The liver is the largest biochemical laboratory in our body. It is involved in more than 500 reactions. Therefore, any changes in her condition may affect her well-being. Everyone knows its important role and has heard about such a terrible diagnosis as cirrhosis, many want to clean it and take special medications. Some are looking for folk remedies, others trust more in the developments of the pharmaceutical industry. The question remains, what will actually be effective?
Get all the necessary tests at a discount of 10% to 25% using the promotional code “MOESHEALTH”. Visit one of the many conveniently located KDL medical offices https://bit.ly/3gIM9wP or call a nurse for free to collect biomaterial using the innovative laboratory service LifeTime https://bit.ly/3yd9Pj2
Composition and release form
| Pills | 1 table |
| Powders: | |
| spiny capers (Capparis spinosa) | 65 mg |
| common chicory (Cichorium intybus) | 65 mg |
| Mandur bhasma (iron oxide) | 33 mg |
| black nightshade (Solanum nigrum) | 32 mg |
| Terminalia arjuna | 32 mg |
| Western Cassia (Cassia occidentalis) | 16 mg |
| common yarrow (Achillea millefolium) | 16 mg |
| Gallic tamarisk (Tamarix gallica) | 16 mg |
| extracts processed over steam from a mixture of the following plant materials: white eclipta (Eclipta alba), phyllanthus niruri (Phyllanthus amarus), spreading berhavia (Boerhaavia diffusa), Tinospora cordifolia, radish (Raphanus sativus), emblica officinalis ), Plumbago zeylanica, Embelia ribes, Terminalia chebula, Fumaria officinalis | |
| excipients: magnesium stearate; MCC; croscarmellose sodium; sodium carboxymethylcellulose |
in plastic bottles of 100 pcs.; 1 bottle in a cardboard box.
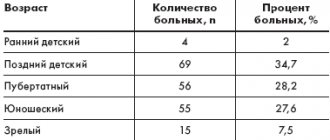
Experience of using Liv.52 in pediatric practice (Literature review)
F
armacotherapy of diseases of the liver and biliary system of children and adolescents is one of the most pressing problems of pediatric gastroenterology. It requires the creation of new effective treatment regimens. Diet therapy, the use of psychotherapeutic methods, the prescription of drugs with a wide range of therapeutic effects, and the treatment of diseases against which biliary tract dysfunction has developed remain relevant.
To optimize treatment, it is necessary to use drugs that have a complex effect on the pathological process. Thus, the tactics of drug treatment for dysfunctional disorders of the biliary tract cannot be standard. Treatment should be comprehensive, depending on the form of the disorder and the nature of the concomitant pathology of the digestive tract. The use of herbal preparations that exhibit both choleretic and hepatoprotective effects is promising.
One of the well-proven medicines that can be used in children from an early age is the herbal preparation Liv.52, available in drops and tablets. This is a herbal preparation that does not contain alcohol or dangerous chemical components. The plants that make up Liv.52 are well known and grow in the territory of central Russia and in the countries of Central Asia (prickly caper, common chicory, black nightshade and common yarrow). Liv.52 has a choleretic, appetite-improving, diuretic, antitoxic, antioxidant, and anti-inflammatory effect [2,3,13].
In 2002–2004 In the leading gastroenterological centers of Moscow, St. Petersburg, Yekaterinburg, Saratov and Nizhny Novgorod, independent scientific studies were conducted on the effectiveness of the drug Liv.52 in more than 300 children and adolescents with hepatitis and biliary dysfunction. The research results confirmed the high effectiveness of the drug in diseases of the liver and biliary tract and identified the mechanisms of the positive effect of Liv.52 on the structure of bile. All studies noted a positive correlation between clinic data and the results of biochemical and ultrasound examinations of patients.
