There are contraindications, consultation with a specialist is required
The benefits of nettle have been known for several thousand years: even in the works of Hippocrates, Dioscorides and Galen, healing properties and use for medical, cosmetic and nutritional purposes were mentioned. This is a universal plant for promoting health, maintaining tone and improving mood. The herb is also used to nourish and enrich the body not only with vitamins, but also with proteins and carbohydrates. Nettle has found application in medicine, cooking and cosmetology.
Useful properties of nettle
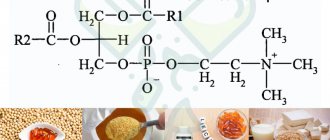
So what are the benefits of this herb? An infusion of this burning plant improves the functioning of the gastrointestinal tract and has a choleretic effect. Thanks to the large amount of plant protein and lectin, the herb has a strong antitoxic effect, and the chlorophyll in its composition helps in healing wounds and strengthening the hair structure.
Effects:
- normalization of lipid metabolism due to the presence of iron salts and vitamins;
- weight loss and acceleration of metabolism and, as a result, assistance in weight loss;
- pronounced hemostatic effect;
- choleretic and anti-inflammatory effects;
- improvement of lactation in lactating women;
- increased metabolism due to the content of large amounts of chlorophyll;
- normalization of cardiac and respiratory activity;
- maintaining vision due to the presence of vitamin A;
- the role of an antioxidant, as it contains a lot of vitamin C;
- protection and maintenance of immunity;
- lowering sugar levels and, consequently, helping people suffering from diabetes;
- hemostatic, wound healing, anti-inflammatory;
- treatment of anemia, as it increases hemoglobin;
- fight against various skin inflammations;
- hair care in the form of masks and lotions.
Garden doctor
Stinging nettle and stinging nettle
People have known about the benefits of nettle for a long time and successfully used it to treat various diseases, but even in our time this plant has not lost its popularity. Nettle is unpretentious and grows almost everywhere: in forests, near rivers, in gardens and parks. There are two types of this plant - dioecious and stinging. The properties of the former are considered especially medicinal.
The herbal mixture can be purchased at a pharmacy or collected independently. But you need to choose environmentally friendly places to collect this medicinal herb. It would be better if it was a forest clearing. Under no circumstances should you collect the plant near the roads; instead of the expected benefit, you may get the opposite.
Chemical composition
If you ask the question “how is nettle useful for humans?”, then the first answer will be its chemical composition, because it contains a huge amount of microelements.
Nutritional value per 100 grams:
- proteins - 4 grams,
- fats - 0 grams,
- carbohydrates - 5 grams,
- calorie content - 24.8.
What vitamins are in nettle?
Since this herb is a multivitamin plant, its leaves contain twice as much ascorbic acid than blackcurrant, lemon or apple, and the carotene level is higher than that of carrots. The plant contains vitamins A, C, group B (B1, B2, B3), E and K, macro- and microelements. The presence of vitamin K is responsible for the hemostatic effect of stinging grass.
Contains:
- glycoside urticine, ergosterol, carotenoids, phytosterols;
- chlorophyll, violaxanthin;
- pantothenic, formic, silicon, gallic acids.
In what form is it used?
The benefits of nettle for humans have long been known, so it is often used in the treatment of boils, acne, and also as a remedy for rheumatism and gout. To do this, it is recommended to use it in the form:
- water infusion,
- briquettes with crushed leaves,
- liquid extract.
This herb grows everywhere in the northwest and central Russia, so collecting it yourself is not difficult for many residents of the country. Therefore, in times of famine, the healing properties of stinging nettle saved many people from vitamin deficiency. The main thing is to choose, collect or buy a plant from ecologically clean regions of Russia.
Important information! If you decide to collect the grass with your own hands, then know: it is best to use leaves that are collected from May to June for treatment. The collection must be dried in a uniform layer up to 5 cm thick.
You can use modern dryers, in which it is necessary to set the temperature to 50°. The shelf life of this product is two years. You can also dry the roots, which have beneficial qualities. The roots are collected and stored from late autumn to the first days of spring, the flowers of the plant - in the summer, and the seeds - from late summer to early autumn. To make nettle juice, you only need young shoots and stems before the inflorescences form.
Nettle juice, or nettle juice
Juice is squeezed from nettle leaves: for these purposes you can use a juicer or a regular meat grinder. The juice has beneficial properties of the plant itself; its use can relieve fatigue, replenish the lack of vitamins in the body and improve metabolism in the body. It is also believed to help prevent osteoporosis because it helps strengthen bones.
Nettle juice
When using the juice, it is recommended to dilute it with a small amount of water to reduce the concentration. It is best to store such a product in the refrigerator, and the juice has a very limited shelf life: it must be consumed within 3 days, so trying to prepare the juice for future use is simply useless.
In scientific research
- Studies conducted on rats have confirmed the anti-inflammatory effect of stinging nettle extract in a model of Alzheimer's disease. In a study, Gholam Hossein Riazi (Laboratory of Neuroorganic Chemistry, Institute of Biochemistry and Biophysics, Tehran University in Iran) confirmed the antiproliferative effect in small cell lung cancer, which is characterized by high mortality.
