Indications
Neurotic, neurosis-like, psychopathic and psychopath-like states, accompanied by anxiety, fear, increased irritability, tension and emotional lability; sleep disorders, obsessive-compulsive disorder, panic disorder, phobias, reactive psychosis; autonomic lability, hypochondriacal-synestopathic syndrome; convulsive seizures of various etiologies, temporal and myoclonic epilepsy, status epilepticus, muscle rigidity, tic, athetosis, hyperkinesis; premedication (as a component of induction anesthesia); as part of complex therapy for withdrawal and toxicomania syndrome, schizophrenia (febrile form, increased sensitivity to antipsychotic drugs); prevention of states of fear and emotional stress.
Comparison of the effectiveness of Phenazepam and Tranquesipam
Phenazepam is more effective than Tranquesipam - this means that the ability of the drug substance to provide the maximum possible effect is different.
For example, if the therapeutic effect of Phenazepam is more pronounced, then with Tranquesipam it is impossible to achieve this effect even in large doses.
Also, the speed of therapy is an indicator of the speed of the therapeutic action; Phenazepam and Tranquesipam are also different, as is bioavailability - the amount of a drug substance reaching the site of its action in the body. The higher the bioavailability, the less it will be lost during absorption and use by the body.
pharmachologic effect
Anxiolytic, hypnotic, sedative, anticonvulsant, muscle relaxant. Strengthens the inhibitory effect of GABA on the transmission of nerve impulses. Stimulates benzodiazepine receptors located in the allosteric center of postsynaptic GABA receptors of the ascending activating reticular formation of the brain stem and interneurons of the lateral horns of the spinal cord; reduces the excitability of subcortical structures of the brain (limbic system, thalamus, hypothalamus), inhibits polysynaptic spinal reflexes. The anxiolytic effect is due to the influence on the amygdala complex of the limbic system and manifests itself in a decrease in emotional stress, easing anxiety, fear, and restlessness. The sedative effect is due to the influence on the reticular formation of the brain stem and nonspecific nuclei of the thalamus and is manifested by a decrease in symptoms of neurotic origin (anxiety, fear). The productive symptoms of psychotic origin (acute delusional, hallucinatory, affective disorders) are practically not affected; a decrease in affective tension and delusional disorders is rarely observed. The hypnotic effect is associated with inhibition of the cells of the reticular formation of the brain stem. Reduces the impact of emotional, vegetative and motor stimuli that disrupt the mechanism of falling asleep. The anticonvulsant effect is realized by enhancing presynaptic inhibition, suppresses the propagation of the convulsive impulse, but does not relieve the excited state of the focus. The central muscle relaxant effect is due to inhibition of polysynaptic spinal afferent inhibitory pathways (to a lesser extent, monosynaptic ones). Direct inhibition of motor nerves and muscle function is also possible.
Comparison of the safety of Phenazepam and Tranquesipam
The safety of a drug includes many factors.
At the same time, for Phenazepam it is quite similar to Tranquesipam. It is important where the drug is metabolized: drugs are excreted from the body either unchanged or in the form of products of their biochemical transformations. Metabolism occurs spontaneously, but most often involves major organs such as the liver, kidneys, lungs, skin, brain and others. When assessing the metabolism of Phenazepam, as well as Tranquesipam, we look at which organ is the metabolizing organ and how critical the effect on it is.
The risk-benefit ratio is when the prescription of a drug is undesirable, but justified under certain conditions and circumstances, with the obligatory observance of caution in use. At the same time, Phenazepam does not have any risks when used, just like Tranquesipam.
Also, when calculating safety, it is taken into account whether only allergic reactions occur or possible dysfunction of the main organs. In other matters, as well as the reversibility of the consequences of using Phenazepam and Tranquesipam.
