Symptoms of persistent constipation
Frequent constipation is often accompanied not only by difficulties and rare bowel movements. They can be characterized by the appearance of mucus and blood in the stool, pain in the rectum and perianal area. This is due to mechanical trauma to tissues from dense stools.
The normal frequency of bowel movements is three times a day to three times a week. The shape of the stool also matters—with constipation, it is denser.
Associate professors of the Department of Internal Diseases Babieva A. M., Bogatyrev V. G., Marinchuk A. T., Koumbatiadis D. G. believe that “constipation contributes to the development of various diseases, reduces quality of life by 20% and is one of the early risk factors the occurrence of pancreatic, gallbladder and colorectal cancer" (Babieva, Bogatyrev, Marinchuk, Koumbatiadis, 2012, p. 52).
Causes of prolonged constipation
There are several reasons for the development of persistent constipation. The most common is poor nutrition, namely a lack of dietary fiber and a predominance of refined foods.
Professor Livkin V.L. believes that “a common cause of the development of chronic disease is a change in the intestinal microflora due to disruption of the production of specific substances by representatives of the normal flora of the colon that promote the formation of stool and support optimal motor activity of the colon” (Livkin, 2013, p. 78).
Constipation can be caused by other factors:
- physical inactivity;
- violation of the water regime;
- intestinal dysbiosis;
- endocrine diseases;
- tumors of the digestive system;
- inflammatory diseases of the gastrointestinal tract;
- proctological diseases;
- neurological diseases.
Also, stool retention may be associated with taking medications. Drugs that can cause constipation as a side effect include drugs to normalize blood pressure and heart rate, antibacterial drugs, hormonal drugs, antiepileptic drugs, diuretics, tranquilizers, iron supplements and others.
By type of reason
Depending on the causes of frequent constipation, they are classified into several types:
- alimentary or nutrition-related;
- neurogenic;
- proctogenic;
- dyskinetic;
- hypodynamic;
- psychogenic;
- medicinal.
The head of the department of gastroenterology of the State Healthcare Institution ROCH Babieva A.M. and other authors believe that “constipation in 80–90% of cases is of a functional nature, the rest is caused by reasons of an organic nature” (Babieva A.M., Bogatyrev V.G., Marinchuk A. T., Koumbatiadis D. G., 2012, p. 53).
By gender and age
Gender and age act as risk factors for the development of constipation. In women, this disorder of intestinal function is more common, developing, among other things, during pregnancy and after childbirth.
According to various sources, up to 60–80% of people over 60 years of age suffer from constipation, which may be due to disturbances in the transmission of nerve impulses, overstretching of the intestinal walls, developed proctological diseases, a sedentary lifestyle and other factors.
Get rid of intestinal problems
The natural British drug is not addictive and works immediately
Find Fitomucil with benefits
Functional constipation: some treatment approaches
The article analyzes the causes of constipation, the stages of the diagnostic search, and the drugs used for this disease. The domestic drug Exportal (international nonproprietary name lactitol), which belongs to the group of osmotic laxatives, is examined in detail. During clinical studies in a group of 30 elderly and senile patients (from 65 to 81 years old) with chronic functional constipation, the effectiveness, safety and tolerability of this drug were assessed. It turned out that Exportal has higher clinical effectiveness in the treatment of chronic constipation compared to Forlax.
Table 1. Causes of constipation
Table 2. Stages of diagnostic search for constipation
Table 3. Dynamics of clinical symptoms in patients with chronic constipation before and after treatment with Exportal
Table 4. Comparative assessment of the effectiveness of treatment of patients with chronic constipation with Exportal and Forlax (p < 0.05)
Rice. 1. Mechanism of action of Exportal
Table 5. Dynamics of SCLC parameters #
Constipation is a delay in bowel movement for more than 48 hours, accompanied by a feeling of incomplete bowel movement with the passage of a small amount (less than 35 g) of stool of increased hardness.
Functional constipation is constipation that is not associated with known genetic, structural and organic changes in the intestine.
An international group of experts has developed criteria for functional constipation (Rome III criteria, 2006). So, constipation is considered functional if:
- its symptoms began at least 6 months ago and persisted for the last 3 months before diagnosis;
- there are no sufficient criteria for diagnosing irritable bowel syndrome (IBS);
- bowel movements rarely occur on their own without the use of laxatives.
