According to the literature [1, 2], 9–36% of patients with ulcerative colitis (UC) in remission exhibit symptoms similar to those of irritable bowel syndrome, the most common of which is abdominal pain (AP). The occurrence of abdominal pain in patients with UC in remission is explained by various reasons, including visceral hypersensitivity.
The purpose of the study was to evaluate the sensorimotor function of the anorectal region in patients with UC during remission with complaints of AB and to study the effectiveness of monotherapy with pinaverium bromide.
Pharmacodynamics and pharmacokinetics
The active ingredient pinaverium bromide is an antispasmodic. Its action is based on two mechanisms: a weak m-anticholinergic effect and selective blocking of calcium channels , which are located on the outer membranes of cells of the digestive tract and urinary tract. The drug reduces tone and eliminates spasms of smooth muscle muscles , reduces the intensity of hydrochloric acid , and improves blood flow to the walls of the gastrointestinal tract.
About 10% of the active substance is absorbed in the intestine. After an hour, the drug reaches its maximum content in the blood plasma. It is important that the drug does not affect the functioning of the heart muscle and blood vessels. The drug is processed in the liver, and pinaverium is excreted in the feces or through the kidneys.
Discussion
The basic treatment for any clinical variant of IBS is antispasmodic drugs. To achieve a relaxation effect at the peripheral level, reduce the contractile activity of the brain, eliminate spasms and restore normal transit, gastrointestinal smooth muscle relaxants of two main groups are traditionally used: anticholinergics and MS [7, 20]. The MS group includes drugs with different mechanisms of action: papaverine and drotaverine (phosphodiesterase inhibitors, promote intracellular accumulation of cAMP), selective direct-acting antispasmodic mebeverine (sodium channel blocker) and selective blockers of calcium channels in the gastrointestinal tract.
The drug Dicetel (pinoverium bromide) belongs to the latter group. The advantage of this drug is the absence of systemic anticholinergic effects, as well as systemic vasodilating and cardiotropic effects characteristic of calcium channel blockers of the nifedipine group. This determines the feasibility of its use for spastic contractions of the stomach and intestines, accompanied by pain in various gastrointestinal disorders, including IBS. At the moment, antispasmodics of direct myotropic action with a selective effect on the gastrointestinal tract are an integral and very effective part of the complex treatment of patients with functional gastrointestinal disorders.
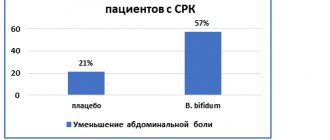
The purpose of our clinical study was to evaluate the effectiveness of Dicetel in relieving abdominal pain and symptoms of dyspepsia in patients with IBS, therefore the drug was used as monotherapy. In the observation groups, attention was drawn primarily to the same initial IBI and the same reaction to the drug in these groups at the end of treatment (comparable percentage reduction in pain intensity by 53.7 and 57%, respectively). The results of the study showed that Dicetel is an effective symptomatic remedy for relieving pain and improving intestinal functions in patients with IBS. Excellent and good results were obtained in half of the patients in both groups. It should be noted, however, that the effect of Dicetelas, rated as “satisfactory” in the groups, differed (see table), which is apparently due to the large number of patients with intense pain in group 2, although the average values of the initial IB were the same. Abdominal pain was completely relieved in only three patients in each group. We believe this is due to Dicetel monotherapy, while treatment of IBS requires a complex pathogenetic approach, including effects on the central and peripheral nervous systems, the use of psychotropic and laxatives, and, in the future, the use of drugs that regulate the functioning of serotonin receptors. Some patients in both groups showed no positive dynamics in terms of pain syndrome, which we also attribute to monotherapy. However, in these cases, it cannot be ruled out that some patients are not sensitive to the drug.
It is interesting that some patients in the IBS-C group (patients with mild and moderate pain syndrome) appeared to have independent bowel movements while taking Dicetel. This observation deserves, from our point of view, attention. Perhaps the use of laxatives is not always necessary for patients with IBS: perhaps restoring intestinal transit with the help of antispasmodics is sufficient.
The dynamics of ODI in both groups were equally positive, but significantly less pronounced than the dynamics of IB, which is also explained by the lack of complex treatment. In conclusion, it should be said that Dicetel, being a myotropic antispasmodic that selectively affects the tone of the gastrointestinal tract, can be successfully used in the treatment of abdominal pain in patients with IBS, with at least two variants of the course: IBS-C and IBS-M. It is most advisable to include Dicetel in the general complex of treatment measures, but in some cases, with moderate pain, it can be effective as monotherapy.