- Wafa Siuda (Faculty of Biological Sciences, Badji Mokhtar Annab University) asked the question “why is nettle good for you?” and conducted a study on “Can stinging nettle supplementation reduce mercury toxicity in rats?” The results of his work clearly demonstrated the antitoxic effect.
- In 2013, V. Hadjashemi and Vahid Klushani wrote an article in a medical journal about the antinociceptive and anti-inflammatory effects of stinging nettle leaf extract when exposed to animals. Thanks to their work, it began to be used more often as a traditional remedy for musculoskeletal pain and rheumatism.
- In 2016, Rahila Qayyum (Faculty of Pharmacy, COMSATS Institute of Information Technology, Pakistan) conducted a study on the mechanisms underlying the antihypertensive properties of stinging nettle.
- The extract is effective as an antioxidant in the adjuvant therapy of type II diabetes mellitus and helps minimize the risk of developing cardiovascular diseases and other complications in patients with diabetes mellitus. This was published by Alidad Amiri Behzadi from the Young Researchers and Elite Club of the Islamic Azad University of Iran, “Effects of stinging nettle supplementation on blood lipids, liver enzymes and nitric oxide levels in patients with type II diabetes mellitus: a double randomized clinical trial.”
- In 2022, Karama Zuari Bouasida wrote an article on the topic “Study on the hemostatic and wound healing potential of stinging nettle leaves.”
- The antibacterial activity of stinging nettle was studied in 2014 by Professor of the Faculty of Biology Hossein Motamedi from Shahid Chamran University of Ahvaz.
- Traditionally used to treat cardiovascular diseases, especially hypertension. Animal studies have confirmed the antihypertensive effect attributable to calcium channel blockade and NO-mediated vasorelaxation. Rohit Bisht from the Department of Pharmacology at ISF College of Pharmacy in Punjab, India, has released a study on this topic.
In official medicine
It has been known as a medicine since the 17th century, its benefits have been proven by modern medical research, so it is actively used:
- in the treatment of gastrointestinal diseases (ulcers, gastritis, colitis);
- with anemia;
- as an antihemorrhagic agent;
- against pulmonary, uterine and other bleeding.
Medicinal properties include increasing blood clotting and hemoglobin, stimulating erythropoiesis and increasing the number of platelets in the blood. The herb increases prothrombin levels when anticoagulants are administered in excess and produces a vasoconstrictor effect. Nettle-based drugs sold in pharmacies have choleretic, anthelmintic, diuretic, anti-inflammatory, and expectorant effects. They are also used for diabetes.
For women's health
This plant can bring both benefit and harm to women, therefore, representatives of the fair sex should be careful. While it will help nursing mothers improve milk production for the baby, it can be dangerous for pregnant women, as it greatly increases the tone of the uterine muscles and can lead to miscarriage.
But during childbirth, it can help women in labor with bleeding disorders and blood loss, and promote rapid and painless contraction of the uterus after childbirth. Therefore, the question “is nettle good for pregnant women?” While it remains open, be sure to consult a physician before use.
In general, the plant is widely used for an analgesic effect and as a hemostatic agent, therefore it will be effective for various gynecological ailments: uterine bleeding and for normalizing menstrual cycles.
For men's health
Why nettle is useful for men: to strengthen potency. The herb has a beneficial effect on the reproductive system and helps in the treatment of prostate adenoma. The herb is used as a general tonic and prophylactic; all components of the plant can be used - seeds, roots, leaves. Traditionally, the duration of treatment is four weeks. Also, herbs can be supplemented with the main course of treatment with medications, but this is only permitted in consultation with a doctor. Independent actions can lead to adverse consequences from other body systems.
In folk medicine
Apply:
- as a diuretic herb in the treatment of edema syndrome;
- for diseases of the kidneys, liver and biliary tract (constipation, cholecystitis, nephritis, pyelonephritis);
- in the treatment of gout, iron deficiency anemia and polyarthritis;
- for atherosclerosis, bronchial asthma, whooping cough;
- during hypertension and even during cancer treatment.
The seeds can help women with infertility and men with impotence. To do this, nettle seeds need to be mixed with a softened banana and eaten every day. Freshly squeezed juice from the leaves is recommended for the treatment of osteomyelitis and for problems with digestion of food, as well as for large amounts of salts in the joints. The leaves are brewed and consumed to strengthen the immune system during colds and flu.
It is useful for poor appetite, gastritis, enterocolitis, pathology of the cardiovascular system, in particular for heart failure of I and II degrees, tachycardia. Plus, it helps restore the sense of smell when it is lost or sensitivity decreases. Powder of sun-dried leaves is used to treat ulcers and ulcers.
What are the benefits of nettle infusion?
