Perhaps everyone will agree that it is unpleasant to note a decrease in intelligence and difficulty remembering information among loved ones and relatives. And even more so, wild horror grips parents when they realize that something is wrong with the child. What to do when such disturbances begin in the functioning of the brain? We are talking about cognitive impairment - the inability to perceive, assimilate information, and come up with ideas.
The main thing is not to panic. Timely treatment of cognitive impairment allows one to achieve excellent results and stable remission. Thanks to modern medicine, adequate therapy can cope with the disease.
Why is it important to start treatment in a timely manner?
Cognitive impairment has three degrees of severity. In the initial stages they cause minor discomfort, but in the later stages they significantly worsen the quality of life.
- Mild violations. With mild cognitive impairment, concentration decreases, memory deteriorates slightly, and the patient quickly gets tired during certain types of intellectual activity.
- Moderate. Memory deteriorates more severely, and lapses may occur. Patients forget some events in life, the way home.
- Heavy. The patient cannot take care of himself, is disoriented in time, does not remember recent events, and forgets his home address. Sometimes patients suffer from hallucinations, delirium, and urinary incontinence.
To prevent the development of severe symptoms, it is important to consult a doctor promptly and begin treatment.
What is cognitive behavioral therapy and what are its benefits?
Cognitive-behavioral therapy (CBT) is a fairly common integrated area of psychotherapy that combines two approaches to the treatment of mental disorders - cognitive and behavioral psychotherapy. Also known as cognitive behavioral psychotherapy (CBT). Its distinctive feature is its short-term nature, focusing on correcting errors in thinking and behavioral skills, adapting emotional and behavioral reactions to the needs of the client and achieving success in performing social, professional, family, creative and other functions.
Cognitive psychotherapy for personality disorders is based on the principle of recognizing that their main cause is thinking errors in the form of illogical, inadequate and inappropriate beliefs that a person follows consciously or unconsciously. By changing incorrect thinking stereotypes to more functional and realistic ones, you can completely change a person’s worldview on his own inner world and attitude towards the reality around him. This is achieved by encouraging and consolidating positive thoughts and beliefs, as well as by denying unwanted, damaging forms of thinking.
Behavioral therapy focuses on correcting behavioral skills without delving deeply into the patient's mind and way of thinking. Teach a person to communicate correctly with others, avoid or painlessly resolve conflict situations, achieve goals, detect and eliminate harmful and inappropriate habits, etc. Cognitive-behavioral psychotherapy combines and enhances the therapeutic effects of both approaches, uses their techniques, and has clinically proven success in treating many mental disorders. A person can be taught a new line of behavior in certain situations, but only by changing his way of thinking, realizing the destructiveness of thoughts about his own insignificance, uselessness and inability to live, can a person radically change his destiny. Only a meaningful approach to one’s behavior is effective in any situation, and not just in those lost in behavioral psychotherapy sessions. But this is not the only advantage of CBT. Its advantages also include the following nuances: • Specification of circumstances. Like Gestalt therapy, CBT operates on the “here and now” principle. This means that the subject of consideration is not past mental trauma, but problems of the current time that a person is not able to resolve on his own. • Active work of the patient, who not only learns new skills, but also practices them in specific situations in order to use them in the future without seeking repeated help from a psychotherapist (what is the difference between a psychologist and a psychotherapist). • Fast therapeutic effect. Usually 5-10 sessions are enough to achieve a pronounced effect. • CBT has been proven effective in treating mental disorders in multiple clinical trials, which explains its growing popularity. The duration of CBT is determined purely individually and depends on the following factors: • The severity of the patient’s condition. • Set tasks. • The wishes of the patient himself. For some, 6-8 sessions are enough, while others feel the need to communicate with a cognitive psychotherapist for several months. And this does not indicate lack of effectiveness, but rather the comfort of the treatment process itself for the patient’s psyche. It should not be forgotten that the ultimate goal of CBT is to prepare a person to independently solve problems of various types, i.e. his “armament” with the emotions, thoughts, ways of behavior and communication necessary for personal development and success in life. What are the basic principles of CBT and how do they correlate with other areas of psychotherapy? As I already mentioned, cognitive behavioral therapy is a complex direction and therefore creatively combines the principles and techniques of its two components - behavioral and cognitive