Side effects
After the drug was released on the market, cases of some adverse reactions were reported; it is impossible to reliably determine the frequency of their occurrence.
Possible side effects:
- abdominal pain , nausea and vomiting, diarrhea , dysphagia (reactions occur if dosage recommendations are not followed);
- hypersensitivity reactions to the active substance;
- skin rashes, itching , urticaria and other manifestations of allergies .
results
Comparative characteristics of the clinical, anamnestic and demographic indicators of the study participants are given in Table. 1.
Table 1. Clinical, anamnestic and demographic indicators of study participants
There were no statistically significant differences between patients with UC-AB, IBS and healthy volunteers by gender and age ( p
>0.017).
The level of quality of life in patients with UC-AB and patients with IBS was significantly lower than in healthy individuals ( p
<0.0001).
Moreover, the final index of physical health SF-36 profile in patients with UC-AB turned out to be statistically significantly lower than the corresponding indicator in patients with IBS ( p
<0.0001).
In table 2 shown
Table 2. Main indicators of sensorimotor function of the anorectal region in two groups of patients and a group of healthy volunteers; results of anorectal manometry in patients with UC-AB, IBS and healthy volunteers.
There were no significant differences in the level of basal pressure of the external anal sphincter in patients with UC-AB, IBS and healthy individuals ( p
>0.017).
In patients of both groups, the threshold for the first sensation of stretching occurred at a larger balloon volume than in healthy volunteers, but the differences were not significant ( p
> 0.017).
Rectal compliance to balloon distension was lower in patients of the two groups than in healthy individuals, but in patients with IBS the differences reached statistical significance ( p
<0.0001), and in patients with UC-AB the differences were at the level of a statistical trend (
p
= 0.026 ).
The maximum tolerated sensation occurred in patients of both groups at a significantly lower balloon volume than in healthy volunteers ( p
<0.004).
There were no statistically significant differences in the level of rectal compliance and maximum tolerated volume between patients of the two groups ( p
>0.017).
After 1 month of treatment with pinaverium bromide, 16 (72.7%) patients with UC-AB and 48 (94.1%) patients with IBS showed a positive effect in the form of relief of abdominal pain syndrome. Differences in the clinical effectiveness of monotherapy with pinaverium bromide between groups were statistically insignificant ( p
=0.092, Fisher's exact test).
In patients with improvement, there was a significant increase in the final quality of life indices of the SF-36 profile ( p
<0.05). In patients of both groups with positive clinical dynamics, an improvement in sensorimotor anorectal function was observed (Table 3).
Table 3. Dynamic assessment of the main manometric anorectal parameters in patients with UC-AB and IBS with clinical improvement.
The level of maximum tolerated volume significantly increased in patients of both groups. In patients with IBS-UC, a significant improvement in rectal compliance to balloon distension was observed. Moreover, after treatment, the differences in rectal compliance between patients of both groups and healthy individuals turned out to be statistically insignificant ( p
>0,05).
Thus, the positive effect of symptomatic therapy confirmed the functional genesis of AB in patients with UC in remission.
Dicetel, instructions for use (Method and dosage)
The tablets are taken during meals , without splitting or chewing .
According to the instructions for use of Dicetel at a dosage of 50 mg, the recommended daily dosage is one tablet once a day or two tablets twice a day. After consultation with a doctor, the dosage can be increased to 300 mg per day.
Three days before examining the intestines with barium, you should take two tablets, three times a day.
For a dosage of 100 mg, the daily dosage is two tablets, in two doses. If necessary, it can be increased to three tablets.
To prepare for an intestinal examination, take one tablet three times a day for three days before the procedure.
Material and methods
32 patients with UC of mild and moderate severity during remission with complaints of AB (UC-AB) were examined. Remission of Y.K. was defined as follows: a C-reactive protein level of less than 6 mg/ml and the absence of endoscopic signs of inflammation (according to colonoscopy, Mayo endoscopic index equal to 0) [3]. The remission period for UC ranged from 7 months to 22 years. The comparison group included 119 patients with irritable bowel syndrome (IBS), diagnosed according to Rome III criteria [4], and 23 healthy volunteers without gastrointestinal symptoms. Patients with UC-AB ( n
=32), IBS (
n
=119) and healthy volunteers (
n
=23) underwent anorectal manometry using a PC Polygraf hardware device (Synectics Medical) and studied their quality of life (SF-36, Healt Status Survey).
