About the work of human sweat glands
Sweating controls the external and internal body temperature. Sweat glands protect the body from overheating and help remove toxins from the body: their normal functioning is extremely important for health. Diseases of the internal organs can cause dysfunction of the sweat glands and pathologies of the eccrine and apocrine centers.
Hyperhidrosis, dyshidrosis, red stippling, anhidrosis, and miliaria are associated with disturbances in the functioning of the eccrine sweat glands, and bromhidrosis, osmidrosis, chromhidrosis, hidradenitis, and inverse acne are associated with apocrine ones.
Surgeons, dermatologists and cosmetologists diagnose and treat diseases of the sweat secretion centers.
The structure of sweat glands
Sweat glands are tubular channels: their number is more than 2-3 million!
They are located in the epithelium of the skin. Sweat accumulates in the secretory section and then comes to the surface. We all know where it usually appears - in the armpits, on the soles of the feet, protruding on the forehead, palms, groin, etc. There are no sweat glands on the lips and in some areas of the genitals.
- Anatomy of the sweat gland or its structure:
- The body is a spiral-shaped tube for collecting secretions.
- Output channel.
- Pores.
Sweat glands are surrounded by a network of nerve receptors: this explains the active secretion of sweat during hot weather, hormonal surges, stressful and extreme situations.
By the way, sweating in men is much more intense than in women.
Sweat centers
Eccrine sweat glands are constantly working, even if we don’t notice it. They are found in greatest numbers in the chest, armpits, back, face, palms and feet. The main function of the eccrine glands is thermoregulation.
There are fewer apocrine sweat glands in humans than eccrine ones. They begin their work at the age of 14, connected to the hair follicles. The main locations are the armpits, groin area, and breast areolas. It is these glands that are responsible for the appearance of each person’s individual scent, protect the skin from drying out, and increase its elasticity.
Sweat gland diseases
- Chromhidrosis - colored sweat.
- Uridrosis is an increase in the concentration of urea and its acid in sweat (often associated with kidney disease).
- Steathidrosis – oily sweat.
- Hypohidrosis – low level of sweating.
- Anhidrosis is a complete absence of sweating.
- Hyperhidrosis is increased sweating, which can be local or general.
- Hidradenitis is inflammation of the sweat glands with suppuration.
- Osmidrosis is an unpleasant odor of sweat.
- Miliaria is a rash on the skin in the form of small blisters with liquid contents.
Symptoms of diseases associated with sweating
Please note: if you have any rashes on your body, nodules in places where sweating occurs, its intensity increases, it begins to take on any color and has an unpleasant odor, consult a doctor (dermatologist, surgeon). He will conduct the necessary examination, if necessary, determine the cause of the condition and prescribe treatment. These could be medications, herbs, cosmetic procedures, etc.
- General recommendations for the duration of therapy (after approval from the attending physician):
- Careful hygiene: shower several times a day using antibacterial soap.
- Using antiperspirant (not to be confused with deodorant).
- Wearing clothes and underwear made from natural fabrics, change as needed.
- Avoid stressful conditions.
- Healthy sleep, rest, nutrition. Eliminate junk food, alcohol, and quit smoking from your diet.
Treatment methods for hyperhidrosis
Excessive sweating can be corrected: no need to worry! Today there are a lot of methods - conservative, cosmetic and surgical. They allow you to forget about the problem that bothers you for a long time. Special antiperspirants are often used, and they really help. But in some cases they do not change the situation globally.
One of the most popular cosmetic methods of combating active sweat production is botulinum therapy. Botox injections allow you to forget about the problem of wet armpits, feet and other parts of the body for a period of several months to a year.
A more invasive technique is curettage: the sweat glands are surgically scraped out. This mini-operation can be prescribed when other methods do not bring the desired result.
Structure and functions of the sebaceous glands
Sebaceous glands are derivatives or appendages of the skin. They were first described by the anatomist Malpighi in 1689. They are located on almost all areas of the skin, with the exception of the palms, soles and dorsum of the feet. In the overwhelming majority, the ducts of the sebaceous glands open into the mouths of the hair follicles of long, bristly or vellus hair. In this case, the sebaceous gland itself is located at the root of the hair on the border of the reticular and papillary layers of the dermis . In addition, the sebaceous glands are located isolated on the following areas of the skin: the area of the nose, forehead, chin, corners of the eyes, edges of the eyelids (glands of the cartilaginous edge of the eyelids - meibomian glands), the red border of the lips, the place where the skin meets the nasal mucosa, the lower third of the rectum intestines, skin of the nipples and periareolar region of the mammary glands, glans penis and inner layer of the foreskin (tysonian glands), as well as on the labia minora and clitoris.