psychotherapy. From behavioral therapy, its basic principles were taken, based on the theory of behaviorism (translated from English as behavior). It assumes that human behavior is a set of unconditioned and conditioned reflexes developed on their basis, fixed or rejected by the individual’s individual history. The theoretical foundations of behaviorism were laid by Russian scientists S.M. Bekhterev. and Pavlov I.P., whom almost all well-known followers of behaviorism in the West consider their teacher. It is the principles of the formation and extinction of conditioned reflexes due to their reinforcement or non-reinforcement by unconditioned reflexes that formed the basis of the theory of behavioral psychotherapy. In addition, of fundamental importance in behaviorism and cognitive-behavioral psychology, respectively, is the concept of behavioral patterns that play a key role in the occurrence of many mental disorders. Patterns of behavior include, in stressful situations, certain vegetative-somatic and endocrine reactions that explain the development of psychosomatic disorders. In addition, the following postulates are of fundamental importance: • Use only methods that have proven their effectiveness in numerous experiments. • The relativity of the concept of normalcy and mental abnormalities. • Focus on developing optimal and desirable behavior for each individual patient. • Directiveness of the psychotherapist, which involves working according to a pre-developed scheme with answers to questions posed and performing recommended exercises with the inclusion of family members in homework. There are many methods of behavioral therapy, but in the practice of CBT the most recognized and widespread are the following: • Imitation of the desired behavior of a real person, a book or film character, or an invented symbolic model. • Role-playing training with training in certain behavioral skills under various problematic circumstances. For example, when communicating with a stranger or in conflict situations. Most often, the patient plays himself, but sometimes this role is played by a psychotherapist or another group member, which allows the patient to examine himself and his behavior as if from the outside and realize his mistakes. • Feedback, in which hardware monitoring of the patient’s stressful state is carried out and when a state of relaxation is achieved, it is reinforced with positive sound (favorite melody, sound of the sea, etc.) or visual images. • Psychological immunization, or stress-vaccination therapy, the main goal of which is psychological vaccination (sensitization) of the patient to face stressful situations of varying degrees of complexity. This allows you to move from a state of helplessness to self-control and the ability to successfully cope with stressful situations without their destructive consequences for the body and psyche. As for cognitive therapy, things are somewhat more complicated. To understand its basic principles included in CBT, one must first consider the goals and merits of cognitive therapy. Advantages of cognitive therapy: • The presence of a natural science base in the form of a psychological theory of normal development, as well as the occurrence of mental disorders. • Psychological models for each nosological group of mental pathologies. • Existence of own specific techniques and stages of treatment. • Relatively short course of therapy, including 20-30 sessions. • Humanistic orientation, putting the interests of the patient at the forefront. Among the main goals of cognitive therapy, which have been transferred to CBT, the following can be identified: • Help in solving the patient’s social, professional, family, career, creative and other problems. • Identifying and eliminating the causes of mental pathologies, in particular, correcting cognitive errors, eliminating dysfunctional beliefs and behaviors. • Partial or complete elimination of symptoms of mental disorders. • Reducing the likelihood of relapse. • Strengthening the therapeutic effect of pharmacological drugs. During the treatment process, a cognitive psychotherapist strives to achieve practical solutions to the following problems: • The patient’s awareness of the influence of his own thoughts on his behavior and emotional background. • The ability to identify, observe and evaluate so-called automatic thoughts. What it is? I'll tell you a little later. • Replacing erroneous mental attitudes with more rational and positive ones. • Identification and leveling of maladaptive beliefs as the basis of erroneous thoughts and behavioral reactions. As you can see, the complex merging of behavioral and cognitive therapy in CBT is completely justified and logical, because their common ultimate goal is improved socio-psychological adaptation to the conditions of the surrounding world and the achievement of harmony with oneself and the external environment.
How to diagnose and treat cognitive impairment
- We interview the patient, relatives, examine the patient and conduct neuropsychological tests to determine the condition and make a diagnosis.
- For initial forms of disorders, we prescribe a course of vitamins and amino acids.
- We prescribe neuroprotective drugs that improve cognitive functions, and drugs that affect the cause of the disorder and eliminate it.
- We organize classes with a psychologist and conduct trainings that help improve cognitive functions.