A strong infusion of leaves is an excellent remedy for ulcers, burns and small wounds. It is actively used to strengthen hair when it is dry and brittle, as well as to treat dandruff. Recipe: Pour warm water over the chopped herbs, making sure to leave some room for fermentation. Cover the container with a lid, a board or wrap it in burlap and place in a warm place for 7–14 days.
What are the benefits of nettle decoction?
Taking the decoction a few days before the start of the menstrual cycle helps reduce the amount of blood loss in women. The decoction is also useful for patients with diabetes, but for a healing effect you need to know how to brew fresh herbs correctly. We offer the following option. Cooking recipe: mix 2 tbsp. tablespoons of dried nettle and mint leaves, add 3 liters of water and cook for 3 minutes. Leave for about half an hour and filter. You can add honey to the broth.
In cooking and dietetics
In cooking, nettle leaves, seeds and roots are popular in the preparation of salads and first courses (pickle soup, borscht), they are also added to sauces, fillings for pies, plus salted and fermented for the winter. To reduce the pungency, the leaves are treated with boiling water. Young, tender inflorescences are added to tea and dried for the winter. You should add it to hot dishes a couple of minutes before they are ready, but first rinse cold dishes, put them in boiling water and cook for two minutes, rinse them with cold water, and only then you can cut them - then you won’t get burned. Often adding recipes with nettle to the menu, you can reduce weight, because 100 grams of this herb contains only 24.8 calories.
Important information! If you eat untreated leaves often and a lot, flatulence will occur.
Tea
For a simple and vitamin-packed tea recipe, take:
- nettle leaves,
- dog-rose fruit,
- thyme.
Pour one tablespoon of each ingredient into two glasses of hot water into a container. Allow the finished product to stand for two hours, then drink as regular tea. Another advantage of this tea is that there is no need to waste time preparing the decoction.
Dangerous properties and contraindications
It is not recommended for use by people diagnosed with varicose veins or thrombophlebitis, as this plant strongly thickens the blood. Under no circumstances should it be used by pregnant women, as it can cause contractions and premature birth.
Support of lactation, prevention and treatment of hypogalactia
World Health Organization experts recommend exclusive breastfeeding for children for the first 6 months and continued breastfeeding until at least 2 years of age [1–4]. According to the literature, one of the main reasons for refusing breastfeeding is an insufficient amount of breast milk, or hypogalactia. Prevention and treatment of hypogalactia allows you to increase the duration of breastfeeding [1–4].
Breast milk production is a complex physiological process involving many factors and the interaction of a large number of hormones. The most important hormone affecting lactation is prolactin. Its secretion occurs according to the principle of negative feedback with dopamine. When dopamine concentration decreases, prolactin secretion from the anterior pituitary gland increases. Within a few months of starting breastfeeding, most breastfeeding women have high prolactin levels compared to non-breastfeeding women. Once lactation is established, there is no direct correlation between serum prolactin levels and breast milk volume in lactating women [1].
Depending on the severity of milk deficiency, four degrees of hypogalactia are distinguished: 1st degree - deficiency up to 25%, 2nd degree - deficiency up to 50%, 3rd degree - deficiency up to 75%, 4th degree - deficiency more than 75% . There are early (in the first 10 days after birth) and late forms (after the 10th day) of hypogalactia [4, 5]. Primary hypogalactia (occurs in 3–5% of women) occurs after severe gestosis, traumatic obstetric operations, bleeding in the postpartum period, and postpartum infections. Secondary hypogalactia (occurs in 95–97% of women) is registered with a late first attachment of a child to the breast, with irregular and incorrect attachment, with attachment to only one breast, with long breaks between feedings (more than 2–2.5 hours), as well as in case of violation of the daily routine, excessive physical activity, poor sleep, stress, maternal fatigue, regular separation of mother and child (hospitalization in a hospital, mother going to work or study) [1, 2, 4, 5].
Very often, the statement about an insufficient amount of breast milk is based solely on the subjective opinion of women [1–4]. The perception of lactation as insufficient is common among breastfeeding women. This leads to anxiety, which in turn can impair breastfeeding [1, 3]. An important factor leading to a decrease or cessation of breastfeeding is the introduction of supplementary feeding with infant formula in the first days after birth, when lactation begins [6].
To initiate lactation, the woman’s correct motivation and desire to breastfeed are important. It is necessary to provide counseling on breastfeeding issues not only to the mother and father of the child, but also to all family members. In the Russian Federation, an association of breastfeeding consultants has been operating since 2004. Of great importance for counseling nursing mothers on lactation issues is the joint work of medical staff with specialists from the association on issues of breastfeeding support [1, 3–5, 7]. To increase lactation, frequent latching of the baby to the breast (latching on demand), night feedings, correct positioning of the baby at the breast with adequate capture of the areola, increased contact between mother and baby, the use of the kangaroo method, and skin-to-skin contact are necessary. It is necessary to pay attention to the correct daily routine of a nursing woman, ensure proper rest and adequate sleep, regular walks in the fresh air, adequate nutrition and fluid intake.
