Chemical properties
Vasopressin is described on Wikipedia as an antidiuretic hormone of the hypothalamus that increases the reabsorption of fluid by the kidneys, increasing the concentration of urine and decreasing its volume.
The substance molecule consists of 9 amino acids , in humans the amino acid sequence looks like Cys-Tyr-Phe-Gln-Asn-Cys-Pro-Arg-Gly , the Cys1 and Cys6 are connected by a disulfide bond.
The hormone Vasopressin is synthesized in the body in the large cell neurons of the hypothalamus. The hormone synthesized in the body of the neuron is redirected to the synapses with the help of axons and accumulates in presynaptic vesicles, from where it is excreted into the blood at the moment when the neuron is excited by a nerve impulse.
Most often, the synthetic hormone is produced in the form of solutions for injection or intranasal administration.
Pharmacodynamics and pharmacokinetics
Vasopressin interacts with V and Vi receptors , which are located on vascular smooth muscle cells, thus regulating vasoconstriction. There is an increase in the permeability of the epithelium of the collecting duct for water located in the kidneys and an increase in the process of fluid reabsorption. The substance causes an increase in the volume of blood circulating in the body, hyponatremia and a decrease in osmolarity.
The drug is also capable of increasing the tone of the smooth muscles of internal organs, in particular the gastrointestinal tract, by interacting with V1a receptors . This leads to increased vascular tone and increased peripheral vascular resistance. Blood pressure increases (the medicine narrows the arterioles). The hormone Vasopressin has a hemostatic effect, spasms small vessels and capillaries, affects the von Willebrand blood clotting factor, and stimulates platelet .
The substance also affects the central nervous system, takes part in the regulation of aggression and the process of memorization. Scientists conducted experiments on mice - prairie voles. In the course of these studies, by influencing vasopressin receptors in the brains of animals, mice were able to be made monogamous, faithful to one partner. Thus, it was possible to prove that vasopressin (its AVPR1A) is responsible for the social behavior of animals, finding a partner and the formation of paternal instinct in males.
Synthetic hormone preparations are prescribed parenterally. When administered by injection or intranasally, the half-life of the substance is about 20 minutes. Metabolism of the drug occurs in the tissues of the liver and kidneys, where disulfide bonds are restored and further breakdown of peptides . A small amount of the substance is excreted unchanged in the urine.
Treatment of central diabetes insipidus
Immediately after the diagnosis of CND is established, patients should be prescribed continuous replacement therapy with arginine vasopressin drugs - the only effective way to treat insufficiency of ADH production [19, 20]. Considering, as a rule, the chronic nature of the disease, the main requirements for drug therapy for CND are as follows: easy tolerability, ease of use, no limitation of the patient’s life activity, the possibility of individual selection of the drug dose and long-term safety of the prescribed drugs, low risk of hyponatremia due to excessive fluid retention.
It should be remembered that patient education plays an important role in achieving the results of pharmacotherapy for CND [3]. During therapy with arginine vasopressin drugs, the patient should avoid consuming excess fluid and should limit fluid intake to the amount necessary to satisfy thirst. Fluid intake for any other reason should be avoided because, unlike individuals with normal ADH secretion, a patient with CND cannot rapidly increase the amount of urine output in response to increased fluid intake, which poses the risk of fluid retention and hyponatremia. It is believed that diuresis per day should not decrease below the normal level (15–30 mg/kg/day) [25]. Patient education to recognize signs of inadequate replacement therapy is also necessary.
At the first stages (1912) of the treatment of CND, they tried to use an extract (extract) from the posterior lobe of the pituitary gland of cattle as pharmacological agents. However, these drugs have not found use in the treatment of CND due to a short half-life, insufficient antidiuretic action and side effects due to the effect on other target organs for ADH, in particular, the vasoconstrictor effect [19, 26]. Work on the development of effective and safe agents for the treatment of CND was continued and in 1954 the synthesis of human arginine vasopressin was carried out. However, a real breakthrough in the treatment of CND was the prolonged synthetic analogues of the peptide, synthesized by minor changes in the native ADH molecule, devoid of the above disadvantages and possessing qualitatively new pharmacological properties [10, 11, 29].