V.F. Uchaikin et al. studied the use of the drug Liv.52 for acute hepatitis A (moderate, mild form) and chronic viral hepatitis B and C in children. It is known that in the pathogenesis of acute and chronic viral hepatitis, the central link is the cytolysis syndrome, which is usually understood as an increase in the permeability of hepatic-cellular and subcellular membranes, which leads to the loss of biologically active substances by hepatocytes, primarily hepatic-cellular enzymes and, as a consequence, , to disruption of all types of metabolism, including biological oxidation processes: conjugated bilirubin in the blood increases, the synthesis of albumin and blood clotting factors decreases, the excretion and passage of bile into the intestines is disrupted, which, in turn, leads to disruption of the digestion processes and absorption of vital substances . Consequently, in all forms of both acute and chronic viral hepatitis, the prescription of drugs aimed at stabilizing cell membranes and restoring the passage of bile is pathogenetically justified [4,11].
In practical work, Essentiale, Phosphogliv, Legalon, Seripar, Flamin, choleretic preparations, etc. are usually prescribed for this purpose. There is some experience in using the drug Liv.52 in tablet form for this purpose. In previous years' work, it was shown that Liv.52 has a fairly pronounced hepatoprotective effect, stabilizes hepatic cell membranes, improves metabolism, and enhances the passage of bile into the intestines [5,6]. In recent years, a new form of Liv.52 K in drops has appeared on the domestic drug market.
70 sick children aged from 4 to 14 years were under observation. Of these, 30 children were diagnosed with hepatitis A (HA): 22 had a moderate form, 8 had a mild form. 40 patients had chronic hepatitis: 13 had chronic hepatitis B, 27 had chronic hepatitis C.
For hepatitis A (18 children), children received Liv.52, 1 tablet 3 times a day for 14 days. For hepatitis B and C (20 children) - 1 tablet 3 times a day for 30 days or 10 drops 3 times a day also for 30 days. The control group of children (32 children) received standard basic choleretic therapy with nicodine, cholenzyme, and pancreatin.
Observations showed that under the influence of Liv.52, children with acute hepatitis A had more favorable dynamics of clinical and laboratory parameters than in the control group. Thus, a decrease in the symptoms of intoxication (weakness, lethargy) occurred on the very first day of treatment with Liv.52, jaundice subsided on the 5th day, and on the 6th day from the start of treatment the size of the liver decreased. Particularly significant was the weakening of skin itching, which occurred almost on the very first day of taking Liv.52. In patients in the control group, this symptom weakened only on the 6th day from the start of observation. A decrease in the severity of other symptoms in patients in the control group was observed 1–2 days later than in patients receiving Liv.52. In patients receiving Liv.52, intoxication symptoms disappeared within 2 days after starting to take the drug Liv.52, jaundice disappeared after 11 days, and the size of the liver normalized within the same period. In patients in the control group, the disappearance of hepatitis symptoms lagged behind those in the experimental group by 1–4 days. As for skin itching, it disappeared on the 4th day of treatment with Liv.52, while in the control group it disappeared only on the 8th day of observation (Fig. 1).
Rice. 1. Disappearance of symptoms of acute hepatitis when taking Liv.52 and in the control group
It was noted that biochemical parameters in patients with acute hepatitis who received Liv.52 normalized faster than in patients in the comparison group (Fig. 2,3).
Rice. 2. Dynamics of total bilirubin levels during treatment with Liv.52 (acute hepatitis A)
Rice. 3. Dynamics of ALT parameters during treatment with Liv.52 (acute hepatitis A)
During treatment with Liv.52, clear positive dynamics in the biliary tract were also revealed. There was a significant decrease in the manifestations of hypomotor dyskinesia, which was expressed in the subsidence of cystic symptoms and normalization of ultrasound parameters: restoration of reduced contractile function of the gallbladder, reduction or disappearance of sediment in the cavity of the gallbladder.
Researchers also note the positive effect of Liv.52 on reactive pancreatitis in patients with acute hepatitis. In patients with chronic hepatitis B and C in combination with severe somatic pathology, during treatment with Liv.52, a significant decrease in the frequency of intoxication symptoms (headache, lethargy, nausea, abdominal pain, loss of appetite) was observed. Under the influence of Liv.52, the frequency of manifestations of hypomotor dyskinesia of the gallbladder, cholecystitis, and reactive pancreatitis decreased in patients in this group (Fig. 4).