Diagnostic criteria for functional constipation must include 2 or more of the following symptoms occurring in at least 25% of bowel movements:
- straining;
- rough or hard stools;
- sensation of anorectal obstruction (blockage) during bowel movements;
- the need for manual techniques to facilitate the evacuation of feces;
- less than three bowel movements per week with small amounts of stool (stool weight less than 35 g/day).
According to the accepted classification, constipation is distinguished:
- according to the course (acute and chronic);
- by development mechanisms: – predominant violation of evacuation (mechanical obstruction, anomaly); – predominant motor impairment (with a predominance of hypokinesia, hyperkinesia, mixed form) – cologenic; – disorder of the defecation reflex from the rectum – proctogenic;
- according to the stage of the course (compensated, subcompensated (stool once every 10 days), decompensated).
Acute constipation develops with obstruction of the large intestine (obstructive or strangulating ileus). In addition to stool retention, in this case there is a delay in the passage of gases, flatulence, colicky pain of an increasing nature, vomiting, collapse, and symptoms of general intoxication appear. Treatment is surgical. Abnormalities in intestinal development also require surgery.
Chronic constipation is much more common, the development of which is caused by various causes (Table 1), which must be taken into account when choosing treatment.
Doctors often take a simplified approach when diagnosing constipation. At the same time, the reluctance to clarify the mechanism of development of constipation leads to loss of time, consolidation of reflex connections, the development of secondary changes in the intestine and “fixation of the situation” in general, i.e. transition of functional pathology to organic.
It should be noted that during the diagnostic examination, special attention should be paid to a thorough assessment of intestinal symptoms and circumstances contributing to the development of constipation [3]. The use of special research methods is required only in some patients.
A program for examining patients has been developed, including certain diagnostic measures at various stages of the search (Table 2), which allows us to get an answer to the main question - whether constipation is caused by a disease or is a functional disorder.
Treatment of functional constipation
A necessary condition for the treatment of chronic constipation is dietary measures depending on the type of intestinal motor-evacuation disorders. Thus, with hypomotility, the diet is based on the type of “slag load” (vegetables, fruits, berries - mostly raw, at least 200 g / day). For hypermotility (spastic dyskinesia), the diet is more gentle: boiled vegetables, vegetable fats.
In this case, an important component of treatment is compliance with the drinking regime (at least 1.5–2 l/day).
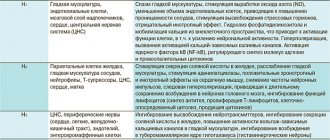
Physical activity and the elimination of negative drug effects are of great importance in the complex of measures to eliminate constipation. Drug therapy includes the use of drugs that affect colon motility and laxatives. The use of drugs that affect motility is determined by the pathophysiological mechanisms underlying primary motor disorders of the colon. To slow down the propulsive activity of the intestine, antispasmodics, M-anticholinergics, opiates, calcium channel blockers, etc. are used.
For hypomotor dyskinesia, drugs that enhance peristalsis are used: metoclopramide, the 5-HT4 receptor antagonist tegaserod, which has shown high efficiency, the motility regulator trimebutine (Debridate), a stimulator of all types of opiate receptors. In young and middle-aged people, the combined drug Meteospasmil (alverine + simethicone) can be used in a course of 1 capsule 2 times a day for 3 weeks. According to our data, restoration of motility and relief of constipation was registered in 67% of patients.
For spastic (hypermotor) dyskinesia, myotropic antispasmodics are used: – nitric oxide donors; – phosphodiesterase type IV inhibitors; – calcium channel blockers of partially selective action – pinaveria bromide (Dicetel) and otilonium bromide (Spasmomen); – blockers of peripheral serotonin receptors; – sodium channel blockers – mebeverine (Duspatalin).
If the above measures are ineffective, the key stage of treatment is the use of laxatives. In addition, there are a number of absolute indications for the use of laxatives: prolonged bed rest; inadmissibility of increasing intra-abdominal pressure during straining (myocardial infarction, aneurysms, thrombosis, hernias, fissures, etc.); drug-induced constipation; dementia.