Dosage
Inside, intramuscularly or intravenously (stream or drip). The dosage regimen is established strictly individually depending on the indications, course of the disease, tolerance, etc. For rapid relief of fear, anxiety, psychomotor agitation, as well as in vegetative paroxysms and psychotic states: IM or IV, initial dose for adults - 0 .5–1 mg (0.5–1 ml of 0.1% solution), the average daily dose is 3–5 mg, in severe cases up to 7–9 mg. Premedication: iv slowly 3–4 mg (3–4 ml of 0.1% solution). When taken orally, a single dose for adults is usually 0.5-1 mg (for sleep disorders - 0.25-0.5 mg), the average daily dose is 1.5-5 mg in 2-3 doses (usually 0.5 –1 mg in the morning and during the day and up to 2.5 mg at night), the maximum daily dose is 10 mg. Neurotic, neurosis-like, psychopathic and psychopath-like conditions: orally, initial dose of 0.5–1 mg 2–3 times a day, after 2–3 days (if necessary) - up to 4–6 mg/day; for severe agitation, the initial dose is 3 mg/day, then the dose is quickly increased until a therapeutic effect is obtained. Neurological practice (diseases with increased muscle tone): orally 2–3 mg 1–2 times a day or intramuscularly 0.5 mg 1–2 times a day. Status epilepticus, serial epileptic seizures: IM or IV, starting with a dose of 0.5 mg. For the treatment of epilepsy - 2–10 mg/day. Alcohol withdrawal: orally, 2.5–5 mg/day. The course of treatment for oral administration is 2 weeks (if necessary - up to 2 months), for parenteral administration - up to 3-4 weeks. Use with caution in the elderly and in children (the daily dose is reduced by 2-3 times).
The place of phenazepam in the modern use of benzodiazepine tranquilizers
With the advent of benzodiazepine tranquilizers in the 60s, the psychopharmacological revolution was almost completed. To the somewhat earlier antipsychotics and antidepressants, a group of tranquilizers was added, which allowed mental health specialists to create a wide arsenal of drugs for the treatment of mental disorders. In our country, the most well-known and studied benzodiazepine tranquilizer is the domestic drug Phenazepam. The study of the properties of Phenazepam began in a number of leading clinics in the country, including the Moscow Research Institute of Psychiatry, since 1976. Already the first studies [1,2,3] conducted in our clinic involving a significant number of patients (143 patients) convincingly showed that the drug has a rapid (3-5 days) and pronounced ability to reduce anxiety, fear, various sleep disorders, vegetative disorders, senesto-hypochondriacal and obsessive syndromes. Thus, the discovery of benzodiazepine tranquilizers made it possible to significantly expand the capabilities of a psychiatrist, especially in the field of minor psychiatry (neuroses, obsessive-compulsive disorder, post-stress disorders, etc.).
However, after decades of widespread and successful use of benzodiazepines in world psychiatry, problems associated with the use of this group of drugs began to arise. Thus, the uncontrolled, often unjustified use of this group of drugs has led to their abuse and the formation of addiction.
The tragedy of the fate of benzodiazepine tranquilizers lies in the fact that in addition to their powerful and rapid pharmacotherapeutic action, these drugs also have some addictive potential. The ability of benzodiazepine derivatives to cause drug dependence is widely described in the literature [4,5,6,7,8]. However, a balanced assessment of this effect has yet to be made.
Currently, a lot of work has been done to determine the duration of benzodiazepine therapy courses, since the main problem leading to the formation of addiction is unreasonably long-term use of this group of tranquilizers. Thus, the well-known Balter MB study [9] showed that in the USA by 1979, more than 15% of patients taking benzodiazepines took them for more than 1 year, and by 1990 this number increased to a quarter of all those taking anxiolytics. A pharmacoepidemiological study of outpatients revealed that among patients taking benzodiazepine derivatives, only 5.6% took them for less than six months, while the rest took them for longer periods [10]. The data presented convincingly show that the problem of abuse of drugs in this group is associated primarily with unreasonably long courses of treatment.
