How does a cream differ from an ointment, and an ointment from a gel?
The difference between cream, gel, balm and ointment is as follows:
- Cream is a dosage form based on oil and water. Creamy substances are easily absorbed, but are not able to penetrate deep into the tissue. They can be applied to surfaces that are constantly wet. In most cases, they are completely absorbed and do not stain clothes. You can rub the cream in and go about your business.
- The gel does not contain fats and oils, its acid-base indicators are close to those of the skin. It spreads easily over the skin, is quickly absorbed, and does not clog pores. Sometimes, after it dries, an airtight film remains (for example, Diclofenac). The structure of gel-like preparations can be liquid (for example, Troxevasin) or viscous. When stored in the refrigerator, they partially thicken, but when heated to room temperature, they restore their properties. Like creams, gels are convenient to use during the day.
- Ointment is a dosage form based on fats. It is absorbed more slowly than gel-like and creamy preparations, but it lasts longer. Penetrates deeply. It is applied to dry surfaces, scars, seals. Lubricated areas can be covered with bandages. The remaining fatty base usually has to be removed manually, so you need to apply ointment-like substances under clothing carefully. Some of them have a specific smell (for example, Vishnevsky ointment). The thickest ointments are called pastes. They contain up to 20% powdery substances. Most often they have drying properties.
- Balm is a medicinal or cosmetic product that contains no water at all. When you need to clarify what the difference is between a balm and a cream, this difference is given first. The absence of water allows balms to retain their properties for a long time. This is due to the fact that harmful bacteria multiply in water, and there is no natural habitat for them here.
Which is better, gel or cream, depends on the patient’s age and the condition of his skin.
The main difference between cream and ointment is the percentage of fat content. Something in between these substances in texture is called liniment. This dosage form contains fats and oils. If there is more fat, then the liniment resembles an ointment, if there is oil, it resembles a cream (for example, Synthomycin liniment). At body temperature, liniments begin to melt, so they are applied a little at a time so that excess medicine does not drip onto clothes and the floor.
Ketonal gel for external use 2.5% 100g
Compound
Active substance: ketoprofen 25 mg. Excipients: (carbomer - 20 mg, trolamine (triethanolamine) - 37 mg, ethanol 96% - 285 mg, lavender oil (lavender essential oil) - 0.28 mg, water - 632.72 mg) - 1 g.
Pharmacokinetics
Ketoprofen is absorbed very slowly and practically does not accumulate in the body. Bioavailability is 5%. Ketoprofen penetrates into the subcutaneous tissue, ligaments and muscles, synovial fluid and reaches therapeutic concentrations there. The concentration of the drug in the blood plasma is extremely low. Ketoprofen is metabolized in the liver to form conjugates, which are mainly excreted in the urine. Ketoprofen is characterized by slow excretion in urine.
Indications for use
Symptomatic treatment of painful and inflammatory processes of various origins, including:
- rheumatoid arthritis and periarthritis;
- ankylosing spondylitis (Bechterew's disease), psoriatic arthritis, reactive arthritis (Reiter's syndrome);
- osteoarthritis of various localizations;
- tendonitis, bursitis, myalgia, neuralgia, radiculitis;
- injuries of the musculoskeletal system (including sports), bruises of muscles and ligaments;
- sprains, ruptures of ligaments and muscle tendons.
Contraindications
- Hypersensitivity to ketoprofen;
- hypersensitivity to salicylates, tiaprofenic acid or other NSAIDs, fenofibrate, UV blockers, fragrances;
- violation of the integrity of the skin (eczema, weeping dermatitis, open or infected wound);
- indications in the anamnesis of attacks of bronchial asthma caused by taking NSAIDs and salicylates;
- history of photosensitivity reactions;
- exposure to sunlight, incl. indirect sunlight and UV irradiation in a solarium throughout the entire treatment period and for another 2 weeks after stopping treatment;
- III trimester of pregnancy;
- children under 15 years of age.
Carefully
Impaired liver and/or kidney function, erosive and ulcerative lesions of the gastrointestinal tract, blood diseases, bronchial asthma, chronic heart failure.
Directions for use and doses
Apply externally 2-3 times/day. The duration of treatment without consulting a doctor should not exceed 14 days.
Storage conditions
At a temperature not higher than 25 °C. Keep out of the reach of children.
Best before date
3 years. Do not use the drug after the expiration date indicated on the package.
special instructions
It is necessary to avoid contact of this product with the eyes, the skin around the eyes, and mucous membranes.
Ketoprofen can be used externally in combination with oral administration. The total daily dose, regardless of the dosage form, should not exceed 200 mg.
To reduce the risk of developing photosensitivity, it is recommended to protect skin areas treated with ketoprofen with clothing from exposure to ultraviolet radiation throughout the entire treatment period and for another 2 weeks after stopping use of the gel.
Do not use as occlusive dressings.