Among modern drugs for replacing ADH deficiency, 1-deamino-8-D-arginine vasopressin (desmopressin) has the greatest antidiuretic activity. Its chemical structure differs from the natural ADH molecule by two changes (deamination of 1-cysteine and replacement of 8-L-arginine with D-arginine), which gives it a number of therapeutic advantages confirmed in practice [19, 32] (Fig. 3).
Rice. 3. Structure of vasopressin and desmopressin.
The main pharmacological effect of desmopressin, the antidiuretic effect, is realized through interaction with specific membrane V2 receptors localized in the renal tubules and responsible for the reabsorption of water in the kidneys. The ability of desmopressin to activate V2 receptors is almost twice as high as that of ADH. Unlike natural ADH, due to the substitution of L-arginine at position 8 with D-arginine, desmopressin selectively activates V2 receptors and does not affect V1 receptors of smooth muscle cells of blood vessels and internal organs. Because of this, the ratio of antidiuretic activity to pressor activity for desmopressin is approximately 2000:1 versus 1:1 for the natural peptide. The desmopressin molecule is distinguished by its resistance to destruction. Additional deamination of cysteine in the 1st position not only increases the ratio of the antidiuretic activity of the peptide to the pressor activity, but also makes it possible to have a much longer antidiuretic effect – up to 12 hours [19, 32].
So, in comparison with natural vasopressin, the antidiuretic effect of desmopressin is most pronounced both in strength and duration of the pharmacological effect; it is also important that the drug is practically devoid of pressor activity.
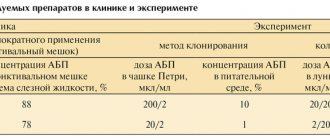
Currently, various dosage forms of desmopressin are available that compensate for ADH deficiency in CND and have proven efficacy and safety (Table 2). Each form has its own advantages and disadvantages, which allows in practice to choose an approach based on the individual characteristics of the patients’ clinical profile [4, 10, 14, 23].
Table 2. Comparative characteristics of various dosage forms of desmopressin
| Dosage form of desmopressin | Intranasal spray | Tablet oral form (0.1 and 0.2 mg) | Tablet sublingual form (60, 120 and 240 mcg) |
| Start of action | 15–30 min | 1–2 hours | 15–45 min |
| Clinically significant blood concentration | 60 min | 2–4 hours | 60 min |
| Duration of action | 8–24 hours | 8–12 h | 8–12 h |
| Mode of application | Intranasally | The drug should be taken after meals | Sublingual, for resorption; do not take the tablet with liquid |
| Initial dose of the drug | 10 mcg 2 times a day | 0.1 mg 1–3 times daily | 60 mcg 3 times daily |
| Average daily dose | 10–40 mcg | 0.2–1.2 mg | 120–720 mcg |
For a long time, desmopressin was used intranasally as a replacement therapy for CND [11]. However, this dosage form did not always provide stable effectiveness of the antidiuretic effect throughout 24 hours. In particular, according to clinical studies, the duration of action after intranasal administration varies for a dose of 20 mcg from 8 to 24 hours, for a dose of 5–10 mcg - from 4 to 18 o'clock [32]. In addition, the high individual variability in the effect of this form of desmopressin can make it difficult to select the dose and increases the risk of developing hyponatremia [15]. Another disadvantage of this form of desmopressin is that absorption may be impaired in patients with pathology of the nasal mucosa, which certainly limits the use of the drug in the event of catarrhal phenomena or chronic rhinitis [3, 14]. In addition, intranasal administration of desmopressin may cause side effects on the mucous membrane of the nasal passages. You should be aware of contraindications to the intranasal use of desmopressin, which include allergic rhinitis, nasal congestion, swelling and scarring of the nasal mucosa, and upper respiratory tract infections.
The next stage in the development of pharmacotherapy for CND was the development of an oral form of desmopressin (Minirin), available in tablets of 0.1 and 0.2 mg. The dose of Minirin is selected individually, ranging from 0.025 to 1 mg/day with a dosage frequency of 1–3 times a day and does not depend on the age and body weight of the patient [10]. However, this form of desmopressin is not without drawbacks due to the peculiarities of its use [13]. In particular, the tablets must be taken with water, which is not always possible in some patients. Due to rapid degradation by gastrointestinal dipeptidases, the bioavailability of this form of desmopressin is quite low (0.16%). Therefore, taking with food reduces the absorption of the oral form of desmopressin, and therefore it is recommended to take the drug on an empty stomach 30–40 minutes before or 2 hours after a meal, which is not always convenient for patients [11].
