Clinical microbiology and antimicrobial chemotherapy, 2000; Volume. 2(3): p. 74–81.
4. Bartlett, JG, Breiman, RF, Mandell, LA, File, TM, Jr. Community-acquired pneumonia in adults: Guidelines for management. Guidelines from the Infectious Disease Society of America. Clin Infect Dis 1998; 26:811.
5. Guidelines for the Management of Adults with Community–Acquired Pneumonia. Diagnosis, Assessment of Severity, Antimicrobial Therapy, and Prevention, Am J Respir Crit Care Med, 2001; Vol 163:1730–1754
6. BTS Guidelines for the Management of CAP in adult, Thorax, 2001; 56 (sapi. 4).
1. Hooper DC Macrolides, Fluoroquinolones, and Aminoglycosides. Lecture given at Massachusetts General Hospital on July 10, 2002.
8. Sinopalnikov A.I., Duganov V.K. Levofloxacin: stepwise therapy for community-acquired pneumonia in adults. RMJ, 2001; volume 9(15): p. 650–655.
9. Wise R, Honeybourne D: Pharmacokinetics and pharmacodynamics of fluoroquinolones in the respiratory tract. Eur Resp J 1999; 14:221–229
10. Schentag J. and Tillotson G. S. Chest, 1997; 112(6 Suppl): 314–319.
11. Preston SL, Drusano GL, Berman AL, et al. Levofloxacin population pharmacokinetics and creation of a demographic model for prediction of individual drug clearance in patients with serious community–acquired infection. Antimicrob Agents Chemother 1998;42:1098–104
12. File TM et al. A multicenter, randomized study comparing the efficacy and safety of intravenous and/or oral levofloxacin versus ceftriaxone with community–acquired pneumonia 1997;41:1965–1972.
13. Norrby RS et al. A comparative study of levofloxacin and ceftriaxone in the treatment of hospitalized patients with pneumonia 1998;30:397–404.
14. Frank E, Liu J, Kinasewitz G, Moran GJ et. al. A multicenter, open–label, randomized comparison of levofloxacin and azithromycin plus ceftriaxone in hospitalized adults with moderate to severe community–acquired pneumonia. Clin Ther 2002 Aug;24(8):1292–308
15. Gotfried MH, Dattani D, Riffer E et. al. A controlled, double–blind, multicenter study comparing clarithromycin extended–release tablets and levofloxacin tablets in the treatment of community–acquired pneumonia. Clin Ther 2002 May;24(5):736–51
16. Sullivan JG et al. J Resp Dis 20(11 suppl):S49 (1999)
17. Bru JP. Update on the role of levofloxacin in the management of acute community–acquired pneumonia. Presse Med 2002 Jun 15;31(21 Pt 2):S19–22
18. Ball P, Mandell L, Niki Y, et al: Comparative tolerance of the newer fluoroquinolone antibacterials. Drug Saf 21:407–421, 1999
19. Breen J, Skuba K, Grasela D: Safety and tolerability of gatifloxacin, an advanced third-generation, 8-methoxy fluoroquinolone. J Respir Dis 20:S70–S76, 1999 (suppl 11).
20. Bartlett, JG, Breiman, RF, Mandell, LA, File, TM, Jr. Community-acquired pneumonia in adults: Guidelines for management. Guidelines from the Infectious Disease Society of America. Clin Infect Dis 1998; 26:811.
21. George, J, Morrissey, I. The bactericidal activity of levofloxacin compared with ofloxacin, D–ofloxacin, ciprofloxacin, sparfloxacin and cefotaxime against Streptococcus pneumoniae. J Antimicrob Chemother 1997; 39:719.
22. Klugman, KP, Gootz, TD. In–vitro and in–vivo activity of trovafloxacin against Streptococcus pneumoniae. J Antimicrob Chemother 1997; 39 Suppl B:51.
23. Hoogkamp–Korstanje, JA. In–vitro activities of ciprofloxacin, levofloxacin, lomefloxacin, ofloxacin, pefloxacin, sparfloxacin and trovafloxacin against gram–positive and gram–negative pathogens from respiratory tract infections. J Antimicrob Chemother 1997; 40:427.