According to the Academy of Breastfeeding Medicine (ABM) protocol, lactagogues can be used if breastfeeding counseling fails [1, 8]. Lactagogues are often used to stimulate lactation in mothers after premature birth, as well as when the child is hospitalized in the intensive care unit. Currently, the lactogonic effect is described in pharmaceuticals and herbal products (lactogonous herbs) [1, 3–5, 8].
Domperidone and metoclopramide are considered pharmaceutical lactogenic drugs. Both are dopamine antagonists, increase basal serum prolactin levels and lead to an increase in breast milk supply. A number of studies have confirmed an increase in prolactin levels in lactating women who were prescribed the drugs domperidone and metoclopramide. Domperidone in the USA and Canada was used orally as a lactation stimulant in doses of 30–60 mg/day [1, 3, 8–10]. However, the optimal dosage for the use of domperidone in women with different serum prolactin levels has not been determined. The experience of using domperidone to initiate lactation in nulliparous women has been described [1, 8–10]. In the United States, the use of domperion and metoclopramide to stimulate lactation is not approved by the Food and Drug Administration (FDA). Domperidone increases the QT interval and can lead to ventricular arrhythmias and sudden death [1, 3, 8–10]. The use of metoclopramide is inferior to domperidone in stimulating lactation and can have serious adverse neurological consequences [1, 8, 11]. However, in some US clinics, drugs are still included in clinical protocols as means to stimulate lactation in mothers of premature babies [1, 3, 8, 12]. It should be noted that the lactogenic effect has been described in human growth hormone, thyrotropin-releasing hormone. However, they are not currently used to stimulate lactation [1, 8].
Currently, a large number of lactogenic herbs and herbal remedies are known that can increase the secretion of breast milk. The use of lactogonic herbs is included in domestic and foreign recommendations for the prevention and treatment of hypogalactia [1, 3–5, 13–15]. A survey conducted in the United States found that more than 70% of health care providers and lactation consultants recommend lactagogues [3, 15, 16].
Most often in foreign literature, fenugreek, goat's rue, thistle, oats, millet, anise, basil, hops, ginger, and seaweed are mentioned as lactogenic herbs [1, 3–5, 8, 13, 14, 16]. However, many of the drugs listed should be treated with great caution due to unproven effects and possible side effects. For example, goat's rue (Galega officinalis L.), despite its lactic effect, can increase blood pressure and lead to disruption of the gastrointestinal tract [1, 3, 8]. Fenugreek (Fenugreek, Trigonellafoenum graecum) is most widely used as a lactogenic agent in Canada and the USA. Many authors indicate the effectiveness of fenugreek and an increase in milk supply in approximately 75% of lactating women [1, 3, 8]. The use of fenugreek is included in current protocols for the initiation and stimulation of lactation [1, 8, 16]. In the Russian Federation and in many foreign countries, medical staff and consultants most often use fennel, dill, anise, cumin, nettle, lemon balm, and oregano as lactogenic herbs [1, 3–5, 8].
Fennel (Foeniculum vulgare) ranks first among herbal lactogonics in terms of frequency of prescription in Switzerland [16], and is also widely used in the USA [15, 17]. Fennel seeds contain 40–60% anethole. Anethole is a phytoestrogen and is structurally similar to dopamine. Anethole can compete with dopamine for receptors, blocking the inhibitory effect of dopamine on prolactin secretion [1, 3, 5]. Fennel in 2022 is described in a review of lactogenic herbs used in traditional Iranian medicine [13]. Fennel is often used to reduce infant colic [14, 18]. However, if the mother is allergic to carrots and celery, then due to possible cross-allergy to plants of the Umbelliferae family, fennel should not be used [3, 5].
Stinging nettle (Urtica dioica) is used in many countries in traditional medicine as a means of stimulating lactation. Nettle also has hemostatic, anticonvulsant and analgesic properties [5]. Stinging nettle is included in the American Breastfeeding Guide [17]. Nettle is also included in many foreign combined herbal medicines used to stimulate lactation [1, 3, 8, 17, 19].
Anise fruits (Pimpinella anisum) are widely used in traditional medicine as a lactogenic agent [1, 8]. Anise seeds contain anethole, which increases prolactin synthesis by competing with dopamine for receptors [3, 5, 20]. Anise is used as a lactogenic agent by midwives in Switzerland [16] and in traditional Iranian medicine [13]. In nursing women, while taking preparations from anise seeds, there is an increase in the tone of the uterus, which accelerates the process of its recovery after childbirth [5]. Anise is effective in treating postpartum depression [19]. In Arab countries, anise has been described as an herbal remedy for colic in newborns [21].
Cumin (Carum carvi) is considered one of the oldest spices that promotes lactation [3–5]. Cumin in English literature is more often found under the name Carvone [1, 3, 5, 8]. Cumin fruits have a positive effect on intestinal motility and stimulate bile secretion [3, 5]. The anesthetic properties of cumin are known for pain in the stomach and intestines [5]. The use of cumin as a herbal lactogenic agent has been described in both traditional and modern Syrian medicine [14].