Rice. 4. Dynamics of the state of the biliary system in patients with CHB and CHC during treatment with Liv.52
Thus, a wide range of positive effects of the drug Liv.52 on the course of acute and chronic viral hepatitis in children and adolescents was identified [7,10].
Along with acute and chronic hepatitis, the diagnosis of biliary dyskinesia (BDSD) remains widespread. The clinical symptoms of ADHD are often regarded by pediatricians without sufficient grounds as an organic pathology, for example, chronic cholecystitis or chronic pancreatitis. As a result, antibacterial, anti-inflammatory and other therapy is prescribed that is inadequate and ineffective in these situations.
Shabunina E.I. et al. conducted an assessment of the effectiveness of the use of the drug Liv.52 (drops, tablets) in 30 children suffering from chronic gastroduodenitis combined with hypotonic type GIVP. Liv.52 was used according to the recommended doses - for preschool children, 10 drops 2 times a day for 30 minutes. before meals, schoolchildren take 2 tablets 2 times a day 30 minutes before. before meals. The course of therapy was 15–20 days. The dynamics of complaints and the results of an objective examination of children during treatment are presented in Tables 1 and 2.
In 54.5% of children treated with Liv.52, an increase in the initially reduced contractile function of the gallbladder was found (according to ultrasound data). The study of biochemical blood parameters indicated a tendency towards a decrease in indirect markers of cholestasis - alkaline phosphatase (from 3.67 to 3.21 μkat/l) and g-glutamyl transpeptidase (from 0.34 to 0.29 μkat/l). In 57% of children, a decrease in initially elevated urine urobilin was noted.
Thus, the results of the study convincingly showed that the use of the drug Liv.52 (tablets, drops) in children with chronic gastroduodenitis in combination with hypotonic type GIVP helps to relieve abdominal pain and dyspeptic syndromes, increase the contractile function of the gallbladder, and reduce cholestasis in the blood and urine (g-GTP, alkaline phosphatase, urobilin).
Researchers note a significant increase in the effectiveness of therapy when Liv.52 is included in the treatment regimens for sick children with gastroduodenitis combined with hypotonic type GIVP in 64% of patients. Good tolerability of the drug was noted in 100% of cases [9].
The high effectiveness of Liv.52 for hypomotor dyskinesia of the gallbladder is also confirmed by studies by Pisarev A.G. et al. Before treatment, ultrasound in all children visualized an enlarged gallbladder with sediment occupying from 1/3 to 1/2 of the volume of the bladder cavity. Contractile function after a choleretic breakfast was reduced. The control group of children received traditional choleretic drugs (Flamin, Cholenzym, Nicodine). The experimental group of children received Liv.52 at a dose of 1–2 tablets. 3 times a day for 14 days. In 63.9% of children receiving Liv.52, there was a pronounced positive dynamics of ultrasound signs of hypomotor dyskinesia. In all children, the contractile function of the gallbladder increased, and in half of the children the sediment in the bladder cavity disappeared completely, and in the rest it decreased significantly. The study found that Liv.52 has a choleretic effect with a choleretic effect. It was also noted that with the use of Liv.52, clinical signs of hypomotor dyskinesia disappeared in 54.4% of children and ultrasound signs in 63.9% of examined patients, while in the control group receiving traditional choleretic drugs (Flamin, Cholenzyme, Nicodine), positive dynamics were noted only in 13.1% and 6%, respectively [12].