24. From the Food and Drug Administration. First drug for penicillin-resistant community-acquired pneumonia. JAMA 2000; 283:1679.
25. Community–Acquired Pneumonia (CAP) Year 2002. Antibiotic Selection and Management Update. Evaluation, Risk Stratification, and Current Antimicrobial Treatment Guidelines for Hospital–Based Management of CAP: Outcome–Effective Strategies Based on New NCCLS Breakpoints and Recent Clinical Studies – The ASCAP Panel Consensus Report, 2002, CLINICAL UPDATE; MARCH 1, 2002
Comparison of ease of use of Levofloxacin and Moxifloxacin
This includes dose selection taking into account various conditions and frequency of doses. At the same time, it is important not to forget about the release form of the drug; it is also important to take it into account when making an assessment.
The ease of use of Levofloxacin is approximately the same as Moxifloxacin. However, they are not convenient enough to use.
The drug ratings were compiled by experienced pharmacists who studied international research. The report is generated automatically.
Last update date: 2021-01-10 10:02:00
When to use analogues?
Levofloxacin, Ciprofloxacin are strong drugs. Not all patients tolerate them favorably. There are a lot of side effects that often occur with the wrong course of use or dosage. Analogues are prescribed in the following cases:
- individual intolerance to components;
- development of side effects after consumption;
- the need to use a different form of release, for example, instead of tablets, you need syrup for children.
When selecting analogues, you need to be careful. Preliminary tests are taken. It is advisable to carry out bacteriological culture. With its help, it is determined which bacteria causes infectious and inflammatory diseases, and whether the antibiotic will work. The study form contains a list of drugs to which there is high or average sensitivity, or lack thereof. OAC and OAM are prescribed, which are best reapplied after completion of treatment.
The positive effect of the analogue is indicated by a decrease in body temperature, elimination of suppuration, and a stable state of blood cells in the analysis.
When severe bacterial infections develop, Tsiprolet, Azithromycin, Amoxiclav, Sumamed, Tavanik and other drugs are prescribed. Use the correct release form. For example, for severe systemic infections, tablets or injections are used. If bacterial conjunctivitis has spread, drops are used.
Efficiency of Tsiprolet
Ciprolet is a medicine containing ciprofloxacin hydrochloride. The medicine is used in the form of tablets or drops. When they act on the body, the following effect occurs:
- wide spectrum of action on most pathogenic microorganisms of bacterial origin;
- influence on bacteria in the reproduction or dormant phase;
- complete destruction of the bacterial cell by suppressing DNA synthesis;
- influence on gram-negative and gram-positive anaerobes.
The drugs are absorbed into the gastrointestinal tract, bioavailability is above average. The connection with blood plasma proteins is low. Metabolism occurs in the liver. The drug is excreted through the kidneys with urine, and to a lesser extent with feces.
If the patient has renal failure, the dosage is reduced by half.
The drug helps with infectious and inflammatory diseases. It is used for infections of the respiratory tract, ENT organs, urinary and reproductive systems, gastrointestinal tract, biliary system, skin and soft tissues, and musculoskeletal system. The product has many contraindications and side effects, so it is used with caution.
Many patients are interested in what is the difference between Ciprolet and Ciprofloxacin. The difference lies in the form of release. The first drug is used in tablets or drops. Ciprofloxacin is produced additionally in the form of injections for intravenous administration.
Strong antibiotic Azithromycin
Azithromycin is a powerful drug based on the active substance of the same name. The release form is different, they produce drops, syrups, tablets, injections. The selection depends on the area of inflammation. Used in severe cases when the patient has a severe infection or resistance to other antibiotics. The following pharmacological actions are distinguished:
- suppression of protein synthesis in the microbial cell;
- inhibition of enzymatic activity and protein production of pathogenic microorganisms;
- influence on gram-positive and gram-negative bacteria, anaerobes.
