The symptoms of pain differ depending on the problem the patient is facing. In this article, we will look at pain and accompanying symptoms in the section of irritable bowel syndrome and mention other possible pathologies.
People experiencing pain in the intestines characterize it with the following symptoms:
- uncertain; - burning; - stupid; - constant; - dagger; - twisting.
Most often, intestinal pain is localized in the iliac regions on the left. Recall that the iliac region is located in the lower part of the abdominal cavity. The pain intensifies during meals, and after taking antispasmodics, during bowel movements, or when gas is released, it decreases.
Why do antispasmodics help with intestinal pain?
The principle of action of antispasmodics is based on a lowering effect on the tone of smooth muscle organs, or on a disruptive effect on nerve impulses associated with smooth muscles. In other words, the drugs prevent spasm. The latter creates a painful contraction of the intestinal muscles.
Another feature of pain in the intestines is their rare occurrence at night. As a rule, the nature of the pathology comes in waves, with an increase in the daytime and intensification after eating food.
Pain in the intestines may be accompanied by constipation or diarrhea. The latter arises from urges. After going to the toilet, the feeling of incomplete bowel movement persists. In the case of constipation, with pain, sheep feces or other dense masses are often released.
Additional accompanying symptoms:
- bloating; - stretching; - flatulence; - stomach rumbling.
Symptoms of anxiety
Pain in the intestines is not always harmless. Immediately make an appointment with a doctor if, in addition to pain in the intestines, you observe:
- weight loss; - presence of blood in the stool; - fever, rise in temperature; - weakness.
Statistically, 1% of people who experience intestinal pain have colitis. Food intolerance/irritable bowel syndrome occurs in 25% of cases. In 6% of cases, we are talking about thyroid dysfunction (especially important for residents of endemic regions, for example, for residents of the Urals). Tumors occur in 0.3% of cases. In statistics, much depends on the gender and age structure of patients.
Typical manifestations of ulcerative colitis
Ulcerative colitis is a form of inflammatory bowel disease.
In ulcerative colitis, inflammation occurs in the colon, the last 1.5 meters of the digestive tract. Unlike the small intestine, where nutrients are absorbed, the large intestine absorbs primarily water. For this reason, one of the most common manifestations of ulcerative colitis is diarrhea , that is, frequent loose stools (diarrhea), almost always with blood . Inflammation leads to increased permeability of the blood vessels located under the mucous membrane of the colon, so that water is not only not absorbed, but is also released excessively into the intestinal lumen. In addition to dehydration, diarrhea due to ulcerative colitis is accompanied by a loss of electrolytes - important trace elements such as sodium, chlorine and potassium. Dehydration and severe electrolyte deficiency not only make you feel unwell, but can also lead to abnormal heart rhythms. Loss of potassium during severe intestinal inflammation increases the likelihood of toxic dilatation, one of the dangerous complications of ulcerative colitis. During severe exacerbations of ulcerative colitis, doctors restore the ratio of electrolytes and the volume of fluid in the body by administering solutions intravenously.
Rice. 1. Sections of the large intestine. Ulcerative colitis affects only the large intestine.
It is not always the case that with every urge to have a bowel movement, a person suffering from ulcerative colitis produces copious loose stools. false urges occur : the desire to go to the toilet appears, but instead of stool, a small amount of mucus and blood is released with virtually no feces. Often such urges become imperative : a person has to run to the toilet, and in people with weakened anal muscles that hold stool in the rectum, fecal incontinence may occur. The reason for these frequent urges is inflammation of the reflexogenic zone in the rectum. Normally, the desire to empty the bowel occurs when feces accumulate in the expanded part of the rectum - the ampulla. During inflammation, a signal to the brain about filling the ampoule often occurs with a minimal amount of stool in the intestine, which would not cause additional sensations in a healthy person.
Rice. 2. Types of lesions in ulcerative colitis. Proctitis refers to inflammation of only the rectum (the last 10 cm of the large intestine). Left-sided damage is limited to the left bend of the colon (as happens, for example, with proctosigmoiditis - inflammation of the rectum and sigmoid colon). Inflammation that extends beyond the left flexure is called total.