The development of modern therapy for CND was aimed at optimizing existing drugs, namely the development of new methods of administering desmopressin while maintaining effectiveness and safety, which can improve the quality of life of patients and make treatment more comfortable [12, 24]. Taking into account the chronic nature of the disease in most cases, in order to obtain the necessary therapeutic effect, not only the effectiveness of desmopressin is important, but also how convenient this or that form is for patients to use.
New possibilities for the treatment of CND have appeared with the introduction into clinical practice of desmopressin in a convenient sublingual form - oral lyophilisate of desmopressin (Minirin Melt), available in dosages of 60 and 120 mcg [1, 13, 16]. A large number of dosages of the drug allows you to accurately select therapy, taking into account the individual characteristics of each patient with CND. The sublingual form of desmopressin dissolves quickly in the mouth; the drug has stable pharmacokinetics. The maximum concentration (Cmax) of desmopressin in the blood plasma is achieved within 0.5–2 hours after taking the drug and is directly proportional to the dose taken: after taking 200, 400 and 800 mcg, Cmax was 14, 30 and 65 pg/ml, respectively.
According to pharmacological studies, the bioavailability of desmopressin when administered sublingually in doses of 200, 400 and 800 mcg is about 0.24%, 0.28%, 0.25%, respectively, which is 60% higher than in oral form and is sufficient to cause a long-lasting antidiuretic effect [12, 24]. This makes it possible to treat patients with CND using lower doses compared to the tablet form of desmopressin, which reduces the risk of developing hyponatremia. In general, the risk of hyponatremia is higher in the elderly, presumably due to increased renal tubular sensitivity to ADH, impaired osmoregulation, decreased thirst, and impaired renal sodium retention [31]. The development of this complication is facilitated by excessive fluid intake.
The results of clinical studies indicate a lower risk of developing hyponatremia when using the sublingual form of desmopressin compared to intranasal administration of the drug [5, 14, 16]. Just like the tablet form of desmopressin, the sublingual form does not cause atrophy of the nasal mucosa.
The effectiveness and safety of the sublingual form of Minirina Melt for CND has been confirmed by international and Russian studies, including comparative studies with other dosage forms of desmopressin, on the basis of which conclusions were made about the possibility of using this drug in patients with this pathology of the hypothalamic-pituitary system. The use of desmopressin in sublingual form provides a long-term therapeutic effect of the drug: a decrease in the volume of urine excreted and a simultaneous increase in urine osmolality and a decrease in OPC [12, 13, 15, 23, 24].
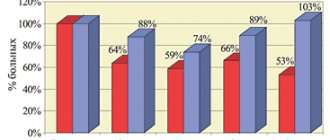
Of interest for clinical practice are the results of a multicenter open study by Arima H. et al., which consisted of studying the long-term clinical efficacy and safety of desmopressin for sublingual administration in patients with CND [5]. According to the study design, patients with CND who had previously received intranasal desmopressin spray were switched to a sublingual form of desmopressin; the observation period was 1 year. The study included 20 patients with CND (60% men) aged from 6 to 75 years (mean age – 39.6±19.5 years). Patients were transferred from the intranasal to sublingual form in the evening (patients began treatment with a dose of 60 mcg). Further titration of the dose was carried out depending on the onset of the therapeutic effect, for which the volume and osmolality of urine were controlled; the daily dose was reduced if the serum sodium level was ≤136 mmol/L. If there was no positive effect, the dose of the drug was increased in increments of 60 mcg. The average daily dose ranged from 60–180 mcg, while the maximum dose in the study group was 720 mcg (240 mcg 3 times a day). The study results demonstrated the long-term clinical efficacy and safety of sublingual desmopressin. The authors consider the use of sublingual desmopressin to be convenient, safe, and effective over long-term use.