The following groups of laxative drugs are distinguished.
- Increasing the volume of intestinal contents (containing plant hydrophilic fibers: bran, seaweed (kelp), flaxseed, plantain seeds, agar-agar; methylcellulose preparations (Mukofalk 10–15 g/day), etc.).
- Osmotic laxatives (Forlax - polyethylene glycol with a molecular weight of 4000, saline laxatives (magnesium sulfate, sodium sulfate, Carlsbad salt), alcohols (sorbitol, mannitol), synthetic disaccharides (lactulose), lactitol (Exportal)).
- Softening feces (vaseline, castor, almond and other oils, paraffin).
- Drugs that stimulate intestinal function (anthraglycosides - rhubarb, buckthorn, senna preparations; Guttalax, bisacodyl (Dulcolax), Agiolax, etc.; combination drugs - Kafiol, Kalifit, Andrews Liversalt, Mucinum, Agarol; herbal laxatives in various combinations).
- Lubricants (mineral oils, glycerin suppositories, castor oil).
Currently, the principles for choosing laxatives and treatment tactics have been developed, including the following provisions.
- The choice of drug is made depending on the leading pathological mechanism of constipation.
- When the mechanism of motor disorder is complex, a combination of drugs with different mechanisms of action is advisable.
- During the treatment process, the drug should be changed and the dose adjusted (since either addiction develops or the sensitivity of receptors to the perception of motor stimuli increases).
- Depending on the effect, you should change the rhythm of administration, the dose of laxatives, and take breaks in treatment.
- It is necessary to take into account the patient’s initial condition (age, concomitant diseases, electrolyte balance), since the use of laxatives may be accompanied by loss of electrolytes, impaired synthesis of B vitamins, etc.
The most commonly used group of laxatives are osmotic agents. Their action does not impair the sensitivity of the receptors; moreover, when they are used, the sensitivity of the receptors is restored. However, the effect of drugs in this group is not clear.
Thus, alcohols with a relatively short chain of 3–6 carbon atoms (sorbitol, mannitol, glycerin) and saline laxatives act at the level of the small intestine and promote the release of large amounts of fluid into its lumen, which is accompanied by dilution of the stool, often to the point of diarrhea. In addition, saline laxatives act quickly (within 2 hours), but are not suitable for long-term treatment (water-electrolyte imbalance is pronounced).
Forlax (macrogol 4000) [2] is not absorbed, not metabolized, it forms additional hydrogen bonds in the intestinal lumen, due to which the volume of intestinal contents increases, the consistency softens, and the urge to stool is formed.
Preparations of the synthetic disaccharide lactulose (Duphalac and others) have proven themselves to be effective, which are not absorbed in the small intestine and are broken down with the help of saccharolytic flora, first to fructose and galactose, and ultimately to short-chain (volatile) fatty acids, which provides an osmotic effect and promotes increasing the biomass of indigenous flora.
Currently, a new domestic drug Exportal [1, 4] (international nonproprietary name - lactitol), which also belongs to the group of osmotic laxatives, has appeared on the Russian market. The active ingredient is lactitol monohydrate (polyhydric alcohol), which provides a rapid therapeutic effect in the absence of side effects (the drug does not act in the small intestine) characteristic of this subgroup of drugs (alcohols).
In addition, the products of lactitol metabolism, which (like lactulose) are formed in the colon under the influence of enzymatic breakdown of obligate flora with the formation of short-chain fatty acids, carbon dioxide and water, have osmotic properties. These products are not absorbed and increase osmotic pressure, increasing the volume of intestinal contents due to increased biomass (energetic effect of volatile fatty acids) (Fig. 1).
We assessed the effectiveness of the drug Exportal in 30 elderly and senile patients (from 65 to 81 years) with chronic functional constipation. Duration of constipation up to 5 years was observed in 3 patients, up to 10 years – in 9, up to 20 years – in 11, over 20 years – in 7 patients. All patients had concomitant pathology (cardiovascular, digestive), but at the time of inclusion in the study they did not receive drugs that affect intestinal motility.
All patients were taking various laxatives with a temporary unstable effect before inclusion in the study.