Despite the fact that many herbal preparations have been used to stimulate lactation in lactating women for quite a long time, very few studies have been published to assess the effectiveness of lactogenic herbs and herbal medicines [1, 8]. It is possible that the reason for the effectiveness of herbal preparations may be the “placebo effect” [1, 4, 8, 22]. Most studies of the effectiveness of lactogenic agents have been conducted in women after premature birth who used breast pumps [1, 7, 8]. There is currently insufficient data on the use of lactogenic agents in women who have given birth to full-term infants, whose lactation problems usually arise in the first few days or weeks after birth [1, 8].
Difficulties also arise from the fact that when using medicinal herbs there are no standard dosages. In addition, the risk of developing allergies and possible plant contamination should be taken into account. When using lactogonic herbs in women, their possible effect on the child should be taken into account [1, 3, 8]. Currently, additional research is required to evaluate the effectiveness and safety of lactogonic herbs and herbal medicines [1].
To initiate and support lactation, complete, high-quality and balanced nutrition for a nursing mother is important, therefore the diets of nursing women should additionally include 30–40 g of protein, 15 g of fat, 30–40 g of carbohydrates, which corresponds to 400–500 kcal [1, 2, 23]. It is known that adequate production of prolactin in a woman occurs only with a sufficient level of protein in the diet [23]. The diet of a nursing woman should contain a sufficient amount of fluid necessary for lactation [4, 23].
One of the ways to provide nursing mothers with the necessary amount of nutrients is to include specialized products in the women’s diet: NutriMa Femilak, Bellakt Mama +, Juno. Currently, balanced formulas for nursing mothers with lactogenic additives are available. These products not only enrich the diet with additional nutrients, but also stimulate the secretion of breast milk [1, 8, 9, 23, 24]. Such products include Milky Way and NutriMa Lactamyl mixtures. The Milky Way mixture is a dry fortified milk-soy mixture with galega extract [1, 9, 23, 24]. NutriMa Lactamil is a dry milk-based product with a complex of lactogenic herbs: fennel fruits, anise, cumin and stinging nettle leaves [23, 24]. It seems relevant to evaluate the effect of specialized formulas for nursing mothers with lactogenic additives on the formation of lactation in women after term birth. For evaluation, we chose the NutriMa Lactamil product as it contains the largest number of lactogenic additives.
The purpose of this study was to examine the effectiveness of the use of the specialized product NutriMa Lactamil to stimulate and support lactation in nursing women after childbirth.
The objectives of the study included:
1) assess the effect of the product on lactation in women; 2) evaluate the factors leading to hypogalactia in lactating women; 3) find out the individual attitude of nursing mothers to the NutriMa Lactamil product; 4) evaluate the effect of maternal intake of the NutriMa Lactamil product on the condition of the newborn child.
Materials and research methods
The effectiveness of the NutriMa Lactamil product was studied at the Chelyabinsk Regional Clinical Hospital No. 2, in the department of pathology of newborns and premature infants.
Breastfeeding women and full-term newborns were under observation. A total of 105 women and 105 newborns were included in the study. All women had singleton pregnancies and delivered full-term infants between 37 and 41 weeks of gestation. Breastfeeding women and newborn babies were divided into two groups. The criterion for dividing into groups was the use of the NutriMa Lactamil product in the nutrition of nursing mothers. To assess lactation in the study groups, the average daily volume of breast milk was studied. All women were in the department of pathology of newborns and premature infants for child care and received equivalent standard nutrition for nursing mothers in the hospital.
The first group included nursing mothers and newborns who used the NutriMa Lactamil product in their diet. The group consisted of 50 mothers and 50 full-term newborns. NutriMa Lactamil was taken in an amount of 400 ml per day (2 times a day, 200 ml per dose). Women received the product from 3 days to 17 days after birth (14 days). Breastfeeding mothers filled out questionnaires in which they assessed taste qualities, personal feelings regarding the effect on lactation, and indicated their attitude towards continuing to take the product after the end of the study. The second group included mothers and full-term newborns whose mothers did not take NutriMa Lactamil (control group). The second group consisted of 55 women and 55 full-term children. Nursing mothers in the study and control groups did not additionally use any other means to correct nutrition and stimulate lactation. In the 1st and 2nd groups, mothers were advised on breastfeeding by a neonatologist together with a consultant from the Association of Breastfeeding Consultants in Chelyabinsk.
The groups were comparable in terms of women's age, gestational age, and parity of pregnancy and childbirth. The average age of mothers in group 1 was 29.0 years (from 19 to 40 years), in group 2 it was 28 years (from 19 to 38 years). The average gestational age in group 1 was 38 weeks (from 35 weeks to 40 weeks), in group 2 - 37.5 weeks (from 35 weeks to 40 weeks). The studied groups of women were comparable in the nature of genital and somatic pathology. The studied groups of newborn children were comparable in the nature and severity of the existing perinatal pathology. Lactation volume in women was measured daily. Newborn babies were fed at the breast. The daily volume of lactation was calculated based on control feedings, as well as on the basis of the volume of expressed breast milk. Assessment of the effect of the product on the condition of the newborn took into account the presence of dyspepsia and gastrointestinal dysfunction. After the end of the study, the percentage of breastfeeding in newborns at a postnatal age of 1 month in the study and control groups was assessed. Statistical data processing was carried out using the Exel 2016 and Statisica 6.0 software package. Arithmetic means, standard deviation and standard error were determined. The Student's test, chi-square test, and correlation coefficient were calculated. Data are given as arithmetic mean and standard deviation (M ± δ). Differences were considered significant at p < 0.05.
