Fluifort is a pharmaceutical product for oral administration. Available in several dosage forms. It belongs to the group of mucolytics, and therefore has a pronounced expectorant and mucus-thinning effect. Intended for the treatment of diseases of the bronchopulmonary system. Widely prescribed for adults and children.
Composition and release form
The drug is presented in the form of granulated powder and syrup.
The granules have a pleasant citrus fruit aroma, are small in size and white in color. Packaged in sachets of 5 mg and a total cardboard package of 10 pieces.
The syrup has a liquid texture and a cherry smell. Sold in a glass bottle of 100 ml. The set includes a special measuring cup.
The active component is carbocisteine. Its content in granules is 2.7 g, in syrup 9 g.
Additional substances: flavorings, citric acid, mannitol, aspartame and orange juice in granular form. Also sucrose, pure water, cherry flavoring and caramel in syrup.
pharmachologic effect
Fluifort belongs to the group of mucolytic agents. Pharmacological activity is to improve the function of the enzyme on the mucous surface of the bronchi. Normalizes the content of acidic and neutral cells. Helps thin mucus in the sinuses and pulmonary system, leading to better clearance and suppression of cough syndrome.
In addition, it increases the regenerative ability of the mucous membrane, eliminates damage to its structure and stimulates the activity of the epithelium.
The drug helps increase the body's specific defenses and normalizes mucociliary clearance.
The components of the drug have high adsorption. The maximum therapeutic concentration of substances in the respiratory organs occurs after 2-3 hours and lasts up to 8 hours.
Excretion is carried out through the kidneys, mainly unchanged.
FLUIFORT (syrup)
spectrum of action.
Fluifort helps get rid of not only mucus in the lungs and bronchi, but also mucus in the nasopharynx and has a positive effect on the mucous membrane, restoring it. Manufacturer: Italy. Apparently, this is the reason for the high cost of this drug - about 300 rubles per 90 ml bottle.
This volume is quite sufficient for treating a child. But for adults, the recommended dose is 15 ml 2-3 times a day for 4 days; several bottles will be needed. It will be too expensive for an adult, but this is just an auxiliary mucolytic agent that is used in complex treatment.
The bottle is made of tinted glass, this is a minus - it can break.
The lid is quite difficult to open - it is childproof.
The set includes a measuring cup and instructions for use, unfortunately they have not been preserved.
I gave the syrup to the baby using a disposable syringe - it’s much more convenient to measure and take. Taken 30-40 minutes after meals, slightly diluted with boiled water.
The syrup is quite liquid and completely transparent. Quite sweet, but not cloying. After administration, there is no feeling of bitterness or other unpleasant aftertaste. The syrup has a very pleasant cherry aroma and taste.
The syringe dripped into the mouth gradually, drop by drop. The baby really liked the taste and took it with great pleasure. But a slight allergic reaction in the form of reddening of the cheeks was still observed.
Taking Fluifort should be accompanied by drinking plenty of fluids throughout the day.
Fluifort has an age limit of up to one year, but many doctors do not take this into account when prescribing and prescribe it to children of an earlier age, simply reducing the dosage. My then two-month-old baby was prescribed 1.5 ml three times a day.
Just a few days after the prescribed complex treatment, I noticed improvements, and a little more than a week later the baby began to breathe freely through his nose.
When the baby was 8 months old and the infectious disease was accompanied by wheezing and coughing, they were treated with a completely different syrup, which has not only a mucolytic but also an anti-inflammatory effect, review here - An effective analogue of Erespal, which did an excellent job in complex treatment.
But since babies cannot cough up on their own due to age, the liquefied sputum does not come out, the baby pushes it back and forth. It is necessary to additionally combine the technique with a drainage massage or with pressure on the root of the tongue so that the mucus comes out.
In order to finally cope with the residual symptoms of a cold in the form of slight wheezing, at first the doctor again wanted to prescribe Fluifort for us. I reported that I had an allergy to it in the form of diathesis and reminded that it is allowed only from the age of one year. She asked, if possible, to replace it with a less toxic and more age-appropriate product. The doctor wrote out a prescription for a free expectorant syrup, which turned out to be no less effective and perfectly helped to completely cope with the cough, review here - Bromhexine Pharmstandard. I suspect that doctors are simply trying to prescribe free medications less often, so as not to write out prescriptions again and to protect themselves from unnecessary work. But even without a free prescription, the cost of Bromhexine Pharmstandard would have cost me several times less than Fluifort, while also being an effective mucolytic agent.