Exportal was prescribed 2 sachets (or 4 teaspoons) of powder per day for 20 days. Depending on the effectiveness of treatment, the dose of the drug was adjusted.
The effect was assessed by the dynamics of clinical manifestations, the results of electrogastroenteromyography, the intestinal transit time of activated carbon - carbolene test (normal transit is 24-48 hours), short-chain fatty acids (SCFA*) were also determined in the feces before and after treatment.
Tolerability and safety of the drug were assessed using observation diaries, biochemical blood profiles, and general blood and urine tests.
The treatment results are presented in Table 3, from which the positive dynamics of all clinical manifestations can be seen. At the same time, I would like to note that formed stool was noted in 63.3% of patients, in the remaining patients the stool became soft, semi-formed; the need for straining disappeared or significantly decreased in the vast majority of patients. In 4 patients, in the first days of treatment, the dose of the drug was increased to 3 sachets per day. This increase was temporary until constipation was permanently relieved, then the dose remained the same - 2 sachets per day; in 2 patients the dose of the drug was soon reduced to 1 sachet. Five patients (16.7%) noted the appearance of flatulence, which was temporary and did not require discontinuation of the drug.
The overall effectiveness in relieving clinical manifestations was 84.7% with a rapid (in the first 4–5 days) onset of daily bowel movements; transit through the intestines was normalized (according to the results of the carbolene test), the power of contractions increased and the rhythmicity coefficient was restored (according to electrogastroenteromyography).
The quantitative and qualitative content of short-chain fatty acids in feces over time was studied using gas-liquid chromatographic analysis (GLC analysis).
It was found that initially there was a significant decrease in the total absolute content of acids, a change in the profile (i.e., relative content) of acetic, propionic and butyric acids, a deviation of the values of the anaerobic index, reflecting the redox potential of the intraluminal intestinal environment, from the range of normal values, and also an increase in the total relative amount of isoacids. The identified changes in SCFA parameters indicated an initial decrease in the activity and abundance of obligate microflora, including lactic acid (bifidobacteria and lactobacilli), a violation of the qualitative composition of microorganisms with dominance in some cases of aerobic (type 1), in other anaerobic (type 2) populations of microorganisms, moreover, their facultative and residual strains, changes in the proteolytic activity of microflora due to changes in its habitat.
After treatment, there was a pronounced tendency towards restoration (in some cases normalization) of the above-mentioned SCFA parameters, indicating restoration of the activity and composition of the colon microflora, which was associated with both the metabolic effect of Exportal and the restoration of intestinal transit.
These data allowed us to draw the following conclusions.
- Exportal is an effective drug for the treatment of chronic functional constipation in elderly and senile patients.
- The effect of the drug is due to: – normalization of motor activity of the colon; – restoration of the disturbed intestinal ecosystem.
- The drug is well tolerated and has a minimum (3.3%) of side effects (moderate flatulence that occurred at the beginning of treatment in some patients, which did not require changes in doses and nature of treatment).
The second part of this study was a comparative analysis of the clinical effectiveness of the drugs Exportal (FPK PharmVILAR, Russia) and Forlax (Ipsen, France) in the treatment of chronic constipation. Forlax was chosen for comparison due to the fact that today it is the most commonly used drug from the group of osmotic laxatives.
To compare the effectiveness of the drugs, 60 elderly and senile patients who suffered from chronic constipation were examined and treated.
2 comparison groups were formed:
- Group 1 – 30 people who received Exportal;
- Group 2 – 30 people who received Forlax.
The average age of patients in group 1 was 74.9 ± 6.9 years (from 65 to 81 years), of which 6 were men and 24 were women. The characteristics of patients in group 2 were comparable. The duration of constipation in most patients was more than 10 years.
Before inclusion in the study, all patients received laxatives (receptor, volume type); some patients (approximately 10%) used cleansing enemas.
Patients of the 1st group received Exportal 2 sachets per day, patients of the 2nd group received Forlax in the same amount. The duration of treatment was 20 days.