Results and discussion
The effect of the NutriMa Lactamil product on supporting lactation in lactating women
There were no significant differences between the study and control groups of lactating women in the amount of breast milk on the 3rd day after birth. However, on the 17th day after birth, the daily volume of breast milk in lactating women in the study and control groups was significantly different. Mothers taking the NutriMa Lactamil product had greater milk production than those in the control group (Table).
The effect of using the NutriMa Lactamil product in the form of an increase in the amount of breast milk in nursing women occurred after 14 days of using the product.
At the age of one month after birth, the percentage of children who were fully breastfed was assessed in the study and control groups. In group 1, the percentage of breastfeeding in children was 96.0% (48 women out of 50). In group 2, the percentage of breastfeeding was significantly lower (p < 0.05) and amounted to 63.6% (35 women out of 55).
Assessment of factors leading to hypogalactia in lactating women
In the study groups, there was no relationship between the amount of breast milk and complications of pregnancy and childbirth. 44.5% of women in group 1 and 47.1% in group 2 had a history of abortion. Toxicosis was recorded in 44.8% of mothers in group 1 and in 43.5% in group 2. In group 1, gestosis was present in 30.4% of women, in group 2 in 28.1% of women. Polyhydramnios and oligohydramnios were recorded in 15.4% and 14.8% of women, respectively. There was a threat of miscarriage in the 1st group in 12.1% of cases, in the 2nd group in 11.4% of cases.
In group 1, the rate of birth of children by cesarean section was 25.1%, and by natural birth - 74.9%. In group 2, the rate of birth by cesarean section was 23.7%, and by natural birth - 76.3%. In both groups, the volume of milk in women on the 3rd day after surgical birth was less compared to women who gave birth independently (170 ± 20 ml versus 250.5 ± 52 ml (p < 0.05) in group 1 and 165 ± 30 ml versus 248 ± 47 ml (p < 0.05) in group 2, respectively). It is important to note that in groups 1 and 2, there were no significant differences in the volume of lactation on the 17th day after birth depending on the type of delivery.
Individual attitude of nursing mothers to the NutriMa Lactamil product
80% of mothers (40 out of 50 mothers) noted the presence of a herbal taste. Breastfeeding mothers described the taste as “milk with herbal flavor,” “milk with dill,” “milk with spices,” and “milk and herbal taste.” 80% of mothers (40 out of 50 respondents) liked the taste of the product. 18% of women (9 women out of 50) found it difficult to answer the question: “Did you like the taste of the product?” One mother (2%) did not like the taste of the product. Despite the fact that only 80% of nursing mothers liked the taste of the NutriMa Lactamil product, the survey results showed that the majority of mothers are ready to continue taking the product - 96% (48 mothers out of 50). And only 2 women (2 out of 50; 4%) noted that they do not plan to continue taking NutriMa Lactamil in the future. An increase in the amount of breast milk after taking the formula was noted by 96% of women (48 out of 50 women). Only 4% of women did not feel a significant effect from taking it (2 women out of 50).
Evaluation of the effect of maternal intake of the NutriMa Lactamil product on the condition of the newborn child
The average daily gain in children in the 1st group was 26 ± 5 g/kg/day, in the 2nd group 25 ± 6 g/kg/day. The duration of preservation of the loss of body weight from birth in newborns of the 1st group was 5 ± 2 days, in children of the 2nd group 4 ± 2 days. There were no significant differences between the 1st and 2nd groups in the number of regurgitations, the nature and frequency of stools. In the study group, a significantly lower incidence of flatulence was recorded (flatulence in 30% of children; 15 out of 50 children) compared to the control group (flatulence in 47.2% of children; 26 out of 55 children). We associated the decrease in the frequency of flatulence in children with the fact that the NutriMa Lactamil product contains anise, cumin and fennel, which are used in pediatrics to eliminate colic and increased gas formation in babies.
Conclusion
First of all, to stimulate lactation, prevent and treat hypogalactia, it is necessary to counsel nursing women on breastfeeding issues [1, 3–5, 8]. The indication for the prescription of lactogonic drugs is insufficient production of breast milk in healthy mothers, which persists after counseling the family on breastfeeding issues [1, 3, 8]. Lactagogues will not be effective unless there is adequate support for breastfeeding from medical personnel and families [1, 4, 8].
Despite the fact that many lactogonic agents have been used for quite a long time to stimulate lactation, currently few studies have been published assessing the effectiveness of lactogonic agents [1, 3, 4, 8].