As a summary, Fluifort syrup is effective, but the price is too high. It has a number of contraindications, age restrictions and can cause allergies. To treat an adult, you will need several bottles and high costs. And for a child under one year old, there are cheaper and no less effective means that are allowed for children from birth!
I will be glad if my review is useful to you! Health to you and your children!
What is Fluifort powder and syrup for?
The main indications for prescribing the drug are diseases of the ENT organs and bronchopulmonary apparatus. Fluifort is effective in acute and chronic cases, when a viscous, difficult-to-separate secretion is formed.
Pathological conditions for which the drug is used:
- Bronchitis.
- Tracheitis, tracheobronchitis.
- Bronchial asthma.
- Rhinitis.
- Sinusitis.
- Otitis.
- Bronchiectasis.
- Adenoiditis.
The drug is also prescribed to patients before diagnostic procedures of the respiratory system.
Otitis media in children: advice from an otolaryngologist
11.12.2020
Otitis media , according to the latest international trends, is a pathology of the auditory tube. Continuation of the infection that occurs in the nasopharynx, as a rule, already enters the middle ear . Normally, the nasopharynx is connected to the middle ear using the auditory tube; in children, this tube is very short, and infection can enter from the nasopharynx through it when children blow strongly through their nose or through the migration of microorganisms.
The occurrence of otitis in children most often begins with a virus, and then some bacterial flora is added. Modern therapy for otitis media very clearly sets the line between where to immediately use antibiotics and where to observe. Taking into account the trends in the world that antibiotics are not prescribed simply and in order to keep strains of microorganisms resistant to antibiotics under control, antibacterial therapy
According to statistics, up to 80% of otitis media end without antibiotics. And only 20% need antibiotic therapy immediately.
The use of antibiotics is categorical in two cases: the child is under 2 years of age and the severity of the disease (temperature more than 38°C, severe pain, etc.). In such cases, an antibiotic is prescribed immediately. By agreement of the parties and provided that the child can be shown to a doctor , the process of prescribing antibiotics is postponed for about a day or two.
If, for example, the child becomes worse within a day or the condition has not changed, only then antibiotics are prescribed. As a rule, vasoconstrictor drops in the nose , anti-inflammatory drugs that suppress inflammation in the nasopharynx and middle ear , anti-inflammatory drops in the ear , which relieve pain and have an anti-inflammatory effect on the eardrum.
Main symptoms
Young children rub their ears and do not allow them to touch them. The fact is that in childhood, a full-fledged external auditory canal is not formed, so when pressing on the tragus, very severe pain occurs, which is no longer the case in adults. The temperature can be either critical (under 38°C) or low-grade. Temperature is the body’s ability to respond in one form or another to an infection. Some people's body reacts hyper-reactively, there may be a high temperature, while others, on the contrary, are hypo-reactive.
Who is at risk?
These are children who have chronic problems with the nasopharynx: adenoiditis, constant runny nose . In these children, otitis occurs more often.
In order to clearly understand whether otitis media , you need to do a blood . And so, in principle, the most important thing is to examine the child.
What complications can there be if left untreated or undertreated?
These are intracranial complications: brain , mastoiditis, which can even lead to death. A rupture of the eardrum may occur. Although it is believed that this is not a categorical complication, it is better not to lead to it. Even in cases where there is already a protrusion due to purulent otitis media , it is better to open it, remove the compression, and then the membrane will heal better.
Prevention
You need to keep your nose in order. If you have a runny nose, you should always use saline nasal . The first thing parents should know is not to use vasoconstrictor drops for a very long time and monitor the condition of the nasopharynx.
How to alleviate a child’s condition at home?
Give pain medication according to the child's age. You can put medicines in your ear to numb the eardrum. You should absolutely not heat it, because there are different stages of otitis media . In some cases, heating is strictly prohibited. The use of folk remedies for acute otitis media is inappropriate.
You need to watch how the child “blows out” his nose . You should teach how to blow your nose : first one nostril is blown out, and then the other. If a child does not know how to blow, most often the child himself inflates his ear infection . Strong blowing provokes infection through the auditory tube into the middle ear . You can use aspirators, they come in different types. When using an aspirator, you must first thin the mucus with saline sprays and then remove it from the nasal passages. For younger children, parents should supervise this.
