Sabril (Vigabatrin)
pharmachologic effect
Antiepileptic drug. Irreversible selective inhibitor of GABA aminotransferase. Increases the concentration of GABA in synapses, thereby increasing inhibitory effects. Suppresses the increased excitability of neurons, which underlies the occurrence and spread of epileptic seizures.
Indications for the active substance VIGABATRIN
Partial seizures, West syndrome.
Dosage regimen
Orally for adults, 500 mg 2 times a day, if necessary, increase the dose to 1.5 g/day.
For children, an initial dose of 40 mg/kg/day is recommended; if necessary, the dose can be increased to 80-100 mg/kg/day.
Side effect
From the central nervous system and peripheral nervous system: anxiety, irritability, aggressiveness, psychotic disorders; rarely - headaches, nystagmus, tremor, paresthesia, impaired ability to concentrate, increased fatigue, visual field impairment; in isolated cases - an increase in the frequency of epileptic seizures, including status epilepticus.
Other: rarely - mild dyspeptic symptoms, weight gain; in isolated cases - swelling.
Contraindications for use
Pregnancy, lactation (breastfeeding), hypersensitivity to vigabatrin.
Use during pregnancy and breastfeeding
Contraindicated for use during pregnancy and lactation (breastfeeding).
Use for renal impairment
In elderly patients, especially with impaired renal function (creatinine clearance less than 60 ml/min), adjustment of the dosage regimen is required.
Use in children
Application is possible according to the dosage regimen.
Use in elderly patients
In elderly patients and especially with impaired renal function (creatinine clearance less than 60 ml/min), adjustment of the dosage regimen is required.
special instructions
Use with caution in patients with mental illness, a history of psychosis and behavioral disorders.
During treatment, careful medical monitoring is required to identify possible adverse reactions from the nervous system.
If it is necessary to discontinue treatment, it is recommended to gradually reduce the dose over 2-4 weeks. Sudden cessation of treatment may result in a recurrence of seizures.
Before starting and during treatment, periodic consultations with an ophthalmologist are required. If visual field defects are detected, the question of further use of vigabatrin is decided depending on the risk-benefit ratio of the therapy. In cases where the detection of visual field defects cannot be adequately performed (for example, in young children), the decision to treat with vigabatrin should be based on an analysis of clinical indicators that allow the risk-benefit ratio of treatment to be assessed.
In elderly patients and especially with impaired renal function (creatinine clearance less than 60 ml/min), adjustment of the dosage regimen is required.
Experimental studies have shown that vigabatrin causes reversible swelling of myelin sheaths. There is currently no evidence of the same phenomenon in humans.
Impact on the ability to drive vehicles and machinery
Use with caution in patients whose activities require high concentration and rapid psychomotor reactions.
Drug interactions
With simultaneous use, a decrease in plasma concentrations of phenytoin, phenobarbital, and primidone is possible.
Order a product
The use of anticonvulsants in pediatric practice
The history of drug treatment of epilepsy begins in the mid-19th century, when the anticonvulsant effect of bromides was discovered. Bromine salts suppressed generalized tonic-clonic seizures, but had a strong sedative effect and were toxic with long-term use [1]. Since the beginning of the 20th century. The first anticonvulsant drug from the group of barbiturates, phenobarbital, is widely used. Subsequently, other barbiturates came into practice - primidone (hexamidine) since 1952 and the domestic drug benzonal. However, the sedative effect of barbiturates was still too high. In 1937, the use of phenytoin began. A positive property of phenytoin was the lack of sedation; disadvantages included nonlinear kinetics and pronounced cosmetic side effects. Today, barbiturates and phenytoin are still produced and used in Russia, however, in most developed countries, drugs from these groups are considered obsolete and their use in pediatric practice is not recommended.
60s of XX century. — the time when in developed countries drugs that are now classified as basic anticonvulsants came into practice: valproate, carbamazepine, ethosuximide, benzodiazepines, sulthiam, acetazolamide. This generation of drugs gradually replaced the more toxic older anticonvulsants and dominated the market until the mid-1990s. Benzodiazepines subsequently moved into the category of drugs of the third or fourth line of choice due to the often developing tolerance of attacks to them.