For 1 month, patients with UC-AB ( n
=22) and IBS (
n
=51) received treatment with pinaverium bromide 200 mg/day. After completion of treatment, patients were studied for clinical symptoms, manometric indicators and quality of life.
Quantitative variables are presented in the work as the mean value and standard error of the mean ( X±m
x).
t
was used to assess the statistical significance of the observed differences .
In case of repeated measurements, the paired Student's t test was used. Qualitative variables were compared using χ2 or Fisher's exact test. Differences were considered significant when comparing two groups at p
<0.05, three groups at
p
<0.017.
Dicetel's analogs
Level 4 ATC code matches:
Disflatil
Mint tablets
Kuplaton
Espumisan
Espumisan Baby
Espumisan L
Espumisan 40
Bobotik
Dill water
Pepsan-R
Sub Simplex
Infacol
Plantex
Bebinos
Meteospasmil
Romazulan
Common analogues of the drug: Bobotik, Disflatil, Carminativum, Bebinos , Kuplaton Plantex , Platifillin, Romazulan, cumin fruits, fennel fruits, Enterospasmil, Espusin-Zdorovye, Espumisan , Vinboron, Infacol, Kolikid, Duspatalin, Meteospasmil, Sab Simplex, Espicol.
Dicetel or Duspatalin - which is better?
It is believed that Duspatalin has a more pronounced antispasmodic effect, has less pronounced side reactions, and allergies occur much less frequently. However, it is not suitable for emergency treatment with excessive anxiety or, for example, problems with nutrition. In addition, the cost of the analogue is slightly higher than that of the original.
Pathogenetic approaches in the treatment of irritable bowel syndrome
Irritable bowel syndrome (IBS) refers to functional diseases in which the pathogenesis of the development of symptoms cannot be explained by organic causes. According to modern concepts, IBS is a psychosocial disorder with impaired visceral sensitivity and intestinal motor activity, caused either by a decrease in the threshold for pain perception, or an increase in the intensity of the sensation of pain impulses with a normal threshold for their perception [1].
At the same time, with almost all organic diseases of the gastrointestinal tract (GIT): peptic ulcer, gastroesophageal reflux disease, malignant tumors, cholelithiasis, chronic pancreatitis, etc., and somewhat less often than other organs and systems, symptoms characteristic of IBS are observed. This fact has allowed a number of authors to suggest the existence of a crossover syndrome between IBS and other diseases or to designate them as IBS-like disorders or symptoms. It is important to note that the principles of treatment of IBS and IBS-like disorders are the same [2].
IBS is considered the most common disease of internal organs. Worldwide, approximately 10–20% of the adult population has corresponding symptoms of IBS. According to most studies, women suffer approximately 2 times more often than men. The peak incidence occurs during the most active working age: 24–41 years. Symptoms of IBS continue for a long time, can overlap with other functional disorders and sometimes seriously impair quality of life.
The following factors are considered in the pathogenesis of IBS: altered gastrointestinal motility, visceral hypersensitivity, disruption of interaction in the brain-gut system, autonomic and hormonal changes, genetic and environmental factors, consequences of previous intestinal infections and psychosocial disorders.
Diagnostic criteria for IBS
To establish a diagnosis of IBS, the Rome III Consensus diagnostic criteria (2006) are used, which include: the presence of recurrent abdominal pain or discomfort on at least 3 days per month in the last 3 months, with the onset of symptoms at least 6 months, associated with two or more more of the following:
1) improvement after defecation; 2) the onset is associated with a change in stool frequency; 3) the onset is associated with a change in the shape of the stool.
Symptoms that support the diagnosis but are not part of the diagnostic criteria for IBS include:
1) violation of stool frequency: stool less than 3 times a week or more than 3 times a day; 2) abnormal stool shape: hard or bean-shaped, liquefied or watery; 3) straining during the act of defecation, or an imperative urge, or a feeling of incomplete evacuation; 4) secretion of mucus; 5) presence of flatulence.
| Rice. Bristol Stool Shape Scale |
According to the Rome III criteria, based on the Bristol Stool Shape Scale (Fig.), it is proposed to classify patients with IBS into the following groups:
1. IBS with a predominance of constipation in the presence of hard or bean-shaped feces in more than 25% of the total number of bowel movements, however, the presence of liquefied (mushy) or watery feces is also allowed in less than 25% of the total number of bowel movements. 2. IBS with a predominance of diarrhea, which is characterized by the presence of pasty or watery stool in more than 25% of the total number of bowel movements, but the presence of hard or bean-shaped stool is also allowed in less than 25% of the total number of bowel movements. 3. Mixed type of IBS, in which there is an alternation of hard or bean-shaped stool and pasty or watery stool in 25% or more of the total number of bowel movements. 4. Unclassified type of IBS - insufficient severity of deviations in stool consistency for the above types.