From cognitive impairment to dementia
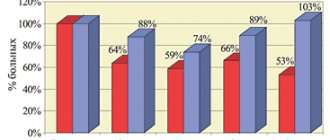
Recently, the problem of pre-dementia mild and moderate cognitive impairment has received increasing attention from doctors and researchers. Although mild and moderate cognitive impairment is not as severe a socioeconomic burden as dementia, the presence of even mild cognitive impairment significantly reduces the patient’s quality of life, and the risk of developing dementia among patients with moderate cognitive impairment is very high and amounts to up to 10-10% 15% per year. Therefore, an extremely important aspect for a neurologist is the diagnosis of cognitive impairment at pre-dementia stages with the goal of prescribing therapy as early as possible to prevent or delay the onset of dementia.
A brief excursion into the history of the Kyrgyz Republic
The criteria for vascular dementia were developed in the late 60s of the twentieth century, so in the pathogenesis of vascular CR, the leading role was given to multi-infarction brain damage, which distinguished neurodegenerative AD from vascular dementia. Subsequently, the presence of multiple large and small (lacunar) infarctions was identified as the cause of vascular dementia. Later, in addition to heart attacks, infarction in areas of the brain strategic for cognitive functions, non-stroke lesions of the white matter of the brain, cerebral hemorrhages, and states of cerebral hypoperfusion began to be identified as the cause of vascular dementia. In 1993, Hachinski et al. proposed the term “vascular cognitive impairment” - vascular cognitive disorders, to designate cognitive disorders that develop as part of cerebrovascular diseases.
The above criteria once again show how difficult it is to diagnose mild cognitive impairment, while MCI manifests itself and is diagnosed more clearly.
Diagnostic criteria for mild and moderate cognitive impairment
| Diagnostic criteria for mild cognitive impairment. Yakhno N.N., Zakharov V.V., Lokshina A.B., 2005. | Modified diagnostic criteria for MCI syndrome (MCl-Revised), J. Touchon, R. Petersen, 2004. |
| 1. Complaints about decreased memory or mental performance, expressed independently or with active questioning of a doctor. 2. Mild cognitive impairment, predominantly of a neurodynamic nature, identified during a neuropsychological study. 3. The absence of cognitive impairment according to the results of screening scales for dementia is the result of a mini-mental status scale of at least 28 points. 4. Stage 2 on the global deterioration rating (GDS). 5. Absence of disturbances in daily activity, including its most complex forms. | 1. Cognitive impairment, according to the patient and/or his immediate environment (the latter is preferable) 2. Signs of recent decline in cognitive abilities compared to the individual norm. 3. Objective evidence of cognitive impairment obtained using neuropsychological tests (a decrease in the results of neuropsychological tests by at least 1.5 standard deviations from the average age norm). 4. There are no disturbances in the patient’s usual forms of daily activity. However, there may be difficulties in complex activities. 5. There is no dementia - the result of the Mini Mental Status Assessment Scale is at least 24 points. |
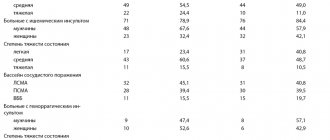
It should be noted that CR of varying severity are observed in the vast majority of patients (87%) who have suffered a stroke. Thus, a decrease in visual memory and attention predominates in patients with deep lesions in the right hemisphere of the brain, and a decrease in auditory-verbal memory predominates in patients with lesions in the left hemisphere
Today, due to various circumstances, mostly mild cognitive impairment and dementia are diagnosed in clinical practice. The syndrome of mild cognitive impairment (synonym: “mild cognitive decline syndrome”) requires special consideration.
MCI syndrome refers to impairments of memory and other higher functions in older people that go beyond the age norm (natural aging), but do not cause social maladaptation; at this stage of development it is difficult to attribute them to any nosological form.
Patients with MCI may experience:
- moderate decrease in the ability to concentrate;
- difficulties in simultaneous perception of several stimuli;
- memory impairment for current events, names of new acquaintances, geographical names;
- absent-mindedness, frequent searches for forgotten things.
Along with impaired memory and attention, at the pre-dementia stage there may be mild speech impairments, expressed in forgetting the names and surnames of loved ones, difficulties in choosing the right word, vocabulary depletion, and mild visual-spatial impairments (difficulty orienting in unfamiliar places). At the same time, patients remain completely critical of their condition; sometimes they even tend to exaggerate the cognitive impairments they have, which leads to severe anxiety and depression. MCI is often accompanied by fatigue, decreased mood and anxiety due to the awareness of one’s own inferiority.