The most common manifestation of ulcerative colitis, which forces you to consult a doctor, is the passage of blood in the stool . The release of blood in ulcerative colitis differs in nature from classic bleeding from a damaged vessel (such as, for example, after removal of a polyp or when the blood supply to the intestine is disrupted). Blood cells in ulcerative colitis leak through the wall of blood vessels due to increased permeability: this is a consequence of the action of various molecules (for example, histamine) released by immune cells attacking the intestine. For this reason, in ulcerative colitis, traditional methods of stopping bleeding are ineffective: clipping (installing a clamp) of the bleeding surface of the intestine, coagulation (cauterization) and the use of hemostatic agents. Because blood flow increases gradually, in people with worsening ulcerative colitis, anemia (a decrease in hemoglobin, the protein in the blood that carries oxygen) appears gradually. With such gradual blood loss, the body often has time to adapt to anemia, while in a healthy person, with sudden bleeding from a damaged vessel, a sudden loss of blood can cause shock - a severe protective reaction of the body to a decrease in pressure in the vessels.
Anemia is a common manifestation of ulcerative colitis. Anemia (anemia) is a decrease in hemoglobin concentration. First, red blood cells (erythrocytes) are lost in the stool. Second, inflammatory molecules (such as tumor necrosis factor alpha, which supports inflammation) suppress hemoglobin formation. With anemia, human organs and tissues receive an insufficient amount of oxygen, the carrier of which is hemoglobin. Symptoms of anemia include general weakness and drowsiness, headache, pale skin and shortness of breath during physical activity. Severe anemia (hemoglobin concentration less than 90 grams per liter) during an exacerbation of ulcerative colitis is considered an indication for hospitalization.
The frequency of stool and the severity of diarrhea depend on the area of intestinal inflammation. With total colitis (inflammation of the entire colon), water does not have time to be absorbed, and loose stools are passed out very often. At the same time, blood and protein are lost faster and general manifestations of the disease appear (such as weakness and swelling ). With ulcerative colitis affecting only the last 10 cm of the colon (ulcerative proctitis), a person experiences paradoxical constipation : despite frequent false urges with blood, the actual stool is not passed. This is how the intestinal nervous system reacts to inflammation of the rectum: areas located above the inflammation zone begin to contract poorly.
The secretion of mucus in ulcerative colitis is one of the intestinal protective reactions to damage to its wall. Mucus is secreted by goblet cells (they actually resemble “cups” or “glasses” in shape, in which a viscous substance accumulates). Mucus in ulcerative colitis can be excreted in the stool for a long time, after the inflammation has subsided.
Destruction of intestinal tissue due to inflammation and blood loss lead to protein deficiency in the body (hypoproteinemia). Blood proteins (proteins), the most important of which is albumin, are not only the main building material for body tissues, but also retain water in the lumen of blood vessels. When protein is lost, water from the vessels rushes into the intercellular space, accumulating in the cavities of the body and its lower half. swelling often occurs , most often in the legs. In severe hypoproteinemia, fluid accumulates in the chest cavity (hydrothorax) or abdominal cavity (ascites).
An exacerbation of ulcerative colitis is accompanied by the release of numerous inflammatory mediators into the blood - molecules that attract new immune cells to the intestines and affect the regulation of body temperature. Increased body temperature - fever - is a common indication for hospitalization, since it indicates either severe inflammation or an associated infection, for example, the proliferation of the bacterium Clostridium difficile.
Abdominal pain with ulcerative colitis is an uncommon symptom. With ulcerative colitis, in most cases, only the mucous membrane is inflamed - the inner thin layer of the intestinal wall, which does not contain pain receptors. For this reason, during a biopsy (taking a piece of the mucous membrane), a person does not feel anything. Most often, pain in ulcerative colitis occurs before bowel movement due to spasm - contraction of the muscles that make up the intestinal wall. These attacks of pain become less frequent and gradually disappear as inflammation in the intestines decreases. Very severe abdominal pain with very frequent bowel movements and copious discharge of blood can be a manifestation of a severe and dangerous complication of ulcerative colitis - intestinal perforation. Bowel perforation is an indication for emergency surgery.
Finally, ulcerative colitis, like another inflammatory bowel disease, Crohn's disease, can cause extraintestinal manifestations, in which circulating immune complexes are formed in the intestine and travel with the blood to other organs. Typical extraintestinal manifestations of ulcerative colitis are primary sclerosing cholangitis (inflammation of the bile ducts in the liver), erythema nodosum and pyoderma gangrenosum (inflammation of the skin), iritis and iridocyclitis (inflammation of the eyes), and various arthritis (inflammation of the joints).
It is important to understand that even if the listed symptoms are present, ulcerative colitis is not a foregone conclusion. A number of examinations and tests are required to establish a diagnosis.
*Does not replace medical advice. To make a diagnosis and prescribe treatment, you must consult a specialist.