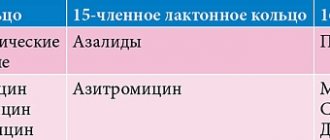
The 1990s saw the emergence of the so-called “new” anticonvulsants: oxcarbazepine, lamotrigine, vigabatrin, gabapentin, felbamate, topiramate, tiagabine, zonisamide, stiripentol (the drugs are listed in the order of their appearance on the market). Some of these drugs are registered in Russia, and not all of them are approved for use in children (Table 1). This review concerns the use of both basic and new anticonvulsants in pediatric epileptology. The daily dose of anticonvulsants in pediatric epileptology is calculated based on the patients' body weight. Dosages, including for outdated anticonvulsants, are given in Table 2.
Major anticonvulsants
Sodium valproate. The history of clinical use of valproate goes back more than 35 years, and during this time it has become one of the most popular anticonvulsants [2]. Valproic acid and its salts have a wide spectrum of action and can be prescribed for almost all forms of epilepsy as first-line drugs of choice, even before the form of the disease is clarified. An exception is West syndrome, in which valproate is significantly inferior in effectiveness to vigabatrin and hormonal therapy. The wide spectrum of action of the drug is usually associated with multiple mechanisms of action. Valproate has been reported to block voltage-gated sodium channels in neurons, however, unlike carbamazepine and phenytoin, it does not affect the restoration of the channel from an inactivated state. Valproate in high concentration acts on T-type calcium channels, reduces the concentration of aspartate and increases the level of GABA [3].
Valproates are also characterized by a low (2%) level of seizure aggravation [4]. The advantages of the drug include the ability, if necessary, to prescribe the drug immediately in the minimum therapeutic dose, bypassing a period of long titration. If the minimum therapeutic dose is ineffective, move to the intermediate and maximum doses before changing the drug or resorting to polytherapy. Since the effect of valproate may be delayed, the interval between dose increases should be 2 weeks to 1 month.
The pharmacy chain has a large number of children's (syrup, drops), divisible retardated forms (Depakine Chrono, Convulex Retard), and enteric forms (Depakine Enteric). Preference should be given to retardated forms, since taking the anticonvulsant twice a day is more convenient for the student’s parents. An individual dose should be prescribed per kg of body weight per day, but so that the daily dose can be easily selected using a measuring spoon or marks on a divisible tablet, since any inconvenience associated with taking the medicine leads to non-compliance (missing doses, unauthorized dose change). Long-term use of valproate requires monitoring of liver enzymes (ALT, AST), pancreas (amylase), and ammonium levels in the blood. An increase in ammonium levels occurs in 20–50% of patients and is most often asymptomatic, but in some cases it can manifest as symptoms of encephalopathy. Another serious complication of valproate therapy is hepatopathy, the risk of which is especially high in children under 2 years of age receiving polytherapy. L-carnitine is used as an antidote for valproic encephalopathy and hepatopathy [2].
The therapeutic concentration of the drug is 50–100 mg/l, but the need to measure it arises either during polytherapy together with enzyme-inducing drugs, or in case of resistance of attacks to therapy.
Carbamazepine. It is believed that carbamazepine (finlepsin, tegretol) stabilizes the voltage-dependent sodium channel in an inactivated state, but other mechanisms are also suggested [3]. Carbamazepine is effective in cryptogenic and symptomatic partial epilepsies (simple, complex and secondary generalized seizures), and isolated primary generalized tonic-clonic seizures. Its use in idiopathic generalized epilepsy is limited due to carbamazepine aggravation of absence seizures and myoclonus. In some cases, in the presence of secondary bilateral synchrony on the EEG in symptomatic frontal lobe epilepsy, carbamazepine is also capable of aggravating seizures.
The risk of atypical evolution associated with the use of carbamazepine has led to restrictions on the use of this drug in rolandic epilepsy. However, carbamazepine is highly effective in childhood occipital epilepsy with late onset (Gastaut form) and in autosomal dominant frontal epilepsy with nocturnal paroxysms [5]. Its structural similarity to tricyclic antidepressants allows it to be used in psychiatric practice; in addition, the drug is effective for trigeminal neuralgia.
In practice, it is important that carbamazepine is completely metabolized to carbamazepine 10-11-epoxide, while inducing microsomal liver enzymes. This means that, having decided on the target dose (in children, usually in the range of 10–30 mg/kg body weight per day), it is necessary to start with a prescription of about 5 mg/kg body weight per day and increase the dosage gradually to avoid dose-dependent side effects. The drug is capable of reducing the concentration of valproate, and although (for resistant partial epilepsies) it can be used in combination with them, such a scheme is not considered rational and may require monitoring the level of drugs in the blood. The therapeutic concentration of carbamazepine is 4–12 mg/l.