It is necessary to monitor the child’s condition, the condition of the nasopharynx, seek help from a doctor and not self-medicate.
Published in Otorhinolaryngology Premium Clinic
Contraindications
The medication should not be used if there is an individual intolerance to the medicinal substances in its composition.
The product is contraindicated for people with diabetes mellitus, since it contains sucrose, for pregnant women and people with impaired renal function.
Fluifort is not prescribed for phenylketonuria or ulcerative lesions of the gastrointestinal tract. Also, syrup is not given to children under one year of age, and granules are not prescribed to those under 16 years of age.
Fluifort should be used with caution when breastfeeding, the elderly, and when the drug is combined with certain pharmacological groups.
Exudative otitis media (EO) is one of the most pressing problems in pediatric otorhinolaryngology. The prevalence of ESO in preschool children, according to some data, reaches 12.9% [1]. 90% of preschool children experience at least one episode of ESO [2]. Despite the fact that in most cases, ESO episodes end in self-recovery, in 30-40% of patients the process tends to recur, and in 5-10% of cases the process lasts more than a year [3]. Based on the tendency of ESO to self-resolve, the starting method of treatment is watchful waiting for 3-18 months [3, 4]. If there is no effect from watchful waiting, in most cases, according to some national recommendations, a decision is made on surgical treatment - tympanostomy. But, unfortunately, the effectiveness of this surgical intervention does not exceed 20-50% [3,4]. Considering the fairly high risk of negative results from both expectant treatment and surgical interventions, in recent years much attention has been paid to the study of various approaches to drug therapy for exudative otitis media in children. The main directions of drug treatment for ESO are anti-inflammatory therapy and the use of mucoactive drugs.
One of the most interesting classes of mucoactive agents are drugs based on carbocysteine, which regulate the production of secretions by glandular cells (mucoregulators), acting directly on the glandular cell and normalizing its secretory function, regardless of the initial state. The addition of lysine to the carbocisteine molecule (Fluifort) improves the tolerability of the drug, as its pH increases and, therefore, adverse events from the gastrointestinal tract are minimized. Fluifort has a so-called “aftereffect” effect, which is confirmed by the normalization of the viscosity and elasticity of secretions and mucociliary transport within 8 days after a 4-day course of therapy [5].
It has been proven that with the simultaneous use of carbocisteine and amoxicillin during exacerbation of chronic bronchitis, the content of the antibiotic in the bronchoalveolar lavage fluid increases significantly [6]. Similar data on synergism with antibiotics were obtained with the use of carbocysteine lysine salt, which significantly increases the level of bacterial eradication and the rate of recovery [7].
The most effective anti-inflammatory therapy today is intranasal glucocorticosteroids (InGCS). Thus, numerous studies have proven the high clinical effect of using mometasone furoate nasal spray in the treatment of adenoiditis in children, which is often the cause of the development of ESO [8-11]. However, further clinical studies examining the effectiveness of InGCS monotherapy in the treatment of ESO gave conflicting results [12, 13]. The use of mucoregulatory drugs, in particular carbocisteine, which, in addition to the mucoregulatory effect, has an anti-inflammatory effect, as monotherapy for ESO, almost doubled the likelihood of drainage of exudate from the middle ear compared to the group receiving placebo [14, 15]. Thus, the currently available rather scarce information on the effectiveness of carbocysteine in the treatment of ESO requires further clinical research on this issue. There is also no information in the literature about the effectiveness of the combination of carbocisteine and InGCS in the treatment of ESO in children.
At the Department of Pediatric Otorhinolaryngology of the Russian Medical Academy of Postgraduate Education, an open randomized comparative study was conducted, the purpose of which was to increase the effectiveness of drug therapy for exudative otitis media in children with recurrent and chronic adenoiditis.
Patients and methods
The study included 150 children aged 2 to 9 years with ESO, with clinical and anamnestic signs of often recurrent or chronic adenoiditis. All patients were combined into three groups. The 1st group consisted of 50 patients who, in addition to irrigation-elimination therapy (intranasal microdiffuse irrigation of the nasal cavity with isotonic saline solution 2 times a day, followed by toileting of the nasal cavity), received orally the drug carbocisteine lysine salt (Fluifort) in the form of syrup in an age-specific dosage for 8 weeks Group 2 - 50 patients who received treatment similar to patients in group 1 + intranasal spray of mometasone furoate 100 mcg/day once for 8 weeks. Group 3 (control) - 50 patients who received only irrigation-elimination therapy.