The drug is indicated for infectious and inflammatory diseases. Effectively eliminates bacteria from the ENT organs, respiratory system, skin and soft tissues, and genitourinary tract. Like Ciprofloxacin, Azithromycin has many side effects and contraindications. If a patient asks which is better, Azithromycin or Levofloxacin, doctors answer that the first drug has a more aggressive effect on bacteria.
The product is prohibited for use during pregnancy and lactation. It penetrates the placental barrier and into mother's milk, negatively affecting the fetus and newborn. It is not recommended to use the drug for severe liver or kidney damage. But the medicine is approved for use in children in the form of syrup.
When is Amoxiclav prescribed?
Amoxiclav is a complex drug consisting of both amoxicillin and clavulanic acid. Due to the content of the substances, the effect on bacterial cells is enhanced. Bacteria that produce beta-lactamases, which form resistance to certain types of antibiotics, are destroyed. The following pharmacological actions are distinguished:
- bactericidal effect on infectious cells;
- inhibition of the synthesis of substances that form the bacterial cell wall;
- destruction of beta-lactamases.
Due to the double action, the destruction of persistent infections is ensured. The drug is used for infectious and inflammatory diseases. It destroys bacteria from the respiratory system, ENT organs, genitourinary system, skin and soft tissues. It is used for bone infections such as osteomyelitis.
Unlike Ciprofloxacin and Levofloxacin, Amoxiclav has fewer side effects.
The negative impact is manifested from the digestive tract, hematopoiesis, and nervous system. Allergic reactions and candidiasis may develop. The drug is contraindicated for phenylketonuria, mononucleosis of an infectious nature, and individual intolerance.
The product can be used with caution in certain conditions. For example, pregnancy and lactation, renal and liver failure. It is used for inflammation of the gastrointestinal tract, but in a smaller dosage.
Sumamed's influence
Sumamed is a drug based on azithromycin dihydrate. It is produced in the form of tablets and syrup. After consuming the dose, absorption occurs in the gastrointestinal tract. Bioavailability is low, metabolism occurs in the liver. The substance loses activity. Excretion occurs to a greater extent through the intestines, and to a lesser extent through urine. The following pharmacodynamics occurs:
- destruction of gram-positive and gram-negative pathogenic microorganisms;
- bacteriostatic effect on cells;
- wide spectrum of action;
- suppression of protein synthesis and enzymatic activity in the microbial cell.
The product is used for infectious and inflammatory diseases of the ENT organs, respiratory tract, skin and soft tissues, and genitourinary tract. It is used for Lyme disease or borreliosis. There are many side effects, so you need to be careful with the course of use and dosage.
It is unacceptable to use the medicine if you are hypersensitive to azithromycin, erythromycin and other substances from the macrolide group. It is forbidden to use the drug for severe liver pathologies or deficiency of enzymes that process excipients. The medicine is used for children, but a different dosage and release form must be used than for adults. Suitable syrup with a course of treatment of 5-7 days.
Distinctive features of Zinnat
Zinnat is a product containing cefuroxime axetil. The drug has a strong effect on the body, but destroys severe infections in different parts. Thanks to it, the following pharmacodynamics are ensured:
- simultaneous bactericidal and bacteriostatic effect;
- resistance to the influence of beta-lactamases;
- suppression of bacterial cell wall synthesis;
- binding to major target proteins.
The drug is active against gram-positive and gram-negative anaerobes, chlamydia, mycoplasma, legionella. Absorption of the drug occurs in the gastrointestinal tract. Metabolism does not occur. Excretion occurs through the kidneys; a toxic effect on the glomeruli and tubular secretion is possible. Therefore, the medicine is used with caution in chronic pathologies of this organ.
The drug is indicated for use in infectious and inflammatory diseases.
Pathologies of the ENT organs, respiratory system, genitourinary tract, skin and soft tissues are eliminated. It is used to treat Lyme disease. There are many side effects and contraindications, so the dosage is used with caution. The drug is suitable for children from 3 months, if you use the suspension form. For women who are pregnant or lactating, the drug is recommended to be used in cases of strict necessity.