In pediatrics, divisible retardated forms of carbamazepine (finlepsin retard, tegretol CR) are convenient for use, allowing the drug to be prescribed 2 times a day, despite the short half-life of carbamazepine. During long-term treatment with carbamazepine, it is necessary to examine the child’s skin and mucous membranes and monitor hematological parameters. For timely diagnosis of secondary bilateral synchrony, control EEG studies should be performed.
Ethosuximide. The only mechanism of action of ethosuximide (Suxilep) is the blockade of voltage-dependent T-type calcium channels [3]. The uniqueness of this mechanism ensures its high effectiveness in absence seizures, both typical (in idiopathic generalized epilepsy) and atypical (in Lennox-Gastaut syndrome, atypical benign partial epilepsy, Landau-Kleffner syndrome, etc.). In addition, ethosuximide is effective for so-called “frontal absence seizures” and negative myoclonus. However, the drug is ineffective against generalized tonic, tonic-clonic and all types of partial seizures, which does not allow the use of ethosuximide as monotherapy; The most commonly used combination is ethosuximide and valproate, which has true synergism for absence seizures in children [2].
The advantages of the drug include the possibility of prescribing it immediately in a therapeutic dose, the disadvantages are the absence of pediatric and divisible forms in Russia.
New anticonvulsants
Lamotrigine. Lamotrigine (Lamictal) blocks voltage-gated sodium channels, but in a different manner than carbamazepine, as might be expected from the broad spectrum of action of this drug. Blockade of voltage-dependent calcium channels has also been reported, leading to a decrease in the excitatory effect of glutamate [1, 3]. The spectrum of action of lamotrigine includes all types of seizures and practically coincides with the spectrum of action of valproate. The interaction of these two drugs is synergistic, with valproate increasing the concentration of lamotrigine, which allows reducing the dose of the latter and thereby affecting the overall cost of treatment.
Disadvantages of lamotrigine include the development of skin rash (in 11% of children) and Stevens-Johnson and Lyell syndromes [1]. The risk of complications is reduced with slow dose titration, but this limits the use of lamotrigine as a first-line drug for newly diagnosed epilepsy. When prescribing the drug for the first time, it is necessary to increase the dose strictly in accordance with the instructions for use of the drug and teach parents to examine the child’s skin and mucous membranes daily. In the future, there will be no need for such control.
The positive properties of lamotrigine include a minimal effect on cognitive function compared to other anticonvulsants and a lower risk of developing ovarian cysts in patients or neural tube defects in a child from a mother with epilepsy than with other drugs [6–9].
Lamotrigine aggravates seizures in severe myoclonic epilepsy of infancy (Dravet syndrome) and is strictly contraindicated in this form. Isolated cases of increased myoclonus have been reported in juvenile myoclonic epilepsy, but this does not prevent the use of lamotrigine, along with valproate and topiramate, in this common form of epilepsy, especially in females.
Topiramate. Topiramate (Topamax) is considered one of the most promising anticonvulsants due to multiple mechanisms of action: blockade of voltage-gated sodium channels and voltage-gated calcium channels; enhancing the effect of GABA on GABAA receptors; blockade of excitatory mediators (glutamate); inhibition of carbonic anhydrase types II and IV [3].
The drug has been shown to have a neuroprotective effect in experimental status epilepticus [10]. Indications for the use of topiramate include most epilepsies and epileptic syndromes, with the exception of absence epilepsies: in this case, it is inferior to valproate. The effectiveness of topiramate in resistant forms of epilepsy is slightly higher than that of basic anticonvulsants [11, 12].
The disadvantages of topiramate include the need for slow titration of the dose (for children - no faster than 1 mg per kg of body weight per week). This titration is necessary to reduce the risk of side effects: hyperactivity, excitability, restlessness. On the other hand, slow titration allows you to more accurately select an individual dose, since the “therapeutic window” of the drug is very wide and control of attacks can be achieved either at a dose of 1 mg per kg of body weight per day or 10–15 mg per kg of body weight per day. The upper limit of the dose of topiramate is being specified and in children under 2 years of age it may be 20–25 mg per kg of body weight per day. During treatment with topiramate, it is necessary to monitor the condition of the kidneys.