The clinical picture was assessed according to the working scheme before treatment and after the course of therapy. The intensity of the main clinical symptoms of the disease was determined. To determine the effectiveness of treatment in each group (main and comparison groups), the number of patients who achieved clinical remission, significant improvement, improvement, and those who did not achieve clinical improvement was counted. Clinical remission was considered the absence of disease symptoms. Significant improvement was noted with a decrease in clinical symptoms by more than 50%. An improvement was defined as a decrease in clinical symptoms of less than 50%.
For statistical processing, the effectiveness of treatment was expressed in points. A score of 0 points meant no effect of treatment, 1 point meant improvement, 2 points meant significant improvement, and 3 points meant clinical remission.
The comparative effectiveness of treatment of patients with chronic constipation with Forlax and Exportal is presented in Table 4, from which it can be seen that the effectiveness of therapy when using Forlax was 80.7% (1.90 ± 0.09 points), when using Exportal - 84.7% ( 2.26 ± 0.11 points), which indicates the advantage of the latter.
In addition to clinical indicators, other recorded tests have also changed. Thus, the transit time for the carbolene sample against the background of Exportal accelerated from 69.7 ± 6.9 hours to 35.3 ± 5.6 hours; during treatment with Forlax – from 68.4 ± 3.9 to 46.3 ± 2.4 hours.
The appearance of flatulence during treatment was recorded with almost the same frequency; however, in the group of patients taking Forlax, other side effects were identified (belching, transient abdominal pain), amounting to a total of 6.5%.
An increase in the dose of the drug was required in 9 patients during treatment with Forlax, and in 5 patients during treatment with Exportal.
The dynamics of electrical activity and the rhythmicity coefficient changed towards normalization in both groups, but in patients receiving Exportal, the shift was more pronounced.
The dynamics of SCFA parameters (Table 5) turned out to be more reliably expressed in patients receiving Exportal, which is associated not only with the normalization of transit, but also with the restoration of the activity and composition of the intestinal microflora. Consequently, in the 1st group, direct - metabolic - and indirect effects of restoring the composition of the intestinal microflora were recorded, and in the 2nd group of patients receiving Forlax, only an indirect effect was recorded, which depends on the restoration of intestinal transit.
The presented data allowed us to draw the following conclusion.
- Exportal has higher clinical efficacy in the treatment of chronic constipation in elderly and senile patients (84.7% versus 80.7% with Forlax treatment; 2.26 ± 0.11 and 1.90 ± 0.09 points, respectively); low incidence of side effects (3.3% and 6.5%, respectively) and faster response to therapy (3.5 ± 1.5 and 5.5 ± 2.5 days).
- The more pronounced effect of Exportal compared to Forlax is associated with a direct (metabolic) effect on the intestinal microflora and with a more pronounced indirect effect associated with the normalization of intestinal transit.
Treatment of chronic constipation
Your doctor will tell you what to do if you have persistent constipation; if you have a chronic problem, it is important to see a therapist or gastroenterologist. Many patients self-medicate by uncontrollably taking laxatives or using cleansing enemas on a regular basis. This may cause the condition to worsen.
Thus, Professor Parfenov A.I. writes that “the systematic use of cleansing enemas inevitably leads to the formation of an inert colon due to the loss of visceral sensitivity and defecation reflex” (Parfenov, 2013, p. 100). To cure chronic constipation, it is important to adjust your diet and not uncontrollably take laxatives.
It is worth understanding that long-term constipation requires complex treatment. There are several directions in which you can act to normalize stool.
Consultation with a gastroenterologist
Contacting a specialist is mandatory if constipation does not occur just once due to certain circumstances, but is observed systematically or appears from time to time. The doctor will examine the clinical picture, listen to complaints, collect anamnesis and prescribe diagnostic methods to identify the exact causes of intestinal dysfunction. These include:
- laboratory blood tests;
- stool examinations, including occult blood tests;
- colonoscopy, irrigoscopy according to indications, etc.;
- FGDS;
- Ultrasound of the abdominal organs.
During the initial consultation, the gastroenterologist will talk about possible causes and provide referrals for research. At the second appointment, based on the results of the completed diagnostics, the exact diagnosis will be known.