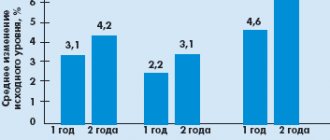
Since the 90s, in connection with the described problems, most international and domestic recommendations suggest sharply limiting the duration of treatment with benzodiazepine tranquilizers to 1 month or even 1–2 weeks to relieve acute symptoms [7, 11, 12]. A number of measures were taken to limit the frequency of prescriptions, which, however, led to controversial results. Thus, a program conducted in New York State from 1988 to 1990, limiting prescriptions for tranquilizers, led to a decrease in their use by 57%, however, in parallel, the use of other psychoactive substances, primarily barbiturates and alcohol, increased [13]. At the same time, despite the emergence of new highly effective psychotropic drugs, primarily the latest generation of antidepressants (selective serotonin reuptake inhibitors - SSRIs, selective serotonin and norepinephrine reuptake inhibitors - SNRIs) and pregabalin, the range of use of benzodiazepine tranquilizers remains wide and covers almost all nosologies . In the field of minor psychiatry, benzodiazepines remain indispensable. In recent years, in the United States and the European Union, use (prescriptions for benzodiazepines) has remained fairly stable (Fig. 1), while in Russia it has been steadily declining (Fig. 2).
According to A.B. Smulevich et al. (1976) [14], benzodiazepine tranquilizers do not fundamentally differ in the spectrum of psychotropic activity, and the features of their therapeutic action depend on the power of the anxiolytic effect. Phenazepam, according to Yu.I. Vikhlyaeva, T.A. Voronina [10], in this regard, is one of the most highly potent (powerful) tranquilizers. In light of the problems associated with the abuse of benzodiazepine tranquilizers, current guidelines recommend the use of drugs of this group with a long half-life, which include Phenazepam [15]. In addition, an important factor for the possibility of flexible use of the drug is the existence of its injectable form.
The target of Phenazepam's action is GABAergic receptors. Due to the fact that GABAergic synapses are distributed in almost all parts of the brain (cortex, cerebellum, limbic system, basal ganglia, etc.), the drug affects most brain functions.
Like all 1,4-benzodiazepine derivatives, Phenazepam has the following effects: anxiolytic, anti-obsessive, sedative, hypnotic, vegetotropic, anticonvulsant, muscle relaxant. When taken orally, the drug is well absorbed from the gastrointestinal tract, the time to reach the maximum concentration of Phenazepam in the blood is from 1 to 2 hours, the half-life from the body is from 6 to 10 hours, excretion of the drug is mainly carried out through the kidneys.
The main clinical target of Phenazepam is anxiety syndrome of any origin (neurosis, depression, generalized anxiety disorder, post-traumatic stress disorder, panic disorder, social phobia, obsessive-compulsive disorder, psychosis). In terms of anxiolytic action, Phenazepam is one of the most powerful tranquilizers, comparable in activity to lorazepam, favorably differing from it in the duration of the effect, more than 2 times greater than diazepam, 5 times greater than clonazepam and nitrazepam [11]. In 1988, a review was made of 15 clinical studies that included more than one and a half thousand patients [16]. In most cases (60%), Phenazepam was used as monotherapy, in 40% it was combined with drugs from other groups (neuroleptics, antidepressants, mood stabilizers). Daily doses averaged 3–5 mg/day. As a result of the treatment, significant improvement was recorded in 63.3%, in 28.8% the effect was insignificant and only in 7.9% there was no effect. Phenazepam turned out to be the most effective in the treatment of mental disorders of the neurotic level, in the structure of which anxiety predominated. Already in the first days after the administration of Phenazepam, a significant decrease in anxiety tension, irritability, sleep disturbances, and somatovegetative disorders was observed. It was also noted that the effect achieved after one month of therapy was persistent. In addition, it was found that the use of the drug for affective disorders turned out to be effective in the case of predominance of depressive anxiety syndrome in the structure and, conversely, the least effective - when manifestations of vital depression and adynamic disorders predominated in the clinical picture. Based on the generalized data, it was found that the use of the drug as monotherapy for psychotic disorders was ineffective. Thus, the effectiveness of the drug decreased if the level of disorder shifted from neurotic to psychotic level.
A study of the vegetotropic effect of Phenazepam in neurotic patients at a daily dose of 3 mg in comparison with diazepam at a dose of 40 mg/day showed that the effect of Phenazepam appeared on days 4–5, coinciding with the anxiolytic effect. A pronounced vegetotropic effect occurred on the 10–12th day. The use of Phenazepam turned out to be more effective in the sympathoadrenal structure of the autonomic crisis than in the vagoinsular one. In terms of its therapeutic effect on autonomic symptoms, Phenazepam was more effective than diazepam [17].