Positive experience is accumulating in the use of sublingual desmopressin in patients with central nervous system dysfunction that developed as a result of surgical interventions for various brain tumors. Interesting and indicative are the results of a recent comparative study involving patients with CND after surgical treatment of brain tumors (n=51: 25 patients with craniopharyngioma, 21 with germinoma, 3 with glioma and 2 with pituitary adenoma) [1]. A single dose of oral Minirin ranged from 25 mcg to 200 mcg, a daily dose - from 25 to 600 mcg, the frequency of administration was from 1 to 4 times a day. According to the study design, patients recorded the amount of urine excreted, the time and dose of Minirin taken for 3 days. Next, oral Minirin was replaced with sublingual Minirin (at the rate of 100 μg oral equivalent to 60 μg sublingual). For 1 week, patients also noted in their diary the amount of urine excreted, the time of administration, and the amount of sublingual Minirin taken. The study assessed patient preference for formulation, efficacy, safety, compliance and ease of use.
As a result of a comparative analysis, it was shown that the clinical effectiveness of the sublingual form of Minirin is comparable to the oral form of Minirin: daily diuresis when taking the oral form was 1.5 ± 0.4 l/day, and when taking the sublingual form – 1.7 ± 0.5 l/day (p>0.05). There were no side effects from the use of the sublingual form.
As is known, along with effectiveness, a compelling argument in favor of choosing a particular drug is ease of use for the patient. At the end of the study, 60% of patients preferred the sublingual form of the drug; patients liked the absence of the need to take the tablet with water and adjust the drug intake depending on food intake. Moreover, the preference for the sublingual form of desmopressin did not correlate with the age of the patients, diagnosis, or duration of CND.
Clinical experience with sublingual desmopressin continues to grow. According to the national register of patients with CND in Denmark, for the period from 2007 to 2011. three quarters of patients with CND received the sublingual formulation, and no serious side effects were reported [16].
In clinical practice, it may be necessary to replace one form of desmopressin with another, and the following approximate dose conversion should be used (Table 3). In particular, when transferring a patient from an oral to a sublingual form, 60 mcg of the sublingual form corresponds to 100 mcg of the oral form.
Table 3. Dosage ratios between different forms of desmopressin
| Sublingual tablets | Pills | Aqueous nasal spray |
| 60 mcg | 0.1 mg | 5 mcg |
| 120 mcg | 0.2 mg | 10 mcg |
| 240 mcg | 0.4 mg | 20 mcg |
Minirin Melt is taken sublingually (the oral lyophilisate is held under the tongue until dissolved without adding water). The dose of the drug is selected individually and depends on the severity of polyuria in the patient; the tablet should not be taken with liquid. The recommended starting dose is 60 mcg 3 times a day, if necessary it is changed depending on the observed therapeutic effect, under the control of the amount of fluid drunk and excreted. Clinical experience suggests that the optimal maintenance dose is 60–120 mcg 3 times daily sublingually; The recommended daily dose is in the range of 120–720 mcg [6, 12]. Monitoring the effectiveness of treatment for CND is assessed by the clinical condition of the patient, the volume and relative density of urine. If there are complaints of swelling and severe headache, as well as changes in blood electrolytes, it is necessary to reduce the dose of desmopressin.
Contraindications to the use of desmopressin are hypersensitivity to desmopressin or other components of the drug; habitual or psychogenic polydipsia (with a urine output of 40 ml/kg/24 hours); heart failure and other conditions requiring the use of diuretics and children under 6 years of age. You should refrain from prescribing the drug in case of hyponatremia, impaired renal function (creatinine clearance below 50 ml/min). There were no side effects on the course of pregnancy, the health of the pregnant woman, the fetus and the newborn when taking Minirin.
When choosing a treatment for CND, it is necessary to take into account that the original sublingual form of desmopressin (Minirin Melt) has proven long-term high efficacy and safety in clinical studies and in real practice. At the same time, several generic drugs of desmopressin are currently registered in the Russian Federation (including Nativa, Nourem), the instructions for use of which contain references to clinical studies conducted with the original sublingual form of desmopressin. The lack of objective information on the therapeutic bioequivalence of original and generic desmopressin preparations does not allow clinicians to use generics with full confidence in the management of patients with ADH deficiency. Therefore, there is an obvious need to conduct comparative studies of the therapeutic bioequivalence of original and generic desmopressin preparations.
Side effects
During treatment with the drug, the following may develop:
- headaches, dizziness , nausea;
- pain and inflammation at the injection site;
- abdominal cramps;
- allergic skin rashes, itching, urticaria .
Also rarely, when using large dosages, the following may occur:
- ischemia , ventricular arrhythmia , or intestinal infarction ;
- cardiac arrest, necrosis .