The study confirmed the clinical effectiveness of the NutriMa Lactamil product for stimulating lactation and preventing hypogalactia in nursing women after term birth. The use of the NutriMa Lactamil product in nursing mothers after childbirth in a dosage of 200 ml 2 times a day for 2 weeks leads to a significant increase in the amount of breast milk and subsequently helps to increase the frequency of breastfeeding, including after surgical delivery. Most mothers are determined to continue taking NutriMa Lactamil, noting its effectiveness. When nursing mothers take the NutriMa Lactamil product, intestinal flatulence in children is less common. The use of the NutriMa Lactamil product in the nutrition of nursing women helps to additionally provide the body of a nursing woman with complete protein, energy, omega-3 fatty acids, vitamins, macro- and microelements. The dairy product NutriMa Lactamil can be reasonably included in the complex of therapeutic measures for the prevention and treatment of hypogalactia in lactating women.
Literature
- The Academy of Breastfeeding Medicine Protocol Committee ABM clinical protocol No. 9 (Second Revision 2018) // Breastfeeding Medicine. 2018; 13 (5): 307–314.
- Protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services. World Health Organization, 2022. 120.
- Zhdanova S.I. Prevention and treatment of hypogalactia. The role of lactogenic agents // Medical Council. 2018; 2:26–31.
- Zubkov V.V. Prevention and correction of hypogalactia in nursing women // Medical Council. 2016; 12: 138–140.
- Keshishyan E. S., Balashova E. D. Hypogalactia in nursing women and methods of its correction // Pediatric practice. 2013; March-April: 23–26.
- Chantry CJ, Dewey KG, Peerson JM, Wagner EA, Nommsen-Rivers LA In-hospital formula use increases early breastfeeding cessation // Journal of Pediatrics. 2014, 164 (6): 1339.
- Ryumina I.I., Evteeva N.V., Onishchenko Yu.G. The role of expressing breast milk in maintaining effective lactation // Questions of practical pediatrics. 2013; 8 (4): 74–76.
- The Academy of Breastfeeding Medicine Protocol Committee ABM clinical protocol No. 9 (first revision January 2011) // Breastfeeding Medicine. 2011; 6 (1): 41–49.
- Zhdanova S.I., Galimova I.R., Idiatullina A.R. Initiation of lactation - myth or reality? // Neonatology: news, opinions, training. 2017; 1:93–97.
- Biewenga J., Keung C., Solanki B., Natarajan J., Leitz G., Deleu S., Soons P. Use of Domperidone: A Systematic Review of the Benefit-Risk Ratio // J Hum Lact. 2015, February, 31: 57–63.
- Bazzano AN, Hofer R., Thibeau S., Gillispie V., Jacobs M., Theall KP A Review of Herbal and Pharmaceutical Galactagogues for BreastFeeding // Ochsner J. 2016, Winter, 16 (4): 511–524.
- Haase B., Taylor S., Mauldin J., Johnson TS, Wagner CL Domperidone for Treatment of Low Milk Supply in Premature Infants: A Clinical Protocol // J Hum Lact. 2016, 32(2): 373–381.
- Javan R., Javadi B., Feyzabadi Z. Breastfeeding: A Review of Its Physiology and Galactogogue in View of Traditional Persian Medicine // Breastfeed Med. 2022, Sep, 12(7): 401–409.
- Alachkar A., Jaddouh A., Elsheikh MS, Bilia AR, Vincieri FF Traditional medicine in Syria // Nat Prod Commun. 2011, Jan, 6(1): 79–84.
- Bazzano AN, Cenac L., Brandt AJ, Barnett J., Thibeau S., Theall KP Maternal experiences with sources of information on galactagogues // Int J Womens Health. 2022, 9: 105–113.
- Winterfeld U., Meyer Y., Panchaud A., Elnarrson A. Management of deficient lactation in Switzerland and Canada: a survey of midwives' current practices // Breastfeed Med. 2012, August, 7: 317–318.
- Hale TW, Hartmann PE Hale & Hartmann's Text book of Human Lactation. 1st ed. Hale Publishing, LP, Amarillo, TX, USA: 2007.
- Ghasemi V., Kheirkhah M., Samani LN The effect of herbal tea containing fennel seed on breast milk sufficiency signs and growth parameters of Iranian infants // Shiraz E Med J. 2014, 15: e22262.
- Ghoshegir S.A., Mazaheri M., Ghannadi A., Feizi A., Babaeian M., Tanhaee M. Pimpinellaanisum in the treatment of functional dyspepsia: A double-blind, randomized clinical trial // J Res Med Sci. 2015, 20: 13–21.
- Foong SC, Tan ML, Marasco LA Oral galactagogues for increasing breast-milk production in mothers of nonhospitalized term infants // Cochrane Libr. 2015, 4: CD011505.
- Abdulrazzaq YM, Al Kendi A., Nagelkerke N. Soothing methods used to calm a baby in an Arab country // Acta Paediatr. 2009, 98: 392–396.