The number of sebaceous glands on different parts of the body surface is not the same. For example, there are few of them in the area of the back of the hands, the skin of the legs and on the red border of the lips. On the contrary, in the area of the forehead, eyebrows, nasolabial triangle, chin (the so-called T-zone), on the scalp, as well as in the area of the ears, midline of the chest and in the interscapular area of the back, the number of sebaceous glands is large and reaches 400-900 per square centimeter. It is these places of large accumulation of sebaceous glands that are affected by seborrhea, a condition in which the secretion of sebum is increased. A large number of sebaceous glands are also present in the armpits, perianally and perigenitally. There they are anatomically connected not only with hair follicles, but also with apocrine sweat glands. Therefore, when they are blocked and inflamed, one of the severe forms of acne occurs - hidradenitis suppurativa, or inverse acne. These areas with a large number of sebaceous glands are usually called seborrheic.
The sebaceous glands are classified as simple alveolar glands with branched terminal sections and excretory ducts. The terminal sections are formed by several alveoli (sacs, lobules, acini), consisting of multilayered epithelium, which contains two types of cells: basal cells and sebocytes. Basal cells lie on the basement membrane and form the peripheral, or germinal layer of the terminal part of the gland. Sebocytes migrate from the basal layer and differentiate. These cells perform a secretory function; lipids accumulate in them in the form of large inclusions; Subsequently, the sebocytes are displaced in the direction of the gland duct, disintegrate and turn into a secretion - sebum. The type of secretion in which the lipid-producing cell completely dies and a gland secretion is formed is called holocrine, or holocrine. Consequently, the sebaceous glands are typical representatives of the holocrine type of secretion. Each terminal section has its own excretory duct, which are combined into a common one; it exits into the hair follicle. The wide and short common excretory duct is lined with stratified squamous keratinizing epithelium.
Sebaceous follicles and separately located sebaceous glands are abundantly supplied with blood from the superficial and deep dermal plexuses. This circumstance is important, since various metabolic products are released with the secretion of the sebaceous glands, as well as toxic and some medicinal substances (for example, preparations of iodine, chlorine, bromine, etc.) coming from the blood.
The innervation of the sebaceous glands is carried out by a complex nerve plexus surrounding the sebaceous glands, hair follicles, and sweat glands. These plexuses include fibers of the autonomic nervous system.
In different areas of the skin, the sebaceous glands are of different sizes. Typically, the smallest sebaceous glands are associated with long hair follicles, and the large and multilobed ones are associated with vellus follicles. Multilobular sebaceous glands in seborrheic areas are significant. They are quite large in size on the pubis, in the area of the labia majora, and also along the suture line on the skin of the penis. The skin of the legs, forearms and dorsum of the hands is equipped with small mono- or bilobed sebaceous glands. That is why the skin in these places is most often characterized by increased dryness.
During life, the sebaceous glands change their size. Thus, they are relatively large immediately after birth and in the first months of the child’s life, and then decrease. A sharp increase in the size of the sebaceous glands occurs with the onset of puberty. The sebaceous glands reach their greatest size by the age of 18-35. In old age, they atrophy to a large extent, so one of the signs of skin aging is its increasing dryness. It is also known that in girls, increased sebum secretion begins earlier than in boys. Subsequently, women experience a slowdown in the rate of sebum secretion throughout their lives, but this persists longer than in men.
The sebaceous glands secrete a complex secretion called sebum. On average, an adult produces about 20 grams of sebum per day. The secretion of the sebaceous glands onto the surface of the skin is facilitated by the contraction of the smooth muscle that lifts the hair. And the hair itself is also covered with a thin water-lipid film.
Sebum, secreted from the secretory section of the sebaceous glands, fills their excretory ducts, the mouths of hair follicles and is gradually distributed along the grooves of the skin, covering the entire surface of the skin with a layer 7-10 microns thick. At the same time, the secretion of the sweat glands reaches the surface of the skin; at the same time it mixes with sebum and emulsifies. Thus, a continuous, thin water-fat emulsion film, called the water-lipid mantle, is formed on the surface of the body. The composition of the water-lipid mantle also includes ceramides of the stratum corneum (see below). Emulsification of sebum occurs due to hydrophilic high molecular weight aliphatic alcohols and cholesterol included in its composition. Depending on the ratio of sebum and sweat on the skin, the resulting water-fat emulsion may contain more fat (water-in-oil type) or more water (oil-in-water type). So, for example, at high ambient temperatures and increased sweating, an “oil in water” emulsion is formed on the skin, and at low temperatures and slight sweating, an “water in oil” type emulsion is formed. In seborrheic areas, a water-in-oil emulsion is formed at higher temperatures.