It should be noted that in the same patient, different subtypes of IBS can vary throughout the course of the disease [3].
The diagnosis of IBS is a diagnosis of exclusion, therefore, when establishing it, it is necessary to identify so-called anxiety symptoms that indicate a more serious pathology (Table 1).
The leading symptom of IBS is abdominal pain.
With any of the options, the leading symptom of IBS is abdominal pain. Clinical variants of abdominal pain syndrome in IBS are variable and diverse. Abdominal pain can be: dull, aching, bursting, vague, sharp, cutting, dagger-like, cramping, burning, of varying localization and intensity. The most common location of pain is the lower abdomen, less often the rectum. If the pain is intense, it may radiate to the back. Often the pain intensifies in an upright position or appears in the left hypochondrium or the left half of the chest, which is associated with the rise and accumulation of intestinal gases in the highest part of the colon - the splenic angle. Relief or reduction in the intensity of this type of pain is observed with the passage of gases, which is facilitated by the patient lying on his stomach with his buttocks raised up, which is referred to as “splenic flexure syndrome.” The presence of the latter allows us to exclude cardiac, vascular and pulmonary pathologies as the cause of pain. If there is a connection between pain and eating, then its appearance or intensification is provoked not so much by its constituent components as by the act of eating itself [4].
Treatment of patients with IBS
The IBS treatment program consists of two stages - the initial course and subsequent basic therapy. The goal of the primary course of treatment is to eliminate the symptoms of the disease and verify ex juvantibus the correctness of the diagnosis, which eliminates the need for further search for organic pathology and additional diagnostic procedures. The duration of the primary course of treatment is at least 6-8 weeks, basic therapy - 1-3 months. The choice of program is determined by the interaction of several factors and depends on the leading symptom (pain, flatulence, diarrhea, constipation), its severity and impact on the quality of life, as well as on the nature of the patient’s behavior and his mental state.
The patient is prescribed an exclusion diet that does not contain: caffeine, lactose, fructose, sorbitol, vinegar, alcohol, pepper, smoked foods, as well as products that cause excessive gas formation.
Treatment of patients with IBS with predominant abdominal pain
The main mechanisms for the development of abdominal pain are due to impaired intestinal motility and visceral hypersensitivity. Depending on the state of tone and peristaltic activity of the circular and longitudinal layers of smooth muscles, two types of motor disorders are formed: 1) accelerated transit of chyme through the intestine, caused by an increase in the propulsive activity of the longitudinal muscle layer of the intestine with the development of diarrhea; 2) slow transit of intestinal contents due to hypertonicity of the circular muscles (spastic dyskinesia) of the colon with the formation of constipation. Since smooth muscle spasm is one of the main components of abdominal pain in IBS, myotropic antispasmodics are considered the drugs of choice for relieving spasms of any origin and relieving pain, especially in functional disorders of the gastrointestinal tract. They affect the final stage of the formation of hyperkinesia, regardless of its cause and mechanism.
The motor function of the intestine is under the control of numerous regulatory influences (central, peripheral, enteric nervous systems and gastrointestinal peptides), which determine the normal tone and contractile activity of the smooth muscles of the intestinal wall. In this regard, smooth muscle cells can be influenced in various ways.
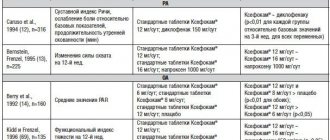
Depending on the main mechanism of action on the stages of muscle fiber contraction, the following groups of muscle relaxants are distinguished (Table 2). Anticholinergics reduce the concentration of intracellular calcium ions, which leads to muscle relaxation. It is important to note that the degree of relaxation is directly dependent on the previous tone of the parasympathetic nervous system. The latter circumstance determines significant differences in the individual effectiveness of drugs in this group. Quite low efficiency, lack of selectivity (effect on almost all smooth muscles, including the urinary system, blood vessels, etc., as well as secretory glands) and therefore a wide range of side effects, as well as the danger of developing muscle fiber hyperrelaxation limit the use of anticholinergic drugs for a course of treatment to relieve pain in a significant proportion of patients with IBS.