ICD-10 offers the following criteria for diagnosing MCI:
- presence of decreased memory, attention and/or learning ability;
- subjective complaints of increased fatigue during mental work;
- lack of connection between cognitive impairment and confusion;
- absence of dementia;
- organic nature of cognitive disorders.
MCI syndrome occupies an intermediate position between changes in cognitive functions caused by aging and dementia, and can be classified as a pre-dementia stage.
From MCI to dementia
In the vast majority of cases, cognitive changes in MCI syndrome are progressive. The outcome of progression of MCI is dementia. According to the DSM-111-R manual (1987), dementia is defined as impairment of short-term and long-term memory, combined with disorders of abstract thinking, judgment and other higher functions of the body, as well as personality changes . All this quite seriously interferes with the patient’s professional activities, complicates normal social activity and contact with other people. Dementia is diagnosed only when intellectual-mnestic impairments are combined with a decrease or decay in the ability to perform professional and social activities.
Comparative characteristics of MCI and dementia:
| UKR | Dementia |
| Daily activities are not impaired (only the most complex activities are limited) | Patients “cannot cope with life” due to an intellectual defect and require outside help |
| Mini-Mental State Examination score usually below 24 | Mini-Mental State Examination score is often (but not always) below 24 |
| The course is variable: along with progression, long-term stabilization and spontaneous regression of the defect are possible | The cognitive defect is in most cases progressive, but sometimes has a stationary or reversible nature |
| Criticism is intact, violations are more disturbing to the patient himself | Criticism is reduced, violations worry the patient’s relatives more |
Benefits of treating cognitive impairment with us
- We select treatment individually
. We conduct an examination and collect a medical history. We take into account the state of health, the degree of cognitive impairment, and the presence of concomitant diseases when selecting treatment. - We use proven methods
. We use methods that have undergone clinical trials and have been approved by Russian and international institutes for the quality of medical care. - We accept after relatives apply
. We make an appointment, conduct an examination and begin treatment if relatives contact us and the patient himself does not admit that there is a problem.
We treat anonymously. We do not register with mental health clinics, we do not transmit information about the patient to state regulatory authorities or the employer. We store documents only in the clinic’s archives and maintain their confidentiality.
To consult with our doctor or make an appointment, call or use the feedback form.
Etiology
The main risk factor for the development of personality disorders with cognitive impairment is age. By the age of 65, almost 30% of patients who come for regular examinations to a therapist complain of a deterioration in intelligence. Risk factors include:
- hypertension: it has been proven that an increase in systemic blood pressure for every 10 mm Hg. increases the risk of intellectual dysfunction by 7–12%;
- coronary heart disease;
- arrhythmia;
- excess weight and physical inactivity;
- hyperlipidemia, atherosclerosis.
In addition, the causes of the syndrome may be:
- deficiency of vitamin B12, folic acid, thiamine;
- hepatic, uremic, discirculatory encephalopathy;
- endocrine pathologies: hypothyroidism, thyrotoxicosis, insulinoma (benign tumor that produces insulin);
- respiratory failure;
- alcohol or drug intoxication;
- autoimmune and systemic diseases, for example, lupus, sarcoidosis, vasculitis;
- some infections: neurosyphilis, HIV, neuroborelliosis, previous meningitis, encephalitis;
- hydrocephalus;
- brain tumors, aneurysms, surgical interventions;
- consequences of traumatic brain injury, stroke;
- depressive and anxiety disorders.
The listed diseases, although difficult, are treatable, and with the right treatment tactics it is possible to completely restore all intellectual processes. The prognosis is much worse if symptoms appear due to dementia or Alzheimer's disease. In such cases, only symptomatic treatment is possible.
How are CBT sessions conducted and what techniques are used?