Description
NSAIDs.
Use in children
Contraindication: children under 15 years of age.
Pharmacodynamics
NSAIDs. It has analgesic, anti-inflammatory and anti-edema effects. Inhibits the activity of COX, which leads to inhibition of prostaglandin synthesis. In addition, ketoprofen inhibits lipoxygenase, bradykinin synthesis, stabilizes lysosomal membranes and prevents the release of enzymes involved in the inflammatory process.
Ketoprofen does not have a negative effect on the condition of articular cartilage.
Side effects
Allergic reactions: very rarely - angioedema, anaphylaxis.
From the skin and subcutaneous fat: infrequently - erythema, itching, burning, eczema, mild transient dermatitis; rarely - urticaria, rash, photosensitivity, bullous dermatitis, purpura, erythema multiforme, lichenoid dermatitis, skin necrosis, Stevens-Johnson syndrome; very rarely - a single case of severe contact dermatitis (due to poor hygiene and insolation), a single case of severe generalized photodermatitis, toxic epidermal necrolysis.
From the respiratory system: very rarely - asthmatic attacks (as a variant of an allergic reaction).
From the urinary system: very rarely - deterioration of renal function in patients with chronic renal failure.
Use during pregnancy and breastfeeding
Ketonal gel is contraindicated in the third trimester of pregnancy.
Ketonal gel can be used in the first and second trimesters of pregnancy after consultation with a doctor, if the expected benefit to the mother outweighs the possible risk to the fetus.
The use of Ketonal gel during breastfeeding is not recommended.
Interaction
Since the concentration of ketoprofen in the blood plasma is extremely low, symptoms of interaction with other drugs (similar symptoms with systemic use) are possible only with frequent and prolonged use.
The simultaneous use of other topical products containing ketoprofen or other NSAIDs is not recommended.
Simultaneous administration of acetylsalicylic acid reduces the degree of binding of ketoprofen to plasma proteins.
Ketoprofen reduces the excretion of methotrexate and increases its toxicity.
Patients taking coumarin-containing anticoagulant drugs are advised to undergo treatment under medical supervision.
Overdose
Overdose is unlikely when the drug is used externally.
In case of overdose, the skin should be thoroughly rinsed under running water.
If the drug is ingested, systemic adverse reactions may develop. In this case, symptomatic treatment and supportive therapy are necessary, as in case of overdose with oral forms.
Impact on the ability to drive vehicles and operate machinery
There is no data on the negative impact of the drug Ketonal gel on the ability to drive vehicles and engage in other potentially hazardous activities that require concentration and speed of psychomotor reactions.
Is it possible to replace cream-type medications with ointment-type ones and vice versa?
What is better, ointment or cream, is decided by the doctor in each specific case. When it is not possible to obtain the required dosage form, the ointment can be replaced with cream. Replacement is possible in cases where the dosage of the active substance in the creamy medicine is the same or less than in the ointment. If the dosage is less, the cream will need to be applied more often (the number of additional procedures must be calculated in advance).
You cannot use ointment instead of cream. It is absorbed much deeper, so it can affect the “wrong” areas (for example, with a strong inflammatory process).
When replacing ointment with cream, pay attention to the concentration of the active substance.
Do not use different dosage forms at the same time. When mixed, their components may not provide the same effect as desired. If your treatment plan includes different medications and you are deciding whether to apply an ointment or a gel first, start with the gel-like substance. When it is completely absorbed and its expiration date has passed (usually 2-4 hours), clean the treated surface from the film as much as possible, then lubricate it with ointment. This is also true for creams that should be used before ointments.
Ketonal gel 25mg/g 50g No.1
Name
Ketonal gel.
Release forms
Gel.
INN
Ketoprofen.
Description
Homogeneous, transparent gel.
Compound
1 g of gel for external use contains 25 mg of ketoprofen. Excipients: carbomer, trolamine (triethanolamine), ethanol (96%), lavender essential oil, purified water.
Pharmacotherapeutic group
Non-steroidal anti-inflammatory drugs ATC code: M01AE03.
Pharmacological properties
Pharmacodynamic properties
Ketoprofen is one of the most powerful inhibitors of the cyclooxygenase enzyme. It also inhibits lipoxygenase activity and bradykinin synthesis. By stabilizing lysosomal membranes, ketoprofen prevents the release of enzymes that are involved in the inflammatory process. Ketoprofen has similar pharmacodynamic properties and effects to non-steroidal anti-inflammatory drugs. It has analgesic, anti-inflammatory and antipyretic effects. The effects of ketoprofen have been established in animal experiments and in many clinical studies in humans.