Levetiracetam (Keppra). Like many new anticonvulsants, levetiracetam (there are several formulations of the drug on the market) was initially registered as a drug for the adjunctive treatment of cryptogenic and symptomatic partial epilepsies in adults. Subsequently, the drug turned out to be effective in idiopathic generalized epilepsy, including juvenile myoclonic epilepsy [13].
When studying the effectiveness of the drug in children, an increase in concentration was noted as a positive effect in 25% of cases. The most common side effects were excitability and aggressiveness [14].
The mechanism of action of levetiracetam remained unknown for a long time, but recently it was found that levetiracetam binds to the presynaptic protein SV2, located in synaptic vesicles. The function of the protein has not been fully elucidated, but the unique mechanism of action of levetiracetam and its structural similarity to piracetam explain the differences in the spectrum of action of levetiracetam and other new anticonvulsants. Levetiracetam, as monotherapy or in combination with piracetam, effectively relieved myoclonus in patients with Unferricht-Lundborg disease and other progressive myoclonic epilepsies [15–17]. Despite the fact that in Russia the drug is not registered for use in children, its earliest possible use both in progressive myoclonus epilepsy and in the treatment of children with non-progressive myoclonic status (Angelman syndrome, posthypoxic myoclonus) seems promising [15].
Rapid dose titration is possible, but to date the dosage limits in pediatrics have not been precisely defined, and there are also isolated reports of paradoxical reactions when taking high doses of levetiracetam.
In conclusion, it should be noted that today the anticonvulsant market in the Russian Federation offers a sufficient number of drugs for the treatment of most forms of epilepsy in children. A limiting factor is the high cost of treatment with new anticonvulsants. At the same time, niches for the use of drugs effective in certain forms of childhood epilepsy remain unfilled. This is vigabatrin (Sabril) - effective for West syndrome (infantile spasms), especially for tuberous sclerosis; sulthiam (ospolot) is a drug effective for syndromes combined with electrical status epilepticus of slow-wave sleep (Landau–Kleffner syndrome, etc.) and Rolandic epilepsy; Clobazam (Frisium), the benzodiazepine with the lowest degree of tolerance. Apparently, the issue of registration of these drugs in Russia should be raised by associations of neurologists and parent organizations.
A. Yu. Ermakov, Candidate of Medical Sciences Moscow Research Institute of Pediatrics and Pediatric Surgery, Moscow
For questions regarding literature, please contact the editor.
Medical Internet conferences
Tuberous sclerosis is a genetically determined disease, belongs to the group of neuroectodermal disorders, characterized by damage to the nervous system, skin and the presence of hamartomas in various organs. Inherited in an autosomal dominant manner.
Clinical case: patient M., 2 years 1 month, was admitted to the clinic with a diagnosis of tuberous sclerosis. Symptomatic epilepsy. Subependymal giant cell astrocytomas of the lateral ventricles of the brain. Multiple cardiac rhabdomyomas.
History: a child from the 2nd pregnancy, which proceeded without any peculiarities, physiological birth at 38 weeks. The family history is not burdened. Sporadic case. According to ultrasound data at the 30th week of gestation, fetal heart rhabdomyoma and tuberous sclerosis were diagnosed? At birth, on the skin in the area of the left buttock there are 2 pigmented spots 3-5 mm, on the anterior surface of the abdominal cavity 1 spot 1.5 by 0.5 cm. In the shoulder area on the right there is a small area like shagreen skin, dense consistency, yellowish-brown color, protrudes moderately above the surface of the surrounding skin.
On ECHO-KG: multiple rhabdomyomas.
At 4 months Nodding movements of the head appeared, after 2 weeks flexor spasms appeared, after 2 weeks the attacks spontaneously stopped. At the age of 6 months, he notes the appearance of “freezing”, with the eyes and head moving to the left, muscle tension in the trunk and limbs, lasting up to 2 minutes, up to 2 times a day. There was a developmental lag. Anticonvulsant therapy was prescribed: Depakine Chronosphere 100 mg-2 times a day, against the background of which positive dynamics were achieved. At 7 months An MRI scan of the brain confirmed the diagnosis of tuberous sclerosis. At 7.5 months. Serial attacks of tonic tension appeared, up to 20 attacks in a series. Sabril (a selective irreversible inhibitor of GABA transaminase) was introduced into therapy - the attacks were stopped at a dose of 500 mg per day, ½ tablet in the morning and evening after 12 hours. There have been no attacks since 02/14/15. Currently - psychomotor development according to age.