Phosphodiesterase blockers - myotropic antispasmodics (papaverine, drotaverine) promote the accumulation of cAMP in the cell and a decrease in the concentration of calcium ions, which inhibits the connection of actin with myosin. These effects can be achieved by inhibition of phosphodiesterase, or activation of adenylate cyclase, or blockade of adenosine receptors, or a combination thereof. When using the above group of antispasmodics, it is necessary to take into account significant individual differences in their effectiveness, lack of selectivity, the development of hypomotor dyskinesia and hypotension of the sphincter apparatus of the digestive tract, especially with long-term use. These drugs are used short-term (from a single dose to a week) to relieve spasms, but not for a course of treatment aimed at relieving and preventing relapse of the disease.
Serotonin plays a significant role in the regulation of gastrointestinal motility. There are several subtypes of serotonin receptors (5-NT1-4), but the most studied are 5-NT3 and 5-NT4. The binding of serotonin to 5-NT3 promotes relaxation, and with 5-NT4 - contraction of muscle fiber. At the same time, the exact mechanisms of action of serotonin on the muscle fibers of the gastrointestinal tract have not been established. Currently, the drugs in this group include the 5-NT3 antagonist alosetron, the full 5-NT4 agonist prucalopride, and the partial 5-NT4 agonist tegaserod (the drugs are not used in Russia).
Endogenous opiates play a certain role in the regulation of the motor function of the gastrointestinal tract. When they bind to μ- (Mu) and δ- (Delta) opiate receptors of myocytes, stimulation occurs, and with κ- (Kappa) - a slowdown of motor activity. Currently, in the treatment of patients with IBS, an opiate receptor agonist is used - trimebutine (Trimedat) - a regulator of gastrointestinal motility.
However, when treating patients with IBS, preference is given to myotropic antispasmodics with a selective effect on smooth muscle cells of the gastrointestinal tract (mebeverine, pinaverium bromide). The group of blockers of fast sodium channels of the myocyte cell membrane includes the drug mebeverine (Duspatalin), the mechanism of action of which is reduced to the blockade of fast sodium channels of the myocyte cell membrane, which disrupts the flow of sodium into the cell, slows down depolarization processes and blocks the entry of calcium into the cell through slow channels. As a result, myosin phosphorylation is disrupted and muscle fiber contraction stops. In addition, the drug blocks the replenishment of intracellular stores with calcium ions, which ultimately leads to only a short-term release of potassium ions from the cell and its hypopolarization, which prevents the development of long-term relaxation of the myocyte. The drug is prescribed 1 capsule 2 times a day 20 minutes before meals.
At the final stage, the balanced functioning of the smooth muscle apparatus depends on the concentration of calcium ions in the cytoplasm of the myocyte. Calcium ions enter the myocyte through specialized membrane channels. The opening of calcium channels leads to an increase in calcium concentration, the formation of the actin-myosin complex and contraction of smooth muscles, and blocking of the channels is accompanied, accordingly, by a decrease in the calcium concentration in the myocyte and its relaxation. Previously, attention was drawn to the fact that calcium antagonists used to treat cardiovascular diseases (nifedipine and verapamil) had a relaxing effect on the smooth muscles of the gastrointestinal tract. This was the reason for creating a group of modern effective myotropic antispasmodics - selective blockers of calcium channels in the smooth muscles of the gastrointestinal tract. The classic representative of this group is pinaveria bromide. Pinaveria bromide was first registered in 1975 and since then the drug has been prescribed to approximately three million patients annually worldwide. It is currently being sold in more than 60 countries. In Russia, the drug is registered under the name Dicetel.