In the vast majority of cases, chronic constipation is associated with dietary habits. But sometimes the doctor deals with diseases of the gastrointestinal tract accompanied by constipation. These include the following:
- dolichocolon;
- intestinal diverticulosis;
- peptic ulcer;
- cholelithiasis;
- intestinal tumors;
- haemorrhoids.
A number of diseases lead to disruption of the digestive processes and contraction of the intestinal muscles, others represent a mechanical obstacle to the movement of feces.
Diet to get rid of constant constipation
Nutrition for chronic constipation should be revised in the direction of replenishing the diet with fiber. A high amount of dietary fiber is found in bran, fresh vegetables, fruits, and dried fruits.
However, to get your daily fiber intake you will need to eat a lot of fiber-rich foods. This can be difficult, so sometimes it makes sense to find a source of dietary fiber in the form of a supplement.
Regular use of fiber will help speed up the movement of stool through the intestines and ensure regular spontaneous bowel movements.
It is important to pay attention to the drinking regime. Drinking less than 1.5–2 liters of water per day can lead to excessive absorption of water in the intestines and dehydration of stool. Therefore, it is necessary not only to drink enough fluid, but also to avoid losing it - eliminate or reduce the consumption of drinks with a diuretic effect. These include tea and coffee.
It is better to exclude from the diet foods and dishes with an astringent, fixing effect: +
- crackers, confectionery products made from premium flour;
- fatty food;
- confectionery;
- peeled rice;
- jelly.
The menu for chronic constipation must include vegetable oils, vegetables and fruits, wholemeal bread, and dairy products without sugar. It is better to choose low-fat poultry, meat and fish, and prefer cereals as side dishes.
Preventive measures
The diet should contain a lot of vegetables, fruits, cereals and wholemeal flour; you can add wheat and oat bran as sources of fiber. It is better to cook vegetable soups. The child should drink a normal amount of liquid - fruit drinks, compotes, clean water, juices.
One of the most important conditions for normal bowel function is constant moderate physical activity. Any kind of sports or even just regular walks will be very useful.
You need to teach your child how to sit on the toilet correctly. Your feet are on the floor, your knees are bent, you can even raise your knees a little by placing a small bench under your feet, your torso is tilted forward. There is no need to push; on the contrary, you need to relax so that the intestines themselves perform the act of defecation.
Sources:
- P.L. Shcherbakov, L.N. Tsvetkova, V.V. Kashnikov. Chronic constipation in children // Issues of modern pediatrics, 2005, vol. 4, no. 4, pp. 54-62.
- HE. Komarova, A.I. Khavkin. Constipation in young children: causes and features of dietary correction // Issues of modern pediatrics, 2014, No. 13 (1), p. 114-118.
- M.I. Dubrovskaya, P.V. Parshina. Current issues in the development of constipation in children, approaches to therapy // Issues of modern pediatrics, 2012, vol. 11, no. 11, pp. 76-82.
Vostrikova Ekaterina Borisovna Clinic
Author of the article
Vostrikova Ekaterina Borisovna
Specialty: gastroenterologist
Experience: 14 years
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
Physical activity for frequent constipation
One of the key values in the prevention and treatment of chronic constipation is physical activity. Loads commensurate with age and health status stimulate improvement of intestinal peristaltic activity.
For example, taking a deep breath stimulates improvement of trophism. Trained muscles of the anterior abdominal wall create optimal pressure for the normal functioning of the lower gastrointestinal tract.
Exercise helps improve a person’s quality of life and relieve chronic constipation. Sometimes regular walking for up to one hour is enough to improve bowel function.
Particularly useful in this regard are gymnastics, water aerobics, swimming, and cycling. Therapeutic exercises are the main method of treating spastic and atonic constipation; it improves the tone of the intestinal muscles. Light fitness, yoga, jogging can also be an option to keep fit.
If there are contraindications to exercise, you should consult your doctor and jointly choose the appropriate types of exercise.
What to do if a child has constipation - treatment methods for children of all ages
How to treat a child depends on the severity and type of problem. These could be medications, enemas, massage, diet.
It is not recommended to do enemas frequently, otherwise flaccid bowel syndrome may develop. That is, he will “forget how” to work independently. However, sometimes enemas are useful. Their volumes vary by age:
- up to 1 month – 30 ml;
- 1-3 months – 30-40 ml;
- 3-6 months – 90 ml;
- 6-12 months – up to 180 ml.