Vasopressin, instructions for use (Method and dosage)
The drug is prescribed intramuscularly, intravenously or intranasally .
Vasopressin, instructions for use
glucose solution . The infusion is performed into a central or peripheral vein using a dispenser. 0.3 IU per minute is administered over half an hour, then increased by another 0.3 IU per minute every 30 minutes until the bleeding stops. The maximum dosage is 0.9 IU per minute. After stopping the bleeding, the dosage should be reduced. If any complications or unwanted side effects develop during therapy with the drug, the procedure must be interrupted.
To reduce the risk of adverse reactions, you can simultaneously administer nitroglycerin intravenously to the patient (10 mcg per minute, increasing every 15 minutes by the same amount).
For non- diabetes mellitus, synthetic analogues of Vasopressin are used according to the instructions and recommendations of the attending physician. Most often intranasally.
Central diabetes insipidus: etiology, pathogenesis, clinical picture and diagnosis
In most cases, insufficiency of ADH synthesis or secretion is a deficiency of neurosecretory cells that form the neurohypophysis. The etiological factors of CND are quite diverse (Fig. 2). CND may be of genetic origin; less than 5% of cases of the disease are associated with hereditary forms [7, 33]. The leading factor in the occurrence of the organic form of the disease, especially in childhood, is infection [4]. Common causes of the central nervous system are suprasellar and intrasellar tumors and cranial trauma. In almost half of children and a third of adult patients, the development of CND is associated with the presence of a primary or metastatic tumor in the hypothalamic-pituitary region (for example, lung cancer, breast cancer). The disease can also occur as a result of surgical or radiation intervention for tumors in the hypothalamic-pituitary region; Another common cause of the disease in adults (17% of cases) is trauma to the central nervous system (head injury, orbital injury, skull fractures) [20, 21, 26]. In addition, CND can manifest itself in the acute post-surgical, post-traumatic period, as a consequence of edema around the axons of vasopressin-containing neurons. Depending on the anatomical location of the damage to the central nervous system, it can be transient or permanent [26, 33]. In particular, in the case of localization of the pathological process above the median eminence with the involvement of vasopressin-synthesized cells of the supraoptic and paraventricular nuclei, the function of the latter is irreversibly lost. If the location of the pathological process is below the specified structure, then the disturbance of water balance often turns out to be transient [19, 21].
Rice. 2. Causes of central diabetes insipidus (CDI)
In recent years, it has been shown that the cause of CND may be an autoimmune process (the presence of antibodies to the neurons of the hypothalamus that synthesize ADH, and less often to the peptide itself). Lymphocytic infundibulo-neurohypophysitis may explain CDI in approximately half of patients with the idiopathic form of the disease. Another cause of idiopathic CDI may be subclinical neuroinfection or the initial growth of tumors in the hypothalamic-pituitary region, which requires repeated instrumental research methods [19, 20].
Among the rarer causes of CND, it is necessary to note systemic infiltrative diseases (sarcoidosis, histiocytosis, tuberculosis), vascular pathology (central aneurysms, thrombosis or hemorrhage, postpartum pituitary necrosis) and hemoblastoses (leukemia, lymphogranulomatosis, etc.).
It is worth adding that CND can be genetic and acquired, while the proportion of familial forms of the disease is less than 5%. In particular, DIDMOAD syndrome, or Wolfram syndrome, in which ADH deficiency develops due to aplasia of neurosecretory cells [4, 26].
Under the name “diabetes insipidus” diseases with different etiologies are combined. In contrast to CDI, nephrogenic diabetes insipidus (NDI) may be caused by impaired renal sensitivity to ADH. NND is observed both in congenital, hereditary inability of the kidneys (usually sex-linked, expressed only in men) to respond to the effects of ADH, and in some acquired conditions accompanied by renal tubular insensitivity to the hormone [19, 20]. Diabetes insipidus in pregnant women develops in one in 30,000 cases. This is a less common type of ND that occurs as a result of the destruction of endogenous vasopressin by placental arginine aminopeptidase. This form is observed only during pregnancy, more often in the middle or at the end of the period, and is called gestational ND [19].