Exclusion criteria from the study were duration of ESO of more than 18 months; a history of data on the ineffectiveness of courses of drug therapy for exudative otitis media using carbocisteine drugs and/or InGCS; children - carriers of tympanostomy shunts; hypertrophy of adenoid vegetations of the third degree, complicated by obstructive sleep apnea syndrome; clinically confirmed primary and secondary immunodeficiencies, cancer; deviated nasal septum or pathology of the turbinates, accompanied by persistent difficulty in nasal breathing; chronic rhinosinusitis with polyps; the child has the conditions specified in the “contraindications” section in the annotation of the drug carbocysteine lysine salt and/or mometasone furoate nasal spray; disagreement of official patient representatives with the proposed treatment regimen; patient non-compliance with the study (at the discretion of the investigator).
The effectiveness of treatment was assessed on the basis of a 10-point visual analogue scale filled out by official representatives of patients, reflecting the dynamics of nasal congestion, nasal discharge and cough, as well as on the basis of tympanometry data. A follow-up examination of the patient was carried out on the 14th (±2), 56th (±5) and 84th (±7) days from the start of treatment. The analysis of side effects associated with the use of the drug carbocysteine lysine salt and mometasone furoate nasal spray was carried out retrospectively at a follow-up examination.
Statistical processing of the results was carried out using the Statistica v.6.0 program. To compare quantitative characteristics, Student's t-test was used, and to compare qualitative characteristics, Pearson's &khgr;2 test was used. The difference was considered statistically significant at p<0.05.
Results and discussion
During dynamic observation, due to non-compliance with the prescription of the supervising physician (failure to appear for follow-up examinations), 7 patients from group 1, 4 from group 2 and 5 from the control group were excluded from the study.
At the initial examination, according to the visual analogue scale, patients of the 1st, 2nd and control groups of the study did not have a statistically significant difference between the main symptoms of the disease (p>0.05) (see Fig. 1-3).
Figure 1. Dynamics of the severity of difficulty in nasal breathing.
Figure 2. Dynamics of the severity of nasal discharge (rhinorrhea).
Figure 3. Dynamics of cough severity.
On the 14th day from the start of treatment, according to VAS, the severity of nasal breathing dysfunction was the least in patients of the 2nd group of the study and amounted to 3.0±0.4 points, which was significantly less (p<0.05) compared to the data indicator in the 1st (4.2±0.4 points) and control (5.6±0.6 points) groups. Moreover, the difference between the indicators was statistically insignificant (p>0.05). Similar data were obtained when analyzing VAS data on the severity of cough and nasal discharge. Thus, the severity of rhinorrhea in patients of the 2nd group was 2.2±0.3 points, which had a significant difference (p<0.05) compared with the indicators of patients of the 1st group (3.8±0.5 points ), and the control group (4.5±0.6 points). The severity of cough on the 14th day from the start of treatment in patients of the 1st group was 5.8±0.5 points, in the 2nd group - 3.2±0.5 points, in the control group - 6.6±0, 6 points. As with other symptoms, the difference in indicators in patients of group 2 compared with patients of group 1 and control was statistically significant (p<0.05). At the same time, the severity of both cough and nasal discharge in patients of groups 1 and 3 was significant, but did not reach a statistically significant difference (p>0.05).
When analyzing VAS scores 8 weeks after the start of treatment, the severity of difficulty in nasal breathing was 2.7±0.5; 1.8±0.4 and 5.2±0.9 points in the 1st, 2nd and control groups, respectively. At the same time, a statistically significant difference (p<0.05) was established between VAS scores in patients of the 1st and control groups, as well as between the 2nd and control groups. The difference in VAS values between patients of groups 1 and 2 was statistically insignificant (p>0.05). The severity of nasal discharge was the least in patients of group 2 - 0.6±0.1 points. In patients of group 1, this indicator was 2.0±0.5 points, in the control group - 4.0±0.5 points. A statistically significant difference (p<0.05) was established both between VAS scores in groups 2 and 1, and between groups 1 and control. A similar statistically significant difference (p<0.05) was obtained according to the VAS data, reflecting the severity of cough in patients of the study groups: in group 1 - 2.8±0.6 points; in the 2nd - 1.2±0.4 points; in the control - 5.5±0.5 points.