The temperature of the water in the enema should be around 23-24℃.
Massage helps well with atonic constipation. You need to massage the anterior abdominal wall in a clockwise circular motion. It is useful to place a small child on his stomach and gently irritate the anus with your hand.
To improve peristalsis, you can give a glass of juice or water.
For psychogenic constipation, you need to follow a number of recommendations:
- give more vegetables and liquids;
- do not focus on the problem, support the child;
- play role-playing games, behave positively, do not show frustration;
- do not scold the child, tell him how his body works, help him understand the problem;
- tell thematic tales, you can invent them yourself.
What can you give your child for constipation? Overview of drug groups
For spastic constipation, suppositories with glycerin can help. The introduction of other substances, including oils, is not recommended.
For constipation, several groups of laxatives are indicated:
- osmotic - transfer liquid to the stool to soften it, safe for children, they can be taken every day and for a long time - magnesium hydroxide, polyethylene glycol, lactulose, magnesium citrate, sorbitol;
- stimulants - promote contraction of the intestinal muscles, move stool through it, they are prescribed for a single dose - bisacodyl, senna;
- lubricants - facilitate the process of stool movement through the intestines, have an oil base - glycerin suppositories, petroleum jelly.
Diet
Nutrition should be correct, with plenty of liquid and plant fiber - vegetables, fruits, oatmeal, pearl barley, etc. You need to give up foods that slow down motor skills, control the caloric intake of the diet, the content of minerals and vitamins in it. The following products are excluded from the menu, and if the child is breastfed, they are excluded by the nursing mother:
- milk;
- strong tea, coffee;
- semolina;
- fatty food;
- baking;
- pasta;
- White bread;
- crackers;
- rice.
It is important to increase fiber in the diet, which will regulate bowel movements. It is abundant in fruits, vegetables, legumes, whole grains, seeds and nuts. The listed products are rich in minerals and vitamins and contain a lot of protein. The fiber content should be 2 g per serving. Recommended standards by age:
- 1-3 years – 19 g per day;
- 4-8 years – 25 g per day;
- 9-13 years - 31 g per day for boys, 26 g per day for girls.
Foods high in fiber
| Product | Fiber content |
| White beans | 9.5 g per ½ cup |
| Cereals | 8.8 g per ½ cup |
| Red beans | 8.2 g per ½ cup |
| Legumes | 7.5 g per ½ cup |
| Pear with peel | 4.3 g per small fruit |
| Raspberries | 4 g per ½ cup |
| Country style potatoes | 3.8 g per 1 piece. |
| Almond | 3.3 g per 30 g |
| Apple with peel | 3.3 g per 1 piece. |
| Banana | 3.1 g per 1 piece. |
| Orange | 3.1 g per 1 piece. |
| Broccoli | 2.8 g per ½ cup |
| Green pea | 2.5 g per ½ cup |
| Corn | 1.6 g per ½ cup |
| Strawberry | 1.5 g per ½ cup |
| Wild rice | 1.5 g per ½ cup |
| Raisin | 1.4 g per ½ cup |
Changing mode
The child needs to be taught to have bowel movements at the same time every day. To stimulate bowel movements, you can give cold water or fruit juice.
Regular physical activity is necessary to improve the functioning of the abdominal muscles. This could be regular walks, ball games, jumping rope, swimming, cycling.
The connection between intestinal microflora and constipation
The consequences of chronic constipation may be disturbances in the balance of intestinal microflora, but there is also an inverse relationship: dysbiosis leads to the development of prolonged constipation. In both cases, the intestinal microbiome should be restored and, at the same time, stool retention should be corrected.
For this purpose, both prebiotics and combination preparations containing them can be used. This is especially true for cases when dysbiosis develops against the background of antibacterial therapy.





![Table 1. Comparison of the results of treatment with Tribestan for men with oligoasthenozoospermia [7] with mod.](https://laram-halal.ru/wp-content/uploads/tablica-1-sravnenie-rezultatov-lecheniya-tribestanom-muzhchin-s-oligoastenozoospermiej-7-330x140.jpg)