In terms of its chemical composition, sebum is a mixture of lipids. It consists mainly of free and bound (esterified) fatty acids. In addition, small amounts of hydrocarbons, polyhydric alcohols, glycerol, cholesterol and its esters, wax esters, squalene, phospholipids, carotene, as well as metabolites of steroid hormones are found in sebum. Among free fatty acids, all fatty acids with a number of carbon atoms from 1 to 22 are found. These include higher and lower fatty acids, saturated and unsaturated, with a straight and branched chain of carbon atoms.
The main part of free fatty acids consists of higher fatty acids and their homologues with 14 (myristic), 16 (palmitic) and 18 (saturated - stearic and unsaturated - oleic) carbon atoms in the chain. Water-soluble lower fatty acids (formic, acetic, propionic, butyric, valeric, capronic, enanthic, pelargonic, capric and undecylenic) and their homologues are contained in sebum in small quantities. It is known that the content of free higher fatty acids is 25% relative to the weight of sebum, and free lower fatty acids are only 5.5%. It should also be emphasized that free lower fatty acids with the number of carbon atoms from 1 to 13 have fungicidal, bactericidal and virusostatic properties, thereby performing the function of a kind of “biological brake” in the protective system of the skin surface.
The skin as a unique structure is rightly compared by many authors to a brick wall, where the role of “bricks” is played by corneocytes (postcellular structures of the stratum corneum), and the “cement” is played by highly specialized and uniquely organized intercellular lipids. Such lipids include ceramides (from the English ceramides), cholesterol, fatty acids, as well as phospholipids, glycosylceramides, free sphingoid bases and cholesterol sulfate. These lipids form the main barrier to water, thereby preventing transepidermal water loss (TEWL). They also play the role of a special intercellular cementing substance, which provides adhesion strength to the postcellular structures of the stratum corneum and ensures the integrity of the skin. It is now known that in the stratum corneum of the epidermis there are six main classes of so-called “free”, not associated with corneocytes, ceramides and two main classes of ceramides covalently associated with the surface of corneocytes (classes A and B). The composition of ceramides in the stratum corneum of the skin in humans is highly variable and depends on race, concomitant medical diseases, age, environment and a number of other factors. Ceramides have a rather complex chemical structure. Most are long chains of sphingoid base with 16 to 22 carbon atoms; less commonly, they are represented by dihydrosphingosine, phytosphingosine and 6-hydroxysphingosine. Sphingoid bases are combined with various fatty acids (oleic, linoleic, etc.), including free lower fatty acids, which perform a number of important biological functions. The functions of ceramides include not only the retention of water in the skin, but also the regulation of the rate of desquamation, as well as the influence on the differentiation of keratinocytes. It has been shown that sphingosine is able to regulate the rate of renewal of the epithelial layer, preventing its rapid change without normal differentiation of keratinocytes.
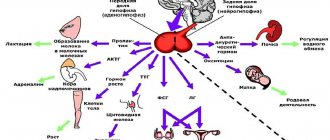
Sebum secretion is regulated mainly by hormonal and to a lesser extent neurogenic mechanisms.
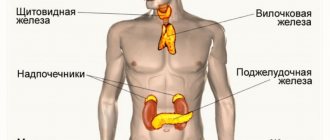
Hormonal regulation of sebum secretion is carried out through androgens, namely testosterone, which is the main hormone that enhances sebum secretion. It is for this sex hormone that there are receptors on the membrane of sebocyte cells. Interacting with the receptor on the surface of the cell that produces sebum, testosterone under the action of the enzyme 5-a-reductase is converted into its active metabolite - dehydrotestosterone, which directly increases secretion production. It has been proven that sebaceous glands of different locations have different numbers of testosterone receptors. This explains the fact that in a number of patients certain areas are often affected, for example, only the skin in the chin area or only the skin of the back, etc. The amount of biologically active androgen, as well as the sensitivity of sebocyte receptors to it, and the activity of 5-a-reductase, which determine the rate of secretion of the sebaceous glands, are genetically determined. In general, hormonal regulation of sebum secretion can be carried out at four levels: the hypothalamus, pituitary gland, adrenal cortex and gonads.
Hormones that suppress sebum secretion include estrogens, since their predominance leads to a decrease in the effect of androgens. However, the effect of estrogens that suppresses sebum secretion is much less pronounced than the effect of androgens, which stimulate sebum secretion.