Treatment with a cognitive psychotherapist takes place in the form of 1-2 sessions per week, the total number of which is 20-30 sessions. As I already said, it is very important before the first session that the patient first decides on the goals of psychotherapy. First of all, he must answer the following questions: • What does not suit you in your life, character, relationships and what specifically would you like to change - relationships in the family, work team, with the opposite sex, or maybe you want to find yourself in a new social role or bring back creativity? • What bad habits or addictions would you like to get rid of (for example, gambling addiction) and what useful skills would you like to acquire? All these problems need to be discussed with a psychotherapist at the first session, who will help to specify them and prioritize them. At the same time, he can offer the patient to undergo a series of tests to objectively assess his mental and moral state, the results of which, by comparison, can be used to monitor the effectiveness of the therapy, to determine its tactics and select the optimal CBT techniques in each specific case. The choice of CBT techniques and methods is huge. In addition to those borrowed from behavioral therapy, cognitive therapy techniques are widely used, namely: 1. To identify automatic thoughts: • Recording thoughts when performing necessary and not performing unnecessary actions. Moreover, this should happen in the order in which thoughts arise, which will make it possible to identify their priority in motivating the patient’s actions. Usually the first thought that comes to mind will be the most important. The main efforts of a cognitive psychotherapist should be directed at its correction. • Cognitive rehearsal, associated with the mental playback of negative situations and verbal voicing of emerging automatic thoughts. All results of the experiment are recorded in a separate diary of thoughts, which also records all the thoughts that arise in the patient over several days in order to identify the most significant ones. • Detachment is a kind of abstraction from one’s own thoughts and its objective assessment. Allows you to highlight and realize the spontaneity of bad thoughts, the automatic nature of their occurrence, inherent in previous negative experiences, as well as their non-adaptive nature, i.e. the ability to cause destructive negative emotions.
2. After identifying automatic thoughts, the most difficult work begins: changing them and correcting distortions. To do this, the following methods are used: • Argumentation and counterargumentation with writing down and repeatedly reading the arguments “for” and “against” when an automatic thought appears. With frequent reproduction, the human brain will remember useful arguments and remove “harmful” motives from quick memory. • Speaker technology. It consists of filling out a table with several columns - the first one records the problem, the 2nd - the accompanying feelings and emotions, the 3rd - the automatic thoughts that arise in this case, the 4th - the arguments for them, and the 5th - th – “against”. • Identifying the pros and cons of the problem in the short and long term. • Conducting experiments to test the correctness of judgments. For example, an offer to evaluate a situation without emotion or imagine how other people would react to it. • Discussing past events with witnesses, especially in situations with patients whose memory is distorted or replaced by fantasies, for example, in schizophrenia. The method is also relevant in case of misinterpretation of the behavior and motives of other people. • Imagination. This is especially true for anxious patients, in whom maladjustment is caused not so much by automatic thoughts as by obsessive images. A variety of techniques are used here, including metaphors, poems, parables for greater clarity, commands to oneself to “stop!”, replacing a negative image with a positive one, etc. • Replacement of emotions and revaluation of values. • Appeal to the experience of the psychotherapist himself, statistical data, fiction, etc. 3. At the next stage, they focus on identifying logical errors and contradictions in judgments. The following techniques are most often used here: • Graduality, or scaling, when extreme polarization of judgments using a scale is excluded, i.e. placing them according to the degree of objective reflection of reality. • Reattribution is a review of the patient’s measure of responsibility for his actions in a given situation, which is important for a correct assessment of one’s own contribution and external factors in the development of events. • Exaggeration – taking a certain belief of the patient to extremes or absurdity and thus encouraging it to be re-evaluated.
4. Assessing the likelihood of the worst case scenario allows you to narrow the time frame of the problem and reveal its true significance in the patient’s life: • Decentering, when the patient’s ideas that he is the center of everyone’s attention and that the whole world is aimed against him lead to a state of discomfort and provoke sociopathic thoughts. • Decatastrophization. It is used for various anxiety disorders and forces the patient to think about a realistic assessment of the consequences of the events that worry him. For example, if this does happen, what will happen - will your career be destroyed, or you will die, or your family will abandon you, or will all this last forever? The answers to these questions will allow a person to understand the transitory nature of the problem, and the automatic thought of its infinity will simply disappear. To consolidate the positive effect of CBT, it is important to use exercises such as: • Repetition - repeated repetition of the desired thinking and behavior in practice, and with the consolidation of positive emotions and thoughts. • Together with the psychotherapist, development of a plan for future actions, including conditions and deadlines for implementation, as well as the sequence of actions in the event of extreme or unforeseen situations. And this is not a complete list of techniques used in cognitive behavioral therapy, which are combined into blocks according to specific goals, stages of therapy, nosological forms of mental disorders, as well as the degree of their severity. You can imagine what a colossal arsenal of knowledge, experience and intuition a cognitive psychotherapist must have in order to select the optimal treatment regimen for the patient and adjust it depending on whether progress is achieved or not.