Dicetel is a calcium antagonist with a highly selective antispasmodic effect on intestinal smooth muscles. This determines its therapeutic use for abdominal pain, intestinal dysfunction and intestinal discomfort due to IBS. Currently, thanks to the results of electrophysiological and pharmacological studies, at least four types of calcium channels have been identified: L, T, P, N. L-type channels are located on the surface of the cytoplasmic membrane of smooth muscle cells and consist of several subunits, of which the most important is alpha1- subunit. The alpha1 subunit of the L-type channel can open due to potential differences at the surface of the cell membrane (neuronal control) or indirectly in the presence of digestive hormones and mediators. Studies using DNA cloning and polymerase chain reaction techniques have demonstrated that the structure of the alpha1 subunit of the calcium channel in intestinal cells is different from that of the alpha1 subunit of calcium channels in cells of other tissues. Dicetel has a high affinity for the isoform of the alpha1 subunit of the calcium channel, predominantly localized in intestinal cells, which emphasizes the high selectivity of the drug for this target organ [5]. Thus, Dicetel has a unique dual therapeutic effect: not only an antispasmodic effect, but also the ability to reduce visceral sensitivity. These effects are realized both by blocking voltage-gated and receptor-gated calcium channels of colon smooth muscle cells, and by reducing the sensitivity of intestinal muscle receptors to gastrointestinal hormones and mediators, such as cholecystokinin and substance P [6].
Pharmacodynamics of pinaverium bromide, therapeutic effects:
- pinaveria bromide has maximum affinity for smooth muscle cells of the colon;
- significantly shortens the transit time through the colon, mainly by increasing the speed of passage through the descending and rectosigmoid zones of the colon;
- for diarrhea, the drug does not increase the mobility of the colon;
- inhibition does not increase with repeated stimulation and is distinguished by the fact that it does not depend on voltage;
- the drug can be used for a long time without fear of developing intestinal hypotension.
Over the past 20 years, the effectiveness of Dicetel in relieving symptoms of IBS in all subtypes has been assessed in numerous multicenter, open, comparative and placebo-controlled studies both in Russia and abroad. Evaluation of the effectiveness of Dicetel by both researchers and patients demonstrated a high frequency of good and very good results in relieving the main symptoms of IBS: abdominal pain, constipation, diarrhea, bloating. The drug effectively and quickly relieves pain caused by spastic contractions of the intestinal wall and restores intestinal transit.
The drug was well tolerated, with minimal side effects. A meta-analysis of 26/23 studies grouped various antispasmodics according to their adverse reactions compared with placebo. Dicetel was found to be better tolerated than hyoscine, trimebutine, cimetropium bromide, otilonium bromide, peppermint essential oil, and dicyclomine bromide [7]. Dicetel does not interact with the autonomic nervous system and therefore does not have anticholinergic side effects, especially when using therapeutic doses. In this regard, the drug can be used in patients with IBS who have concomitant prostatic hypertrophy, urinary retention or glaucoma. Unlike standard calcium antagonists, Dicetel in therapeutic doses does not have cardiovascular effects. This is due to its very low level of systemic absorption, predominantly hepatobiliary excretion, and high specificity for both intestinal smooth muscle tissue and calcium channel subtypes. Dicetel is prescribed 100 mg × 3 times a day with meals. Dicetel can be combined with bulk laxatives (lactulose, polyethylene glycol, psyllium) in the treatment of IBS patients with constipation. In case of IBS with diarrhea predominance, the effectiveness of Dicetel can be increased by combination with enveloping drugs and adsorbents.
In the presence of flatulence, simethicone-dimethicone preparations can be added to Dicetel, which will increase the effectiveness of treatment for patients with IBS.
Treatment of patients with IBS with predominant constipation
For IBS with constipation, if there is no effect of diet (increasing the intake of dietary fiber to 25 g / day) and myotropic antispasmodics, the treatment regimen includes osmotic laxatives, among which lactulose, milk of magnesia, Psilikon-Psilium, Macrogol 4000 and etc. Irritating laxatives for the treatment of IBS with constipation are contraindicated because they can provoke spastic contractions of the intestine and increase pain [8].
Treatment of patients with IBS with diarrhea predominance
If the patient has a slight increase in stool frequency, it is possible to use adsorbents - calcium carbonate, activated carbon, dysmectite 3 g per day in the form of a suspension. However, it must be taken into account that the antidiarrheal effect of these drugs occurs no earlier than after 3–5 days. If the combined use of antispasmodics and adsorbents is ineffective and there is a significant increase in stool frequency, Loperamide may be prescribed. Loperamide is an agonist of m-opiate receptors, which determines its ability to suppress fast propulsive contractions of the intestine and leads to a slowdown in the transit of feces. This is accompanied by a decrease in the passage of the liquid part of the chyme, as a result of which the reabsorption of fluid and electrolytes in the intestine increases. The starting dose of Loperamide for adults is 4 mg (2 capsules). The maintenance dose should not exceed the maximum permissible daily dose for adults - 16 mg (8 capsules).