What to do
Regardless of age and personal prejudices regarding the disease, make an appointment with a doctor.
If symptoms of anxiety are identified, or additional risk factors are identified (for example, age), the patient will be prescribed additional examination, including an endoscope. If there are no deviations, we will establish a diagnosis and examine visceral sensitivity.
About visceral sensitivity in the context of pain in the intestines
Irritable bowel syndrome can be caused by stress, infections, smoking, medications, and certain types of foods. Gut sensitivity is how it responds to physiological stimuli. As you know, even strong fear or any other emotional impact causes gastrointestinal reactions.
Treatment of pain due to constipation
In the fight against pain due to constipation, the following will help:
- Nutrition aimed at increasing the amount of fiber consumed. Diet is the main method of treating functional constipation caused by decreased intestinal motility.
- Lifestyle changes. Involves increased physical activity and regular physical activity.
- Discontinuation of medications that cause constipation.
It is important to understand that you should not stop taking medications prescribed by your doctor on your own. For example, if you are taking iron supplements that are causing you to have bowel movements, changing the dosage yourself or stopping it may make your iron deficiency anemia worse. Contact your doctor for advice on alternative medications or dosage adjustments. Particular caution should be exercised when taking hormonal drugs, antidepressants, anticonvulsants, and narcotic analgesics.
The main condition for getting rid of abdominal pain due to constipation is the normalization of stool. Symptomatic treatment in the form of painkillers and antispasmodics will not give long-term results. In addition, it is worth remembering that in some cases, constipation is associated with a weakening of intestinal motility - a change in the tone of its muscles. In this case, anti-spasm medications may aggravate the underlying problem.
Foods high in fiber will help normalize stool. These include bran, white cabbage (fresh and pickled), celery and other vegetables. Whole grains such as bulgur and buckwheat, as well as nuts, are rich in dietary fiber.
At the same time, it is better to avoid products that have a fixing effect. These include foods high in tannin: chocolate, black tea, red wine, white rice, etc. You should avoid baked goods, sweets, bread and pastries with cream - they increase gas formation and also provoke fermentation in the intestines.
You need to eat in small portions, but often. Small meals 5-6 times a day will ensure a uniform supply of nutrients to the body and will help avoid stretching the walls of the stomach and intestines.
Medication should not be aimed at eliminating pain, but at its cause. Pain usually goes away with bowel movements, so it is important to choose the appropriate way to quickly get rid of the problem. Laxatives will help cope with this. They come in several types:
- Osmotic, or saline, increases the volume of fluid in the intestines.
- Stimulating - act irritatingly on intestinal receptors, stimulating peristalsis.
- Volumetric - increase the volume of stool and change its consistency.
- Auxiliary - mechanically help promote the movement of feces in the intestines (for example, oil).
There are also local drugs that act as an irritant on the mucous membranes of the rectum and soften the passage of feces. The use of cleansing enemas may also be advisable, but often resorting to them is not recommended due to possible disturbances of the local microflora.
Diverticulosis of the colon
The main reasons for the formation of the disease:
- violation of the structure of the walls of the colon;
- dysfunction of blood vessels;
- weakening of muscle tissue.
In addition, there are factors that can provoke the development of the described pathologies:
- chronic intestinal inflammation;
- regular constipation/diarrhea;
- unbalanced diet;
- trauma/surgery;
- deficiency of useful compounds;
- natural wear and tear of muscles (in old age);
- insufficient consumption of plant fiber.
Among the signs of the development of the disease are:
- increased gas formation, bloating and rumbling in the abdomen;
- excessive salivation;
- intestinal dyspepsia;
- systematic stool disorder;
- formation of streaks of blood and/or mucus in the stool;
- feeling of nausea;
- lower abdominal pain
- fever;
- intestinal bleeding.
For uncomplicated diverticulosis, the doctor prescribes the following medications:
- laxatives (Duphalac, Romphalac, Goodluck);
- antidiarrheal drugs (Silix, Loperamide, Lopedium);
- painkillers (Drotaverine, Spazmalgon, No-shpa);
- agents that stimulate gastrointestinal motility (Motilium, Domperidone);
- enzymes (Creon, Mezim, Pancreatin);
- broad-spectrum antibiotic drugs (Amoxicillin, Ceftriaxone, Ampicillin).
In some cases, surgical treatment is used.
Colon polyps
There are several factors that can trigger the development of the disease:
- heredity;
- chronic inflammation of the gastrointestinal tract;
- endocrine system disorders;
- autoimmune diseases;
- presence of bad habits;
- frequent stress, emotional overstrain.