A study of the effect of Phenazepam in agripnic disorders showed a clear positive effect on all types of sleep disorders (disturbances in falling asleep, night awakenings, early insomnia), superior in severity and speed of onset to all other tranquilizers, including diazepam. The effect of the drug, as a rule, was not accompanied by morning drowsiness and lethargy [18]. Phenazepam is also effective for sleep disorders of alcohol origin [19]. It must be emphasized that the prescription of Phenazepam as a hypnotic drug should take into account the periods currently recommended by WHO and domestic guidelines, that is, no more than 1 month [7, 11, 12].
A review summarizing the use of benzodiazepine tranquilizers in epilepsy notes that Phenazepam has been successfully used in combination therapy with anticonvulsants to treat various types of seizures [19, 20]. The introduction of Phenazepam into the regimen for the treatment of resistant polymorphic seizures led to a complete cessation or halving of their frequency in 60% of patients [21, 22].
Benzodiazepine tranquilizers play an important role in the treatment of somatic and psychosomatic diseases. Thus, in the review work of V.A. Raisky [21] noted the high effectiveness of benzodiazepines in anxiety, anxiety-phobic and accompanying vegetative disorders in cardiovascular, gastrointestinal, pulmonary and other diseases. At the same time, depending on the task, the drug had both the main anxiolytic and hypno-sedative, anticonvulsant and muscle relaxant effects. It was noted that Phenazepam in doses of 1.5–2 mg/day was superior to diazepam and nitrazepam in all types of action and showed equal results with lorazepam. Its moderate analgesic effect was also noted [23].
Phenazepam is widely used in cardiology. The main indication for treatment with Phenazepam is neurohumoral disorders of the cardiovascular system in the form of vegetative paroxysms of the sympathetic-adrenal type with cardialgia, hyperhidrosis, tachycardia, accompanied by fear of death and psychomotor agitation. The use of Phenazepam at a dose of 1–3 mg/day relieves vegetative paroxysms, sleep disturbances, and cardialgia [24]. There is evidence that Phenazepam at a dose of 1.5 mg/day has an antiarrhythmic effect on various heart rhythm disorders - atrial, ventricular, supraventricular extrasystole, paroxysms of atrial fibrillation. Phenazepam is most effective (69%) in patients with an association of heart rhythm disturbances with neurotic disorders [14].
Phenazepam is successfully used in complex therapy for coronary heart disease (CHD). Thus, already in the first days of taking the drug, night sleep is normalized, anxiety and fear for one’s life and health, irritability, and fixation on various manifestations of the disease are reduced. Phenazepam has a significant positive effect on autonomic-vascular dysfunctions - headache, sweating, respiratory arrhythmia. It was found that Phenazepam is more effective for neurosis-like disorders in patients with coronary artery disease (70%) compared to diazepam (62%) and chlordiazepoxide (49%) [25].
Benzodiazepines are widely used in anesthesiology and resuscitation. They are used for preoperative sedation, as an introductory drug for general anesthesia and potentiation of its effect.
Phenazepam is used for sedation of seriously ill patients on mechanical ventilation. The drug has the ability to block the mechanisms of psychogenic provocation of bronchial asthma attacks, which is observed in 19–51% of patients [26].
Phenazepam is used in gynecological practice in the treatment of premenstrual tension syndrome. It has been shown to be more effective than traditionally used hormonal therapy [27].
The presence of a muscle relaxant effect in Phenazepam allows its use in neurological disorders: extrapyramidal disorders, increased muscle tone (tardive dyskinesia, essential tremor, restless legs syndrome) [28]. There is successful experience in using the drug for headaches (tension headache, migraine, post-traumatic encephalopathy) [29]. The presence of sedative and vegetative-stabilizing effects in benzodiazepines, the ability to reduce spastic phenomena, and reduce the content of pepsins and hydrochloric acid in gastric juice justifies their use in gastroenterological practice in the treatment of gastric ulcers, dyskinesia of the gastrointestinal tract, ulcerative colitis, etc. [9]. At a daily dose of 2–3 mg, Phenazepam was effective for cardio- and angioneurosis, hyperventilation syndrome, “irritable stomach”, “irritable colon”, “irritable bladder” [30].