The clinical picture in patients with CND consists of symptoms caused by ADH deficiency. The manifestation of the disease, as a rule, occurs with a significant decrease in the secretory activity of the neurohypophysis (by 80–90%). The main manifestation is a pathologically increased excretion of diluted urine (hypotonic polyuria - exceeding 2 l/m2/day or 40–50 ml/kg/day). ADH deficiency can be complete or partial, which determines the severity of polyuria. More often, the volume of urine increases to 5–6 l, although it often reaches 10–12 l, which requires urination both day and night, almost every hour [19, 20]. In children, the first symptom of the disease is usually bedwetting, and daytime urinary incontinence is often observed [4]. Plasma hyperosmolality (>300 mOsm/L), caused by severe polyuria, stimulates uncontrollable thirst (polydipsia), which does not stop at night. Patients drink large amounts of liquid, preferring chilled drinks. There is often a decrease in sweating and salivation.
Even in cases where polyuria is fully compensated by drinking plenty of fluids, the secretion of saliva and digestive juices is reduced, which leads to a deterioration in appetite. Due to the systematic consumption of large quantities of liquid, gastrointestinal disorders may occur: distension and prolapse of the stomach, constipation is common. Mental and emotional disorders are characteristic - headaches, insomnia, emotional imbalance up to psychosis, decreased mental activity. In connection with polyuria and polydipsia, insomnia appears, which is accompanied by physical and mental asthenia. Without adequate replenishment of excreted fluid and large diuresis practically not decreasing, dehydration becomes severe. Collapse develops and the filtration capacity of the kidneys decreases. The patient's body weight quickly drops and blood thickening occurs.
Clinically, it is important to remember that the course of CND may be complicated by other hypothalamic-pituitary disorders, just as the latter (Schien's syndrome, acromegaly, etc.) may include, at a certain stage of their development, manifestations of a lack of ADH secretion.
The success of treatment and prognosis in patients with CND directly depend on timely diagnosis based on the analysis of pathogenetic mechanisms, the correct choice of diagnostic methods and the prescription of effective treatment. The choice of treatment tactics should be based on an individual approach to pharmacotherapy in each specific case [28]. In typical cases, the diagnosis of CND is not difficult. Its confirmation is the identification of hypotonic polyuria, i.e. urine output more than 2 l/m2, or more than 40 ml/kg per day in older children and adults with low relative density (<1005–1010 g/l) or urine osmolality less than 300 mOsm/kg in the most concentrated portion; plasma osmolality more than 290 mOsm/kg [18, 19]. Hypernatremia is often detected.
In clinical practice, the differential diagnostic test with dry eating is most successfully used (with the exclusion of liquid from food and an increase in plasma osmolality, the specific gravity of urine in CND remains low), which makes it possible to differentiate CND from primary polydipsia, when there are no changes in ADH secretion and sensitivity to it [3 , 6]. The desmopressin test is performed for the differential diagnosis of CND and NDD [4].
The Zimnitsky test can provide some assistance in diagnosis. The sample should be evaluated taking into account possible extrarenal losses. With the preserved ability of the kidneys to osmotic dilute and concentrate urine, the following are noted:
- significant fluctuations in urine volume in individual portions (50–250 ml);
- the maximum relative density (RMD), which characterizes the ability of the kidneys to concentrate urine, should be no lower than 1025 g/l;
- the minimum TPR, reflecting the ability of the kidneys to osmotic dilute urine, in a healthy person should be lower than the osmotic concentration (osmolality) of protein-free plasma equal to 1010–1012, and is usually 1003–1006;
- significant fluctuations in TRP: the difference between the maximum and minimum indicators should be at least 12–16 units. (for example, from 1006 to 1020 or from 1010 to 1026, etc.);
- significant daily fluctuations in BPM are associated with the preserved ability of the kidneys to either concentrate or dilute urine depending on the constantly changing needs of the body;
- predominance (approximately twofold) of daytime diuresis over nighttime.
In order to identify and subsequent specialized treatment of the pathology that is the cause of CND, instrumental methods are also used. Carrying out MRI of the brain, which has a number of advantages over other imaging methods, is necessary to exclude the organic nature of the disease, which accounts for approximately 40% of cases of CND. A distinctive feature is the absence of an image of the neurohypophysis or the visualization of a dimmer glow due to reduced ADH synthesis in the central form of the disease [30]. It should be remembered that the manifestation of CND, caused by pathology of the hypothalamic-pituitary region, can often be several years ahead of the identification of any formations in it. In this regard, regular MRI monitoring is necessary in patients with an unknown cause of the disease.