Treatment of patients with IBS with a predominance of flatulence
Inherent and distressing symptoms of IBS for the patient are bloating or a feeling of abdominal distension, as well as belching and excessive release of gas through the rectum. These symptoms are minimal in intensity in the morning and intensify in the evening. Their formation is based not so much on an increase in the volume of intraluminal gas, but on a decrease in tolerance to stretching of the intestinal wall. The main reasons for excess gas content in the intestine are an increase in its production by intestinal microflora, a slowdown in transit as a result of spastic dyskinesia, as well as impaired absorption of the intestinal wall into the blood, in particular during rapid transit during diarrhea.
If complaints of bloating and flatulence predominate in the IBS clinic, with an adequate assessment of the role of gas formation in each specific case, the prescription of drugs is indicated, the mechanism of action of which is based on weakening the surface tension of gas bubbles in the digestive tract, which ensures resorption and free release of gases. One of these symptomatic drugs to reduce gases in the intestines is simethicone. For flatulence, 2 capsules of simethicone are prescribed 3-5 times a day. The simultaneous administration of antispasmodics improves gas transit through the intestine. It should be taken into account that in the pathogenesis of excess gas formation, a violation of the intestinal microflora plays a significant role.
Correction of intestinal microflora
Recently, a large amount of data has accumulated indicating the role of disturbances in intestinal microflora in the formation of IBS and IBS-like disorders [9]. This is especially true for patients with post-infectious IBS, whose symptoms developed after acute intestinal infections [10, 11].
The results of experimental and clinical studies have shown that changes in the composition and habitat of intestinal microflora are accompanied by disturbances in motor activity and sensory sensitivity of the intestine, which underlies the formation of symptoms of intestinal dyspepsia, including abdominal pain, stool disorders, flatulence, etc. [12, 13]. In IBS with diarrhea, accelerated transit of chyme through the intestine, caused by an increase in the propulsive activity of the longitudinal muscle layer, is accompanied by disruption of the processes of hydrolysis and absorption due to short-term contact of food ingredients with enzymes. This creates conditions for the development of bacterial overgrowth, increased production and decreased absorption of intestinal gas into the blood. Slow transit of intestinal contents due to hypertonicity of the circular muscles (spastic dyskinesia) of the colon with the development of constipation is accompanied by an increase in intraluminal pressure not only in the colon, but also in the small intestine and duodenum, as well as in the stomach. Long-term stasis of intestinal contents leads to disruption of the quantitative and qualitative composition of the intestinal microflora.
In the presence of excessive bacterial growth in the intestines, severe flatulence, or when opportunistic microflora is detected in intestinal content cultures, drug therapy, regardless of the type of IBS, is recommended to be supplemented with one or two seven-day courses of broad-spectrum intestinal antiseptics (Alfa-normix (rifaximin), furazolidone, nifuroxazide, Sulgin (sulfaguanidine), etc. in standard doses), with a change in the drug in the next course of treatment and subsequent use of probiotics (Bifiform, Linex, etc.).
Psychological treatment
Psychological treatment should be used when IBS symptoms are refractory to drug treatment or there is evidence that stress and psychological factors contribute to exacerbation of gastrointestinal symptoms. The patient's understanding of the need for such treatment is an important factor in the success of therapy. Treatment is selected with the participation of a psychotherapist. For IBS, tricyclic antidepressants or selective serotonin uptake inhibitors are usually prescribed. The purpose of prescribing such drugs is: 1) treatment of mental comorbidity [14]; 2) changes in the physiology of the gastrointestinal tract (visceral sensitivity, motility and secretion) [15]; 3) decreased central perception of pain [16]. It is important to understand that antidepressants are prescribed for IBS as drugs that directly reduce visceral hypersensitivity, and only secondarily to relieve depressive symptoms caused by pain. Such therapy should continue for 6–12 months until the maintenance dose is reduced and determined [17].
A variety of complementary treatments are also used for IBS, including exercise therapy, physical therapy, hypnotherapy, biofeedback, and group interpersonal treatment.
Literature
- Drossman DA, Camilleri M., Mayer EA, Whitehead WE AGA technical review on irritable bowel syndrome // Gastroenterology. 2002; 123:2108–2131.