Results: Sabril provided a lasting and positive effect, the attacks stopped, and the girl’s condition improved. The general condition is satisfactory, consciousness is clear. Understands spoken speech according to age. There are no cerebral or meningeal symptoms. Head circumference 47.5 cm. Movement of eyeballs: full. There is no nystagmus. The exit points of the trigeminal nerve are painless. The face is symmetrical. The hearing is preserved. Tongue in the oral cavity in the midline. Head in the midline. Passive movements in full, active movements in full. Muscle strength is preserved. Muscle tone is preserved. Tendon reflexes are preserved.
International Neurological Journal 5(21) 2008
In pediatric neurology, one of the most difficult problems is the problem of infantile spasms, the frequency of which in children can reach up to 250 attacks per day. Treatment of patients with West syndrome is associated with a number of difficulties.
We are monitoring 10 patients with West syndrome aged from 2 months to 3 years, receiving vigabatrin (Sabril) and synacthen depot. Convulsions in young children were represented by infantile spasms, and were also combined with myoclonus, focal paroxysms, and generalized general seizures, which debuted at the age of 1 to 6 months. With the onset of seizures, all children experienced developmental delay. These patients were observed for epileptic syndrome with seizures resistant to therapy. The frequency of episodes during the day varied from 5 to 30, in a series there were up to 64 infantile spasms, the maximum number of attacks per day was up to 242. In three children, the onset of convulsive syndrome coincided with the start of vaccination. All children underwent a comprehensive clinical examination, including EEG, MRI of the brain, ECG, EchoCG, ultrasound of internal organs, examination for a group of intrauterine infections, and consultation at a medical genetic center. An EEG revealed the presence of hypsarrhythmia, high-amplitude complexes of peak and polypeak waves, and spike waves, which confirmed the diagnosis of West syndrome. Previous therapy was not effective.
The introduction of Sabril into therapy in combination with synacthen depot made it possible to achieve relief of attacks in 6 children, while there was an improvement in cognitive functions and positive dynamics according to EEG data. It was possible to achieve a reduction in seizures, reduce their severity and improve cognitive functions in 4 children (in this group there was a combination of infantile spasms with other types of seizures).
Here is an example of a clinical observation. Patient B.D., 9 months. The onset of the disease is from 4 months in the form of series of infantile spasms, up to 5–7 episodes per day (the frequency of infantile spasms in a series is up to 15–19), accompanied by severe anxiety in the child. With the onset of seizures, the child experiences delayed psychomotor development. During anticonvulsant therapy, the frequency of attacks remained high (up to 19–22 episodes per day, the frequency of infantile spasms in a series - up to 64, per day - up to 242). From the anamnesis it was established: a child from the first pregnancy with toxicosis, nephropathy, hyperglycemia, first term birth, body weight - 3600 g, OSHA 8-9 points, breastfed. Vaccinated up to 4 months. Neurological status on admission: head circumference - 44 cm. The child's condition is severe due to the disease. Vyalovat. Restless from time to time. Severely retarded in development. He holds his head, watches for a short time, does not roll over, does not sit, does not reach for a toy, the support on his legs is weak. The large fontanel is not tense. Palpebral fissures D = S, pupils are equal. Ng no. Movement of the eyeballs is not noticeably limited. Slight asymmetry of nasolabial folds. Muscle tone in the limbs is dystonic. Tendon reflexes are increased D > S.
The child was examined in the clinic with an ECG, echocardiography, ultrasound of internal organs, and examined for intrauterine infections. EE mapping in June 2008: Dream. Sleep phases are not determined. Throughout the entire recording, there is an alternation of low-amplitude slow-wave polymorphic activity with periods of high-amplitude slow polymorphic waves in combination with discharges of spike waves and sharp waves, without clear localization. Hypsarrhythmia can be assumed, because During sleep, the hypsarrhythmia pattern resembles the burst-suppression pattern. MRI of the brain 07/03/2008: irregularly shaped zones are visualized in the white matter of both hemispheres, periventricular and subcortical. The midline structures are not displaced. Moderate expansion of the lateral ventricles of the brain up to 1.0 cm, intrathecal spaces are markedly expanded in the temporo-frontoparietal regions on both sides (up to 0.8 cm). An S-shaped tortuosity of the extracranial sections of both internal carotid arteries is determined, with the presence on the left in the area of tortuosity of an area of moderate decrease in the intensity of the MR signal (due to changes in blood flow in the area of tortuosity (?)). Moderate tortuosity of the extracranial sections of both VAs is also noted. Conclusion: the above-described areas in the brain may be due to incomplete myelination (control over time). Moderate expansion of the lateral ventricles of the brain. Marked expansion of the intrathecal spaces. S-shaped tortuosity of both ICAs, tortuosity of both PAs.