Polyps appear:
- alternating constipation and diarrhea;
- the formation of mucus and/or blood in the stool;
- intestinal discomfort;
- headache;
- general weakness;
- pain syndrome in the lower abdomen;
- intestinal obstruction.
In some cases, intestinal bleeding is present, which can result in anemia.
Polyps cannot be cured with the use of medications. Therapy for this pathology is carried out only by surgery.
In case of early diagnosis and treatment, the prognosis is considered favorable. Relapses are possible, which usually occur a couple of years after surgery.
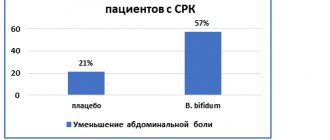
Symptoms of irritable bowel syndrome
- nausea and gag reflex;
- flatulence with copious release of gases;
- abdominal pain or cramps;
- constant bloating;
- stool disorders - constipation or diarrhea;
- pain in the lower abdomen;
- sleep disturbance;
- increased heart rate;
- increased fatigue;
- long digestion of food;
- the appearance of mucus in the stool;
- false urge to defecate;
- loss of appetite.
Also, the disease is often accompanied by symptoms that, at first glance, are not characteristic of intestinal pathologies: headaches, discomfort in the spine and muscles, weight loss and abdominal swelling. All these symptoms are not constant, they can disappear and reappear over time. Unpleasant sensations most often appear after each meal, and then become less pronounced.
Hirschsprung's disease
This disease is congenital, occurs in utero, and is hereditary.
Main symptoms:
- constipation;
- feeling of nausea;
- abdominal pain;
- gagging;
- flatulence.
We recommend a video about congenital disease in children:
Conventional treatment cannot completely cure the patient. However, it can be used to prepare the patient for surgical therapy. To do this you need:
- stick to the diet menu;
- stimulate peristalsis with massage, therapeutic exercises;
- do enemas;
- use protein preparations, electrolyte solutions intravenously;
- take vitamins.
The prognosis for Hirschsprung's disease is relatively favorable if surgical treatment is performed before complications develop.
Symptoms of colon disease
Signs of this disease:
- Aching, spasmodic pain occurs in the lower abdomen, as well as in the umbilical area.
- After painful bowel movements, relief comes.
- In the absence of inflammation, eating and the occurrence of pain are not related to each other.
- Constipation appears, gradually turning into a chronic form.
- Flatulence develops (most often after eating).
- There may be blood and mucus in the stool.
Diarrhea may also appear, alternating with constipation.
Intestinal structure
The small intestine, which is divided into sections:
- duodenum;
- jejunum;
- ileum.
Colon:
- cecum;
- colon;
- sigmoid colon;
- rectum;
- appendix.
Symptoms of intestinal disease depend on the department. If it hurts in the navel area, it’s all in the small intestine, and if it hurts on the sides, it’s in the large intestine.
Non-pharmacological therapy
In combination with drug treatment of the disease, additional methods and techniques are recommended that speed up the healing process:
- physical activity within acceptable limits (for example, yoga). If you are overweight, it is also necessary to use programs to reduce your body mass index;
- dietary nutrition that excludes the use of poorly digestible substances, but includes foods enriched with soluble dietary fiber. In addition, it is necessary to exclude the use of products that cause gas formation;
- psychological consultations, stress management training programs.
Survey
Colonoscopy
- Cost: 25,000 rub.
More details
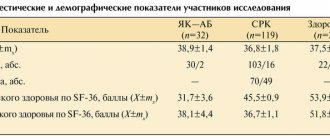
Diagnosis begins at a consultation with a gastroenterologist with examination and questioning. The nature of pain and discomfort and their duration play a big role. When diagnosing colitis, a whole range of instrumental studies is used:
- Colonoscopy. The most common endoscopic examination of the intestine.
- Sigmoidoscopy (examination of the rectum and anal area).
- Laboratory examination of stool (scatology, bacterial examination, inflammatory markers - calprotectin and others).
- X-ray examination using a contrast agent (irrigoscopy). Allows you to detect the exact localization of inflammation.
- Biopsy of the mucosa for histological examination. Allows you to clarify the diagnosis and exclude the possibility of a malignant neoplasm, which often manifests itself with the same symptoms as colitis.
Diagnostics is aimed at collecting the maximum amount of data about the disease. The doctor tries to find out the cause (it must be eliminated during treatment) and to clarify the localization of the inflammatory process. The more accurate the examination, the easier it is to choose effective treatment tactics.