Thus, the data presented indicate the widespread use of Phenazepam in general somatic practice. The breadth and diversity of the clinical profile of Phenazepam makes it possible to use it in many areas of medicine.
At the same time, it is necessary to take into account the most important issues of tolerability, adverse events, as well as the dosage regimen and criteria for the duration of benzodiazepine therapy courses. 1,4 benzodiazepine derivatives are one of the safest groups of drugs in medicine, due to the “wide corridor” between therapeutic and toxic doses. There are no data on deaths as a consequence of treatment with Phenazepam and other tranquilizers in therapeutic doses [12], and deaths from overdose with benzodiazepines are extremely rare [31]. The drugs do not have a significant effect on the cardiovascular, hepatic, endocrine and urinary systems [32]. However, when prescribing Phenazepam, it is worth considering the possibility of its interaction with certain drugs used in both psychiatric and somatic practice. It is necessary to mention the ability of benzodiazepine tranquilizers in combination with barbiturates and opiates to depress the respiratory center. It is worth considering this possible complication when prescribing Phenazepam in patients with chronic obstructive pulmonary diseases [3, 18].
A much more serious aspect of inappropriate use of benzodiazepine anxiolytics is withdrawal syndrome. Most often, this phenomenon occurs when the drug is abruptly discontinued or discontinued after an unreasonably long (more than 1 month) course of therapy. Typical withdrawal symptoms are anxiety, irritability, sleep disturbances, headaches, muscle twitching, tremors, increased sweating, and dizziness [33]. In the vast majority of cases, to relieve withdrawal symptoms, it is enough to use the discontinued drug. Thus, in a survey of general practitioners and psychiatrists in Moscow, of the cases assessed as withdrawal syndrome, 83% had a mild form of the disorder that did not require drug treatment. There are polar opinions on this issue in the literature. The number of patients with withdrawal syndrome ranges from 0.1 to 100% [34]. It is often extremely difficult to distinguish the manifestations of this phenomenon from the manifestations of the underlying disease, which occurs predominantly with alarming symptoms [35]. To avoid the development of withdrawal syndrome and the formation of dependence when using benzodiazepine tranquilizers, in addition to limiting the course duration, you can use several simple recommendations given in Table 1.
Thus, Phenazepam is effective for various conditions and has a scope of application in almost any field of medicine, being a highly effective, fast-acting and safe remedy for solving a huge number of tactical problems that clinicians often encounter in their practice. At the same time, it is not recommended to prescribe Phenazepam (like all benzodiazepine derivatives) as long-term therapy. The course of treatment with the drug should not exceed 1 month [11, 12]. It is obvious that the combination of the wide therapeutic profile of the drug, the power and safety of its action still determine the high demand for Phenazepam in the treatment of patients with anxiety (neurotic) and psychosomatic disorders.