Therapy was carried out: Depakine syrup (40 mg/kg per day), Sabril (60 mg/kg per day, dexamethasone, synacthen depot, asparkam, diacarb, nicotinic acid. After the introduction of synacthen depot into therapy, the attacks stopped. After stopping the attacks, the child monitors more actively , walks, plays with toys.
EE mapping 09/09/2008: Wakefulness. A slow-wave EEG is recorded with a predominance of delta activity and without signs of local pathology. It was not possible to register any signs of paroxysmal activity at the time of the examination. Functional immaturity.
The child was discharged from the department in satisfactory condition. Remission 1.5 months.
Thus, in the treatment of infantile spasms, the drugs of choice are: depakine 30–50 mg/kg per day or vigabatrin (Sabril) at a dose of 40–80 mg/kg per day in combination with hormonal therapy - synacthen depot at a dose of 0.15 ml per day and further according to the scheme. This combination demonstrated high effectiveness in children with West syndrome and contributed to remission of attacks up to 2 years of age, and improved development and cognitive functions in children.
The court ordered the issuance of Sabril, unregistered in Russia, to three girls
The Ryazan district court ordered the regional Ministry of Health to issue the drug Sabril, unregistered in Russia, to three seriously ill girls, the Ryazan Memorial society reported.
“For more than a year, the girls’ mothers, together with our lawyer Petr Ivanov, sought the issuance of the drug Sabril, which is needed to reduce the frequency of epileptic seizures. Due to the fact that in order to purchase a medicine that is not registered in Russia, a complex procedure must be launched, the Ministry of Health refused to parents under various pretexts, but the court considered this position of the ministry illegal,” the statement says.
As Miloserdiy.ru was told by the Ryazan Memorial Society, one package of Sabril lasts a patient 25 days. Its cost reaches 7,000 rubles. You need to take the drug constantly.
According to the court decision, the ministry must begin purchasing the medicine immediately, since delay poses a threat to the health of children, local media reports. “For parents, such a court decision is a big victory, but the decision is important for the Ryazan region and Russia as a whole. For a long time, the Ministry of Health ignored the law and refused to recognize that these children have the right to free Sabril provision. We hope that now seriously ill people who are prescribed drugs unregistered in Russia for medical reasons will be able to receive medications in a timely manner according to the legal procedure, and not spend several months on prosecutors’ offices and courts, as in this case,” noted Petr Ivanov , who represented interests of parents in court.
Earlier, Pyotr Ivanov explained to Miloserdiyu.ru what regulations parents of seriously ill children rely on when seeking to provide them with unregistered medications. “After a law was passed at the end of 2014 that introduced articles into the Criminal Code and the Administrative Code prohibiting the import of unregistered drugs into Russia, parents for some time could not receive such drugs at all, fearing suspended sentences and huge fines. Then the Ministry of Health gave an explanation and said that you can import it for personal use. That is, parents can go abroad on their own, buy medicine and bring it back for their child. Naturally, only a few have that kind of money,” Ivanov said.
However, there is an order of the Ministry of Health dated August 9, 2005 No. 494 “On the procedure for using medicines in patients for health reasons.” “This document says that if a drug is needed for health reasons (without it there will be a serious deterioration in health or even death), then a council of doctors can prescribe it,” the lawyer explained.
“If the council prescribed such a drug, then another norm will apply here - Article 80 of the federal law “On the fundamentals of protecting the health of citizens,” he continued. – This article clearly states that drugs that are not included in the list of vital and essential drugs are not subject to payment at the expense of citizens’ personal funds if they are replaced due to individual intolerance for health reasons.
That is, if it is impossible to prescribe a drug included in the list of free drugs, and this drug is needed for health reasons, then it is provided free of charge.”
If a medicine is prescribed to a child for health reasons, even if it is not registered in Russia, it can be prescribed, and the state is obliged to provide it, summarized Pyotr Ivanov.
Only last one year!