- Sim TF, Hattingh HL, Sherriff J., Tee LB The use, perceived effectiveness and safety of herbal galactagogues during breastfeeding: a qualitative study // Int J Environ Res Public Health. 2015; 12(9):11050–11071.
- Baby nutrition: a guide for doctors / Ed. Tutelyana V. A., Konya I. Ya. 4th ed. M.: MIA, 2022. 777 p.
- Kiosov A.F. Support of lactation after premature birth // Issues of pediatric dietology. 2014; 6:51–55.
A. F. Kiosov, Candidate of Medical Sciences
GBUZ OKB No. 2, Chelyabinsk
Contact Information
DOI: 10.26295/OS.2019.82.82.001
Support of lactation, prevention and treatment of hypogalactia / A. F. Kiosov For citation: Attending physician No. 6/2019; Page numbers in the issue: 7-11 Tags: nursing women, breastfeeding, prolactin
For hair growth and scalp care
In cosmetology, it is widely known as the best helper for hair loss. The author of the medieval medico-pharmacological treatise in Latin verse “On the Powers of Herbs” mentioned it as an effective remedy for hair growth and strengthening. There are many cosmetic recipes using nettle decoction; modern manufacturers make products based on this hot plant, but we still offer recipes so that you can independently make home cosmetic procedures for the health and beauty of your hair.
- To stimulate growth and shine: take 100 grams of leaves, finely chop, add 0.5 cups of vinegar, 0.5 cups of water. The mass must be boiled for half an hour, then cooled and rubbed into the scalp 2-3 times a week.
- Mask for growth: add pharmacy vitamin E capsules to nettle juice. This mask will help well for the growth and strengthening of curls. It is recommended to rub it into the roots once a week for best results.
- Mask for oily hair: take fresh herb and grind it in a blender. You need to add a teaspoon of salt to the resulting mixture. The resulting paste should be applied to the hair and rubbed in gently. Then you need to wrap your head in plastic and wrap it in a towel. After 20 minutes, wash off. This mask can be applied no more than twice a week.
- For a general strengthening effect: take 1 tsp. dried nettle leaves, 1 tsp. sage, 1 tbsp. l. dried chamomile flowers and 2 glasses of water. Boil water, place the herbs in a mug or jar and fill it all with hot water. Cover with a lid and let steep until the broth has cooled. After this, strain the infusion through cheesecloth and use while showering or after.
- To combat early gray hair or seborrheic disease: take 100 grams of leaves, chop and boil in one glass of water. You can rinse your hair with this infusion 3-4 times a week.
- For lightening hair. A suitable option for blondes. To obtain a brightening effect, brew nettle leaves and chamomile flowers mixed in equal proportions. Then strain the infusion and rinse your hair with it. Next, wrap the wet curls in a bag or plastic wrap and a towel for 60 minutes. Afterwards, rinse your hair again with the remnants of the cooled infusion.
- Scalp scrub. You need to grind rye bran and nettles in a blender. Add finely ground salt (extra) to the mixture. Then use the mass to cleanse the skin of sebaceous secretions and dandruff once a week.
- Revitalizing mask. Take 1 cup of crushed leaves, 50 g of yeast, 3 tbsp. l. honey and vegetable oil. Mix everything and stir for a long time until smooth. The mask is designed for only 30 minutes, then rinse your hair thoroughly with water and be sure to use shampoo.
Literature:
- Nettle (genus of plants) // Great Soviet Encyclopedia M.: Soviet Encyclopedia, 1969-1978.
- Lavrenova G.V., Lavrenov V. Encyclopedia of medicinal plants.
- Yuri Konstantinov “Nettle. A unique natural medicine."
- Daria Veryasova "Nettle". Ivan Dubrovin “All about ordinary nettles.”
- I. P. Neumyvakin “Nettle: myths and reality”, 2022.
- Akhmetov R.B. “Overcome the grass.”
- Polevaya M. A. "St. John's wort and nettle - natural power."
Collection and storage of nettles
The collection of nettle leaves usually occurs in May-July. The leaves are either torn off immediately (you just need to do this with gloves to protect your hands), or you first mow down the plant, dry it, and only then collect the leaves.
Is it necessary to pour boiling water over nettle leaves?
They can be used fresh (for example, squeeze the juice out of them), but before using the leaves should be doused with boiling water so that the plant stops “burning”.
Cutting nettles for drying.
Drying nettles
Most of the raw materials need to be dried. Do this only in a well-ventilated area (for example, in the attic), or under a canopy. You can also use special dryers, laying out the leaves in a thin layer and making sure that the temperature does not rise above +40...+50 °C. Please note that the total mass of dried raw materials will be no more than 20% of the mass of fresh ones.
The main thing is to never dry the raw materials in the open sun: this can not only spoil the appearance of the leaves, but also destroy some of the vitamins that make up them.
Dried leaves can be stored for 2 years, in a ventilated area away from direct sunlight. ! Nettles should be collected for medicinal, cosmetic or culinary purposes away from highways, as the plant easily absorbs harmful substances and can be dangerous.
Collection of fresh nettles.