The effectiveness of the drug for diarrhea has been confirmed by a number of studies conducted at the Saratov State Medical University under the leadership of prof. Eiberman A.S. The study included 20 children of the main group and 10 children of the control group aged 3–15 years. Patients in the main group received the drug Liv.52 in two dosage forms: drops and tablets in age-specific dosages 3 times a day for a course of 2 weeks. Patients in the control group received flamin in age-specific dosages for a course of 2 weeks. The effectiveness of therapy was assessed based on drug tolerability, dynamics of complaints, clinical manifestations, biochemical parameters and ultrasound examination. Researchers have not recorded a single case of intolerance to the drug Liv.52. A higher clinical effectiveness of the drug Liv.52 was noted compared to Flamin, which was expressed in a more rapid relief of the manifestations of the disease. Dyspeptic and pain syndrome in all children of the main group was relieved on days 3–4 of therapy, in the comparison group – on days 5–6. Blistering symptoms and pain in the right hypochondrium during the use of Liv.52 disappeared by 5–7 days, in the control group by the 10th day of therapy. During a control study of biochemical parameters after 2 weeks, their normalization was noted in children receiving Liv.52. After 2 weeks of Flamin therapy, 100% of children maintained elevated levels of alkaline phosphatase. Based on the results of clinical observation, it was concluded that the drug Liv.52 has a good choleretic and hepatoprotective effect and is the drug of choice for the hypomotor variant of biliary dyskinesia in children
[14].
It is known that children who have had hepatitis are at high risk of complications from the liver and gallbladder. Prevention of these complications is an urgent task in pediatric gastroenterology. Muravyova N.N. studied the effectiveness of Liv.52 in children at risk for cholelithiasis. During long-term follow-up and clinical and biochemical examination of children who had viral hepatitis, biliary dyskinesia was identified with the highest frequency among chronic gastrointestinal pathologies: in the immediate follow-up in 97.7%, 1–2 years after viral hepatitis - in 76.9 % of children. Ultrasound examination and cholecystography data in 45.8% of cases in patients who had viral hepatitis revealed biliary sludge and thick parietal bile in the gallbladder, indicating a change in the lithogenicity of bile. In this regard, a crystallographic study of bile was carried out to reveal changes in its colloidal properties. When comparing data on changes in the colloidal properties of gallbladder bile in children receiving therapy with Liv.52 and in children in the control group not receiving the drug, it was revealed that in children receiving Liv.52, in 60% of cases the gallbladder bile was homogeneous (isotopic) structure without signs of crystal formation, and only in 30% of cases in patients in this group by the end of the day dendritic structures like “fern leaves” were formed. In children at risk for cholelithiasis who did not receive Liv.52, hard crystals were detected 6 times more often than in the main group, and an undifferentiated pattern of crystallization was established in 25% of children in this group, which is the onset of stone formation (Fig. 5). A study of lipid metabolism revealed that in the group of patients receiving Liv.52, there was a significant decrease in blood a-cholesterol (1.04±0.01 mmol/l, versus 1.36±0.07 mmol/l in the control group) , as well as b-lipoproteins and triglycerides in the blood serum.
Rice. 5. Crystallographic picture of bile in VG convalescents (in%) during treatment with Liv.52
The data obtained for the first time established the possibility of using the drug Liv.52 in children with dyslipidemia, which is a serious risk factor for the early occurrence of cholelithiasis against the background of severe disorders of gallbladder motility in CH convalescents.
Data obtained by N.N. Muravva indicate a high risk of cholelithiasis among patients who have had viral hepatitis and have various pathologies of the gastrointestinal tract. This study clearly shows the effectiveness of the preventive effect of the drug Liv.52 on the process of initial stone formation. The mechanism of influence of the herbal preparation Liv.52 on the lithogenicity of bile, established for the first time, explains the effectiveness of the drug in disorders of the digestive processes at various levels of the gastrointestinal tract and confirms that Liv.52 has a convincing preventive effect against the threat of cholelithiasis in children [1].
Aronskind E.V. assessed the effectiveness of Liv.52 in the treatment of prolonged jaundice in premature infants (more than 18 days). The relevance of hyperbilirubinemia in newborns is determined by the high incidence of this pathology in the neonatal period (in 65% of all newborns). Optimization of treatment affects the prognosis of hyperbilirubinemia: from the development of deep metabolic disorders in the newborn’s body and changes in its functional state to residual neurological disorders in the form of cerebral palsy.