- Farrokhyar F., Marshall JK, Easterbrook B. et al. Functional Gastrointestinal Disorders and Mood Disorders in Patients with Inactive Inflammatory Bowel Disease: Prevalence and Impact on Health // Inflamm Bowel Dis. 2006; 12 (1): 38–45.
- Drossman DA The Functional Gastrointestinal Disorders and the Rome III Process // Gastroenterology. 2006; 130 (5).
- Yakovenko E. P., Agafonova N. A., Yakovenko A. V., Ivanov A. N., Pryanishnikova A. S., Krasnolobova L. P. The role of motor disorders in the mechanisms of formation of clinical manifestations of irritable bowel syndrome (IBS) and IBS-like disorders // Questions of therapy. Consilium Medicum. 2011; 1:69–73.
- Morel N., Buryi V., Feron O., Gomez JP, Christen MO, Godfraind T. The action of calcium channel blockers on recombinant L-type calcium channel α1-subunits // Br J Pharmacol. 1998; 125:1005–1012.
- Christen MO Pinaverium bromide: A calcium antagonist with selectivity for the gastrointestinal tract // Today's Therapeutic Trends. 1995; 13 (2): 47–62.
- Poynard T., Naveau S., Mory B., Chaput JC Meta-analysis of smooth muscle relaxants in the treatment of irritable bowel syndrome // Aliment Pharmacol Ther. 2001; 15: 355–360.
- Ramkumar D, Rao SS Efficacy and safety of traditional medical therapies for chronic constipation: systematic review // Am J Gastroenterol. 2005; 100:936–971.
- Grigoriev P. Ya., Yakovenko E. P. Irritable bowel syndrome associated with dysbiosis // Consilium medicum. 2003. T. 2, no. 7. pp. 305–307.
- Yakovenko E., Grigoriev P., Tcherenchimediins at al. Is irritable bowel syndrome (IBS) related to altered gut flora? // Gut. 1997. Vol. 41, suppl. 3. PA 123.
- Parfenov A.I., Ruchkina I.N., Osipov G.A. Bismuth tripotassium dicitrate in the treatment of patients with post-infectious irritable bowel syndrome // Rus. honey. magazine 2006. T. 8, No. 2. P. 78–81.
- Dunlop SP, Jenkins D., Spiller RS Distinctive clinical, psychological and histological features of postinfective irritable bowel syndrome // American J Gastroenterology. 2003. Vol. 98, No. 7. P. 1578–1583.
- Tazume S., Ozawa A., Yamamoto T. at al. Ecological study on the intestinal bacteria flora of patients with diarrhea // Clin Infect Dis. 1993; 16. Suppl 2: S77–S82.
- Lancaster-Smith MJ, Prout BJ, Pinto T. et al. Influence of drug treatment on the irritable bowel syndrome and its interaction with psychoneurotic morbidity // Acta Psychiatr Scand. 1982; 66:33–41.
- Gorard DA, Libby GW, Farthing MJG Effect of a tricyclic antidepressant on small intestinal motility in health and diarrhea-predominant irritable bowel syndrome // Dig Dis Sci. 1995; 40: 86–95.
- Mertz H., Fass R., Kodner A. et al. Effect of amitryptiline on symptoms, sleep, and visceral perception in patients with functional dyspepsia // Am J Gastroenterol. 1998; 93: 160–165.
- Onghena P., Houdenhove BV Antidepressant-induced analgesia in chronic non-malignant pain: a meta-analysis of 39 placebo-controlled studies // Pain. 1992; 49: 205–219.
N. A. Agafonova, Candidate of Medical Sciences, Associate Professor E. P. Yakovenko, Doctor of Medical Sciences, Professor A. S. Pryanishnikova, Candidate of Medical Sciences, Associate Professor A. V. Yakovenko, Candidate of Medical Sciences, Associate Professor A. N. Ivanov, Candidate of Medical Sciences, Associate Professor
RGMU , Moscow
Contact information about the authors for correspondence: [email protected] ru
Dicetel price, where to buy
You can buy 20 tablets of 50 mg for 317 rubles.
The price of Dicetel for 100 ml is approximately 485 rubles for 20 pieces.
- Online pharmacies in RussiaRussia
ZdravCity
- Dicetel tablets p.p.o.
100 mg 20 pcs Abbott Healthcare SAS/Mylan Laboratories SAS RUB 754 order - Dicetel tablets p.p.o. 50 mg 20 pcs. Mylan Laboratories SAS
RUR 543 order