When analyzing VAS scores 12 weeks after the initial visit, the severity of difficulty in nasal breathing was 3.2±0.5; 2.6±0.8 and 5.5±0.8 points in the 1st, 2nd and control groups, respectively. At the same time, a statistically significant difference (p<0.05) was established between VAS scores in patients of the 1st and 2nd groups, as well as between the 1st and control groups. The severity of nasal discharge was 1.8±0.4; 1.0±0.4 and 3.6±0.5 points in the 1st, 2nd and control groups, respectively. A statistically significant difference (p<0.05) was established between VAS scores in patients of the 1st and control groups, as well as between the 2nd and control groups. The difference in VAS values between patients of groups 1 and 2 was statistically insignificant (p>0.05). In the same way, a significant difference (p<0.05) was revealed in VAS scores reflecting the severity of cough in patients of all study groups. In group 1, this indicator was 3.2±0.5 points; in the 2nd - 2.5±0.4 points; in the control group - 5.7±0.6 points.
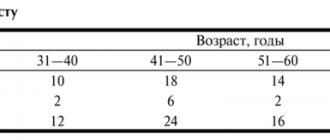
According to tympanometry data, all patients who completed the study were diagnosed with unilateral or bilateral exudative otitis media during the initial examination (see table).
When examined 14 days after the start of treatment, complete bilateral normalization of the function of the auditory tube and the condition of the middle ear cavity (tympanogram type A) was noted in 7 (16.3%) patients of the 1st group, in 21 (45.7%) patients of the 2nd group. th group and only in 4 (8.9%) patients in the control group. At a follow-up examination 8 weeks after the start of therapy, the best indicators of complete resolution of tubular dysfunction were also noted in children of the 2nd group of the study, where bilateral type A on tympanometry was obtained in 25 (54.3%) cases. This figure was slightly lower in patients of group 1 - 19 (44.2%) people. In the control group, complete resolution of tubular dysfunction was observed in only 14 (31.1%) patients. Tympanometry results at the final visit revealed similar results. Thus, complete resolution of tubular dysfunction was noted in 21 (48.8%), 24 (52.2%) and 14 (31.1%) patients in the 1st, 2nd and control groups, respectively.
When interviewing parents of patients at the final visit, satisfaction with the child’s condition was expressed in 40 (93%) cases in the 1st group of the study, in 44 (95.7%) cases in the 2nd group and only in 27 (60%) in the control group .
During the dynamic study, no clinical signs of acute bacterial rhinosinusitis were identified in any patient of groups 1 and 2. Only 1 patient in the control group was diagnosed at the final visit with acute bacterial rhinosinusitis, which required dynamic observation by an otolaryngologist and treatment according to generally accepted standards. The development of acute otitis media (complaints of ear pain) against the background of ARVI was noted in 1 patient in the 1st and 2nd study groups and in 3 in the control group. In all cases, there were no indications for systemic antibacterial therapy; patients received only symptomatic treatment.
None of the patients in groups 1 and 2 who completed the study developed undesirable side effects associated with the use of the drug carbocisteine lysine salt and/or mometasone furoate.
conclusions
Based on the results of the study, we can conclude that the use of the drug carbocisteine lysine salt (Fluifort) in the treatment of exudative otitis media in children with recurrent and chronic adenoiditis is a more effective treatment method compared to expectant management, which is consistent with the available literature data. The use of the drug carbocysteine lysine salt in combination with mometasone furoate nasal spray allows for faster relief of symptoms of adenoiditis and significantly accelerates the resolution of exudative otitis media compared to a monotherapeutic approach. The use of the drug carbocisteine lysine salt is a safe treatment method with an extremely low risk of developing unwanted side effects.
Side effects
As a result of a course of therapy with a mucolytic drug, the following side effects may occur:
- Dizziness and intense headaches.
- Malaise, fatigue.
- Allergic reactions - itching, hyperemia and skin rashes. Rarely - urticaria.
- Dyspeptic disorders - abnormal stool, heaviness in the abdomen, flatulence, pain in the epigastric region, nausea. Rarely - vomiting and symptoms of gastritis.
If side effects develop, symptomatic treatment is prescribed. Often, the above symptoms disappear on their own after stopping the medication.