Depending on the use of Liv.52 and phenobarbital in the treatment of jaundice, all children were divided into 3 groups: children receiving Liv.52 and phenobarbital; children who received only Liv.52; control group receiving phototherapy and infusion therapy. Liv.52 was prescribed after 18 days of life, 5 drops 3 times a day for 3 weeks. Data were obtained allowing the conclusion that Liv.52, in the form of monotherapy or in combination with phenobarbital, promotes a gradual decrease in serum bilirubin levels. In no case was there an increase in the activity of alanine and aspartate aminotransferases. The average weight gain of newborns receiving Liv.52 during the study period was significantly greater than in the control group. Dynamic ultrasound examination of the liver, carried out weekly, revealed that by the end of the second week of treatment there was a significant decrease in liver size in children receiving Liv.52 compared to the control group. It should be noted that in the control group and after the end of the observation period there were no significant positive ultrasound dynamics in the condition of the hepato-biliary system [8].
Conclusion
Thus, an analysis of the comparative effectiveness of the use of Liv.52 (drops, tablets) in more than 300 children aged 18 days to 14 years with various pathologies of the liver and gallbladder indicates the high effectiveness of the drug and the pathogenetic validity of its use in comparison with traditional treatment acute and chronic hepatitis and hypomotor dyskinesia of the gallbladder in children and adolescents. At the same time, all researchers note that the drug is well tolerated. There were not a single case of allergic reactions or side effects.
The data obtained are consistent with data obtained by other clinicians who studied the effect of Liv.52 on the pathological process in patients with viral hepatitis, and allow us to recommend this drug for the treatment of acute and chronic viral hepatitis in children and adolescents. Liv.52 is also an effective and safe drug for the treatment of children with hypomotor dyskinesia of the gallbladder. It is advisable to include Liv.52 in complex treatment of patients who have had viral hepatitis and have chronic pathology of the digestive organs, in order to prevent the formation of stone formation in the gallbladder.
Research data indicate the effectiveness of Liv.52 in treating decreased appetite and low body weight in young children. The use of Liv.52 helps restore the protein-synthetic function of the liver, reduce the level of transaminases, bilirubin, reduce the symptoms of nausea and vomiting, normalize stool, relieve dyspepsia, a feeling of heaviness and pain in the right hypochondrium.
It should be noted that Liv.52 K in the form of drops is a convenient dosage form for use in pediatrics.
The drug does not contain alcohol, is easy to dose, and tastes good. Literature:
1. Muravyova N.N. The effectiveness of Liv.52 in children at risk for cholelithiasis.// Hospital – 2001 – No. 12 – p.11
2. Loverdo R.G., Rakovskaya R.L., Titrova E.Z. and others. The use of hepatoprotectors (Liv.52) in the treatment of children with acute intestinal infections. // Hospital - 2000 - No. 4. – p.13
3. Reddi JR, Sudhakar R., Robini K., Kusnena G. The management of viral hepatitis in children.//Indian Pediatrics. – 1975. – v.8 – p.659–665
4. Exhibition G.V. Viral hepatitis with cholestasis syndrome in children: Author. Diss. Ph.D. – M., 2000. – 21 p.
5. Sarchaeva V.G., Lupanova R.I., Use of Liv.52 for viral hepatitis in children.//Sb. theses “Treatment of infectious diseases in children” – 1982. – pp. 35–40
6. Mukhina N.V., Tyurina O.V., Paramonova O.A., Petrov V.A. Use of Liv.52 in complex therapy of viral hepatitis in children. //Materials of the VIII Congress “Man and Medicine”, Moscow. – 2001. – p.195
7. Uchaikin V.F., Cherednichenko T.V., Chaplygina G.V., Pisarev A.G. Liv.52 - a new look at the effectiveness of acute and chronic viral hepatitis in children. // Children's infections - 2003 - No. 3 - pp. 41–44.
8. Aronskind E.V. Hyperbilirubinemia in newborns.//Abstracts for the 2nd Congress “Mother and Child”, Moscow, 2003.
9. Shabunina E.I., Lavrova A.E., Dmitrieva G.V. The effectiveness of using the drug Liv.52 in children with gastroduodenobiliary pathology // Abstracts for the 2nd Congress “Mother and Child”, Moscow, 2003.