LITERATURE
1. Avedisova A.S. On the issue of addiction to benzodiazepines // Psychiatry and psychopharmacotherapy. 1999; 1:12–15. 2. Avedisova A.S., Yastrebov D.V., Kostacheva E.A. and others. Pharmacoepidemiological analysis of outpatient prescription of benzodiazepine tranquilizers in psychiatric institutions // Russian Psychiatric Journal. 2005; 4:10–12. 3. Avrutsky G.Ya., Vovin R.Ya., Lichko A.E., Smulevich A.B. Biological therapy of mental illnesses. L.: Medicine, 1975; 311. 4. Avrutsky G.Ya., Aleksandrovsky Yu.A., Berezova N.Yu. and others. Use of the new tranquilizer Phenazepam in psychiatric practice // Journal of Neuropathology and Psychiatry named after. Korsakov. 1979; 3: 344–350. 5. Avrutsky G.Ya., Neduva A.A. Treatment of mental patients. Guide for doctors. M.: 1988; 528. 6. Aleksandrovsky Yu.A. Clinical pharmacology of tranquilizers. M.: Medicine, 1973. 7. Aleksandrovsky Yu.A., Benkovich B.I. and others. The place of psychopharmacotherapy in the treatment of autonomic dysfunctions in patients with borderline forms of neuropsychiatric disorders. Paroxysmal autonomic disorders. M.: 1979. 8. Andronati S.A., Avrutsky G.Ya., Bogatsky A.V. and others. Phenazepam. Kyiv. 1982; 288. 9. Balter MB, Uhlenhuth EH The beneficial and adverse effects of hypnotics // J Clin Psychiatry, vol.52 (Suppl.), 1991, 16-23 10. Vikhlyaev Yu.I., Voronina T.A. Pharmacology of Phenazepam // Express information: new drugs. M.: VNIIMI, 1978; 3: 265–279. 11. Voronina T.A. Position of Phenazepam among benzodiazepine drugs. New psychotropic drugs. Proceedings of the symposium. Lvov, 1978; 100. 12. Holmgren P., Jones AWJ Forensic Sci. 2003; 48:6:1416–1421. 13. Drobizhev M.Yu. Psychopharmacotherapy in the general somatic network (somatotropic effects, compatibility with somatotropic drugs) //Psychiatry and psychopharmacotherapy. 2000; 2: 2. 14. Smulevich A.B., Mazaeva N.A., Golovanova L.A. and others. Differentiated pharmacotherapy of neurotic conditions (comparative effectiveness of benzodiazepine derivatives) // Journal. neuropathology and psychiatry named after. Korsakov. 1976; 2: 255–262. 15. Kaplan G.I., Sadok B.D. Clinical psychiatry. 1994; 2: 412. 16. Kostovski V. Benzodiazepines: mechanisms of action and application. 1988. pp. 28–37 17. Mezhevitinova A.E. Premenstrual syndrome (to help the practitioner) // Gynecology. 2002; 4: 23. 18. Mosolov S.N. Basics of psychopharmacotherapy. M.: 1996; 288. 19. Mosolov S.N. Psychopharmacological and antiepileptic drugs approved for use in Russia, Ed. 2nd, revised, M.: 2004; 301. 20. Patsernyak S.A. Stress. Vegetoses. Psychosomatics. St. Petersburg ABC. 2002; 384. 21. Raisky V.A. Psychotropic drugs in the clinic of internal diseases. M.: Medicine. 1988; 256. 22. Rudenko G.M., Shatrova N.G., Lepakhin V.K. Features of psychotropic activity and effectiveness in the treatment of various conditions of the original domestic tranquilizer Phenazepam. Express information: New drugs. M.: VNIIMI. 1978; 3:7–29. 23. Rudenko G.M., Shatrova N.G., Lepakhin V.K. Psychotropic activity and effectiveness of Phenazepam in the treatment of various conditions. Phenazepam. Kyiv. 1982; 228–245. 24. Seredenin S.B., Voronina T.A., Neznamov G.G., et al. Phenazepam: 25 years in medical practice. The science. 2007; 222. 25. Smulevich A.B., Drobizhev M.Yu., Ivanov S.V. Clinical effects of benzodiazepine tranquilizers in psychiatry and general medicine. M.: 2005; 56. 26. Smulevich A.B., Drobizhev M.Yu., Ivanov S.V. Clinical effects of benzodiazepine tranquilizers in psychiatry and general medicine. M.: Media Sphere. 2005; 88. 27. Smulevich A.B., Drobizhev M.Yu., Ivanov S.V. Clinical effects of benzodiazepine tranquilizers in psychiatry and general medicine. M.: Media Sphere. 2005; 68. 28. Smulevich A.B., Drobizhev M.Yu., Ivanov S.V. Clinical effects of benzodiazepine tranquilizers in psychiatry and general medicine. M.: 2005; 51. 29. Ashton H. Benzodiazepine withdrawal: an unfinished story // Brit Med J 1984; 288:1135–1140. 30. British national formulary No. 31, 1996. 31. Karobath M. Molecular basis of benzodiazepine action // Trends Neurosci. 1979; 2: 166. 32. Reidenberger MM Effect of requirement for triplicate prescription for benzodiazepines in New York state // Clin Pharmac and Terap. 1991; 50: 129–131. 33. Roy-Byrne PP, Hommer D. Benzodiazepine withdrawal: overview and implications for the treatment of anxiety // Am J Med. 1988; 84:1041–1052. 34. WHO. Program on substance abuse. Rational use of benzodiazepines. 1996. 35. Laughren TP, Baltey Y., Greenblat DJ Chronic diazepam treatment in psychiatric outpatients // Aсta Psychiat Scand. 1982; 65:171–179
Comparison of ease of use of Phenazepam and Tranquesipam
This includes dose selection taking into account various conditions and frequency of doses. At the same time, it is important not to forget about the release form of the drug; it is also important to take it into account when making an assessment.