As for the neurogenic regulation of secretion, it is mainly carried out by the autonomic nervous system. Increased sebum secretion is found in individuals with vagotonia; At the same time, other symptoms of increased vagal tone may appear - sharply increased sweating, persistent red dermographism, acrocyanosis. A change in the tone of the autonomic nervous system, which innervates the muscles that lift the hair, leads to a more rapid emptying of sebum from the sebaceous glands associated with the hair follicle. It is believed that not only the autonomic nervous system influences the secretion of sebum. It is also known that sebum secretion clearly increases with various lesions of the cerebral cortex (stroke) or with certain subcortical disorders in encephalitis, parkinsonism, diencephalic disorders, as well as with damage to peripheral nerves. Significant disturbances in sebum secretion also occur in patients with mental illnesses such as schizophrenia, manic-depressive and infectious psychoses, epilepsy, and various depressive states. Apparently, in all of these conditions, changes in the release of hormones from the pituitary gland and hypothalamus and an indirect effect on testosterone levels are more significant.
In conclusion, the biological role of the sebaceous glands should be emphasized. First of all, the sebaceous glands secrete sebum, which is part of the water-lipid mantle of the skin. The water-lipid emulsion formed on the surface of the skin has the following effects:
- Gives elasticity to the skin and prevents it from drying out.
- Regulates the rate of desquamation and differentiation of keratinocytes.
- Helps maintain a constant body temperature due to changes in the physical composition of the water-lipid mantle.
- Neutralizes alkalis that reach the skin surface with organic fatty acids and maintains a constant slightly acidic pH (4.5-5.5).
- Suppresses the proliferation of bacteria, fungi, viruses thanks to free lower fatty acids and some other substances that are part of sebum, sweat and the stratum corneum.
- It is one of the ways of excretion of various metabolic products, as well as medicinal and toxic substances.
Hyperhidrosis
Diabetes
Climax
Menopause
14293 December 16
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Hyperhidrosis: causes of occurrence, what diseases it occurs with, diagnosis and treatment methods.
Definition
Hyperhidrosis is excessive sweating that occurs from time to time or is constantly present. There are from two to five million sweat glands on the human body - most of all in the armpits, on the palms, and feet.
Sweating is a physiological process necessary to maintain body temperature.
However, there are a number of conditions in which sweat begins to be released too intensely, which indicates certain dysfunctions and brings significant physical and psychological discomfort to a person. According to statistics, about 3% of people of both sexes complain of hyperhidrosis.
Sweating is controlled by the autonomic nervous system, of which the parasympathetic nervous system is a part; a malfunction in its functioning can be either a consequence of other diseases or an independent disorder.
Types of hyperhidrosis
By localization:
- Local hyperhidrosis - occurs in certain parts of the body - on the palms, soles, armpits, skin folds, on the forehead, above the upper lip.
- Generalized – increased sweating is observed over the entire surface of the body, but is most noticeable in places where the sweat glands are most concentrated.
Depending on the cause,
there are:
- Primary hyperhidrosis, when excessive sweating is not associated with other diseases. It usually appears in childhood or adolescence.
- Secondary hyperhidrosis occurs against the background of other diseases.
By intensity:
- Easy.
- Moderate.
- Heavy.
Possible causes of hyperhidrosis
Primary hyperhidrosis is one of the most common causes of increased sweating. It is based on the individual physiological characteristics of the body.
On the one hand, people with primary hyperhidrosis have a larger number of sweat glands, on the other hand, the sweat glands are more sensitive to various stimulating factors that cause sweating.
Typically, this type of hyperhidrosis manifests itself in childhood and intensifies during adolescence. This pathology is hereditary and is often transmitted from one of the parents. The severity can vary from moderate to very strong.
Secondary generalized hyperhidrosis is observed in infectious diseases in response to an increase in body temperature.
Purulent processes in the body, such as abscesses, phlegmon, and destructive pneumonia, can lead to sudden changes in temperature during the day.
These are serious conditions that require hospitalization and often surgical treatment.
Excessive sweating can be a consequence of chronic infections - tuberculosis, malaria, brucellosis, etc.
Generalized hyperhidrosis is observed with endocrine pathologies - for example, with an increase in the level of thyroid hormones. In addition, there is a loss of body weight with normal appetite, rapid heartbeat, and emotional arousal. Patients with diabetes mellitus often complain of increased sweating - special attention should be paid to the appearance of cold, sticky sweat, which may indicate a sharp drop in blood sugar levels. Hormonal changes during pregnancy and menopause are often accompanied by hyperhidrosis.
People with cancer of the hematopoietic system are characterized by increased sweating, especially at night. In addition, patients have no appetite, they lose weight, there is severe fatigue, body temperature can fluctuate between 37–38°C, and one or more groups of lymph nodes may enlarge.