10. Cherednichenko T.V., Chaplygina G.V., Chaplygina G.V., Smirnov A.V., Kovalev O.B. Experience of using the drug Liv.52 to improve the quality of life in acute and chronic viral hepatitis in children // Abstracts of the X Russian National Congress “Man and Medicine”, Moscow, 2003, p. 404.
11. Blyuger A.F., Novitsky I.N. Practical hepatology. – Riga: Zvaigzne, 1984 – 405 p.
12. Pisarev A.G., Faingerts G.B. Ultrasound diagnosis of gallbladder lesions in the cholestatic form of acute hepatitis A and B. // Children's infections - 2002 - pp. 68–71.
13. Coche G., Sevenet F., Desombes P. et al. Cholestatic viral hepatitis with portal adenopathia.//Ann.Radial. – 1990. – v.33 – N3.–p.209–210
14. Eiberman A.S., Shulgina E.N., Chapurina T.A., Sukhova T.G. Influence – The influence of hepatoprotectors on the motility of the gallbladder in children // Abstracts in the materials of the 9th Russian conference “Hepatology today”, Moscow, 2004.
Drugs
Liver problems can develop for more than 10 years and not bother you at all. The average life expectancy with a diagnosis of cirrhosis is 9 years. Therefore, even if you have liver problems, you can fight them. There are about 1000 types of drugs used in hepatology. Therapy not only treats the disease itself, but also supports the liver in order to create the most favorable conditions for recovery. One of these groups of drugs are hepatoprotectors. Hepatoprotectors help restore metabolic processes in the liver, increase the organ’s resistance to destructive factors, normalize functional activity and stimulate regenerative processes in the liver.
Requirements for hepatoprotectors
Since the liver is the organ through which many substances are exchanged, drugs must not only be powerful, but also meet certain safety requirements, as well as:
- well absorbed;
- have a “first pass” effect through the liver;
- have the property of neutralizing or preventing the formation of substances that damage the liver;
- reduce the activity of inflammatory processes;
- slow down scar formation;
- help liver regeneration;
- do not cause rejection in case of liver pathology;
- extensive enterohepatic circulation;
- have no toxic effect.
Despite the fact that the requirements are known, the ideal drug has not yet been created. More than half of the presented products are of plant origin, the rest is divided between phospholipids, synthetic derivatives, organic preparations and amino acids.
Despite the fact that the requirements for liver drugs are known, the ideal one has not yet been created.
Conclusion
There are many hepatoprotectors, they differ in composition and mechanism of action. Doctors have an ambiguous attitude towards them; many of them are used and produced only for the territory of post-Soviet countries. Sometimes you can find reviews that a person, after quitting an alcohol binge, drank a certain drug for 3 months and his tests improved. This could have happened not because of the drug, but because the toxins stopped affecting the liver, and it was able to recover to a certain extent.
When exposure to toxins ceases, the liver itself can recover to a certain extent.
The main thing in treating the liver is not taking medications to compensate for the damage we cause ourselves, but stopping exposure to toxins and other destructive factors. That is, you need to give up alcohol, smoking and extra pounds (the risk of non-alcoholic fatty hepatosis). Because by alternating courses of medications with an unhealthy lifestyle, we create the illusion of well-being. If you suspect that something is wrong with your liver, be sure to consult a doctor. Incorrect self-medication for liver problems can only cause harm.
Read also[edit | edit code]
- Allohol
- Field artichoke
- Sandy immortelle
- Betaine
- Gepabene
- Hepa-Merz (Ornithine-aspartate)
- Heptral (Ademethionine)
- Dymyanka
- Calendula
- Karsil (Silymarin)
- Coriander
- Corn silk
- Chime
- Legalon
- Lecithin
- Tansy
- Milk thistle
- Remaxol
- Rosanol
- Siromin
- Tykveol
- Pumpkin seeds
- Flamin
- Holagol
- Holenzym
- Holosas
- CBB (betaine bofur citrate)
- Cynarin
- Essentiale