The ease of use of Phenazepam is approximately the same as Tranquesipam. However, they are not convenient enough to use.
The drug ratings were compiled by experienced pharmacists who studied international research. The report is generated automatically.
Last update date: 2020-12-13 10:31:30
Comparison of addiction between Phenazepam and Tranquesipam
Like safety, addiction also involves many factors that must be considered when evaluating a drug.
So, the totality of the values of such parameters as “syndrome o” for Phenazepam is less than the similar values for Tranquesipam. Withdrawal syndrome is a pathological condition that occurs after the cessation of intake of addictive or dependent substances into the body. And resistance is understood as initial immunity to a drug; in this it differs from addiction, when immunity to a drug develops over a certain period of time. The presence of resistance can only be stated if an attempt has been made to increase the dose of the drug to the maximum possible.
Side effects
From the nervous system and sensory organs: drowsiness (usually in the first days of treatment), lethargy, dizziness, increased fatigue, headache, memory impairment, muscle weakness, ataxia, tremor, slurred speech, paradoxical reactions in mentally ill patients, incl. . psychomotor agitation, anxiety.
Other: dry mouth, nausea, dyspeptic symptoms, leukopenia, impaired liver function (including jaundice), allergic reactions, fainting, changes in libido.
Possible addiction, drug dependence, syndrome o).
Comparison of side effects of Phenazepam and Tranquesipam
Side effects or adverse events are any adverse medical event that occurs in a subject after administration of a drug.
Phenazepam has more adverse effects than Tranquesipam. This implies that the incidence is low for Phenazepam and low for Tranquesipam. Frequency of manifestation is an indicator of how many cases of an undesirable effect from treatment are possible and registered. The undesirable effect on the body, the strength of influence and the toxic effect of drugs are different: how quickly the body recovers after taking it and whether it recovers at all. When using Phenazepam, the body's ability to recover faster is higher than that of Tranquesipam.
Precautions for the substance Oxazepam
Use with caution in cases of predisposition to arterial hypotension, especially in elderly patients (due to the possibility of cardiac dysfunction), and an increased risk of drug dependence.
Should not be administered with MAO inhibitors, phenothiazine derivatives. The likelihood of overdose symptoms increases with concomitant use of CNS depressants or alcohol. During the treatment period, alcoholic beverages are excluded.
Should not be used for a long time (due to the risk of developing drug dependence). If long-term treatment is necessary (several months), the course should be carried out using the method of intermittent therapy, stopping treatment for several days and then prescribing the same individually selected dose. Cancellation should be carried out gradually. With abrupt withdrawal of oxazepam, withdrawal syndrome may occur (tremor, convulsions, abdominal or muscle spasms, vomiting, perspiration), most often appearing after taking high doses or long-term treatment.
With long-term treatment, monitoring of liver function and peripheral blood patterns is necessary.
Should not be used by vehicle drivers and people whose profession involves increased concentration of attention.
Overdose
Symptoms: CNS depression of varying severity (from drowsiness to coma) - drowsiness, confusion, lethargy; in more severe cases (especially when taking other drugs that depress the central nervous system, or alcohol) - ataxia, decreased blood pressure, hypnotic state, coma.
Treatment: induction of vomiting, gastric lavage, symptomatic therapy, monitoring of vital functions. For severe hypotension, norepinephrine is administered. The specific antidote is the benzodiazepine receptor antagonist flumazenil (administration only in a hospital setting). Hemodialysis is ineffective.