Neuroses and panic attacks are often accompanied by increased sweating.
What diseases cause hyperhidrosis?
- Acute viral or bacterial infections.
- Chronic infections (tuberculosis, malaria).
- Endocrinological diseases (diabetes mellitus, hyperthyroidism, pheochromocytoma, acromegaly, carcinoid).
- Cardiovascular failure.
- Neurosis, panic attacks.
- Obesity.
- Neurological diseases (polyneuropathy, syringomyelia, chorda tympani syndrome).
- Lymphomas.
Which doctors should you contact if you have hyperhidrosis
? Since hyperhidrosis can be not only an independent condition, but also a symptom of other diseases, you should first consult a general practitioner. After a thorough examination, medical history, laboratory and instrumental studies, consultation with specialized specialists may be required: endocrinologist, neurologist, cardiologist, oncologist, infectious disease specialist, dermatologist.
Diagnosis and examinations for hyperhidrosis
The extent of hyperhidrosis and its boundaries can be determined using the Minor test. You need to apply a 2% iodine solution to the area where there is increased sweating, let the liquid dry and sprinkle the skin with starch. If you sweat excessively, your skin will turn purple or sometimes black.
To clarify the diagnosis, the doctor prescribes the following examinations:
- Clinical blood test with a detailed leukocyte formula to identify inflammatory processes in various infectious viral diseases.
There are two types of sweat glands in the human body:
- merocrine
- secrete sweat without destroying the cell; - apocrine
- secreting sweat with its destruction.
How do sweat glands work?
The secretory sections of the sweat glands are located in the reticular layer of the dermis and look like a twisted tube. Daily sweating occurs mainly due to the work of the merocrine glands. Sweat bubbles in the cells of their secretory sections are surrounded by a membrane. Approaching the cell membrane, these vesicles merge with it and release their contents into the lumen of the excretory duct. Up to 10 liters of sweat can be produced per day. 98% of it is water, and 2% is sialomucins, nitrogenous substances and ions.
The main producers of sweat are light cells, the cell membrane of which forms basal intussusceptions, increasing the working surface. Dark cells produce sialomucins. The third type of cells in the secretory compartments are myoepithelial cells. Their cytoplasm contains contractile proteins. These cells cover the secretory section with their processes, compress it and displace sweat into the excretory duct. Myoepithelial cells form synapses with the endings of nerve fibers, through which sweating is regulated. Both mero- and apocrine glands are innervated. The former are approached by cholinergic nerve fibers, and the latter by adrenergic nerve fibers. The excretory ducts of the sweat glands have three sections - epidermal, dermal and intercalary.
Cambial cells, most likely, by analogy with the same elements of other glands, are located in the intercalary excretory ducts. The wall of the excretory ducts is formed by a two-layer epithelium, the apical surface of the cells of the inner layer forms microvilli. The cells of the excretory ducts absorb ions and some water and return them back to the blood, which helps maintain the pH of the blood plasma. The epidermal section of the excretory ducts of the merocrine glands sometimes ends on the surface of the skin; its wall is formed by cells similar to keratinocytes. Apocrine glands are about ten times smaller. They are located mainly in the axillary and anogenital areas and have larger secretory sections. The ducts of the apocrine glands open into the hair funnel, slightly above the confluence of the sebaceous gland duct. Their protein secretion is mixed with sebum.
Sweating
Sweat glands have an abundant blood supply. Under conditions of overheating, blood supply, activity of myoepithelial cells, and sweating intensity increase. Sweating also increases when eating hot food, during emotional and physical stress, and many diseases.
The intensity of sweating varies with age. Newborns do not sweat; the function of sweating appears only in infancy, reaches its maximum development in adolescents and young men and fades away in old age. But we must remember that hyperfunction of the sweat glands is often a symptom of diseases (type 2 diabetes, disorders of the autonomic nervous system, etc.).
Merocrine sweat glands perform the following functions:
- sweating, which helps protect the body from overheating;
- moisturizing the epidermis (urea contained in sweat fluid retains water);
- removal of protein breakdown products and excess salts;
- maintaining a slightly acidic pH of the skin.
Apocrine glands:
- hormone dependent;
- determine the smell of the skin;
- play a role in the sexual behavior of animals, and possibly humans.
How does Formagel® affect the sweat glands?
Formagel®
suppresses the functions of sweat glands, regardless of their type. When Formagel® is applied to the skin, a thin film is formed, which not only prevents the evaporation of the active substance, but also promotes its complete penetration into the depths of the sweat glands. Formaldehyde has a coagulating effect on the tops of sweat-producing cells, thereby reducing sweating.