Pharmacokinetic properties
Plasma and tissue levels of ketoprofen were studied in 24 patients after knee surgery. After repeated application of the gel to the skin, its plasma level was 60 times lower (9-39 ng/g) than that after a single oral dose of ketoprofen (490-3300 ng/g). Tissue levels of ketoprofen in the area of application were in a similar range of concentrations for the gel and oral forms, although there was significantly greater inter-patient variability with the gel. When administered topically, the bioavailability of ketoprofen was estimated to be about 5% of the level observed after oral administration, based on urinary excretion. Plasma protein binding is 99%. Ketoprofen is excreted by the kidneys, mainly in the form of glucuronides.
Indications for use
Ketonal is a non-steroidal anti-inflammatory drug. It has analgesic and anti-inflammatory effects. Ketonal is used: - to relieve acute painful conditions caused by injuries, such as sports injuries, damage to ligaments and tendons, bruises; - for pain due to mild arthritis.
Directions for use and doses
Adult patients: Apply the gel to the painful or inflamed area 2-4 times a day, gently rubbing into the skin. The dose depends on the area of the diseased area. Duration of treatment is up to 7 days. 5 cm of gel corresponds to 100 mg of ketoprofen, 10 cm of gel corresponds to 200 mg of ketoprofen. Contact with eyes or mucous membranes should be avoided. After each application of the gel, you should wash your hands thoroughly. Wearing tight clothing during treatment is not recommended. Ketonal gel can be used in combination with other dosage forms of Ketonal (capsules, tablets, suppositories). The total maximum daily dose, regardless of the dosage form, should not exceed 200 mg of ketoprofen. Elderly Patients: There are no specific dosage recommendations for the elderly. For those most prone to adverse reactions, the lowest dose should be combined with adequate clinical safety monitoring. Children: Not recommended as safety in children has not been established.
Contraindications
The use of Ketonal gel is contraindicated: - in patients with hypersensitivity to ketoprofen or any other component of the drug; - patients with known hypersensitivity reactions (eg, bronchospasm, rhinitis, urticaria) to ketoprofen, other non-steroidal antirheumatic drugs, salicylates (eg, acetylsalicylic acid), fenofibrate and tiaprofenic acid; - on skin damaged and changed by a pathological process, for example, eczema, acne, various dermatoses, open wounds or infectious lesions; - during the last trimester of pregnancy; - patients with a history of photosensitivity reactions; - patients with a history of allergic reactions to ketoprofen, fenofibrate, tiaprofenic acid, UV blockers or fragrances; - exposure of the area where the gel is applied to sunlight (including in cloudy weather), as well as UV radiation (solarium) throughout the entire treatment period and for 2 weeks after stopping the use of the drug. Children: Not recommended as safety in children has not been established.
Precautionary measures
Adverse effects can be reduced by administering the lowest effective dose for the shortest period of time needed to control symptoms. Although systemic adverse reactions from topical use of ketoprofen should be rare, the gel should be used with caution in patients with renal, cardiac or hepatic insufficiency, a history of gastric or duodenal ulcers or inflammatory diseases of the colon, cerebrovascular bleeding or bleeding diathesis. Ketonal gel should not be applied to the mucous membranes, anal area, genitals and around the eyes. Avoid getting the gel in your eyes. You should not wear tight clothing during treatment. Do not apply the gel under occlusive dressings. When the first signs of a skin reaction appear, the application of ketoprofen should be stopped immediately. Topical use of ketoprofen may provoke asthma in susceptible individuals. Large amounts of topically applied gel may cause systemic effects including hypersensitivity and asthma. Areas of skin to which Ketonal gel has been applied should be protected with clothing during treatment and for 2 weeks after completion to avoid exposure to ultraviolet radiation and the risk of photosensitivity.
Interaction with other drugs
Although interactions with other drugs are unlikely because ketoprofen blood concentrations are low after topical administration, caution should be exercised in patients taking methotrexate. Serious interactions have been described following the use of high doses of methotrexate and NSAIDs, including ketoprofen, when administered orally or parenterally. It is advisable to monitor patients receiving treatment with coumarins.
Pregnancy and lactation
Pregnancy The safety of using ketoprofen during pregnancy has not been proven. During the first two trimesters of pregnancy, ketoprofen should be discontinued unless the expected benefit to the mother outweighs the possible risk to the fetus. Ketoprofen is contraindicated during the last trimester of pregnancy. The use of ketoprofen in the last third trimester can cause delay in labor, increased bleeding in the mother and newborn, and cause premature closure of the ductus arteriosus with the development of pulmonary hypertension in the newborn. Lactation Ketonal should not be used during breastfeeding, since the safety of using ketoprofen during lactation has not been proven.
Impact on the ability to drive vehicles and operate machinery
Not applicable.
Side effect
The most common adverse effects associated with topical use of ketoprofen are localized skin reactions, which may spread beyond the site of application. Classification of adverse effects according to MedDRA by organs and systems and frequency of occurrence: Very common (≥1/10); Frequent (≥1/100,
Overdose
Given the low blood levels of ketoprofen when administered topically, no cases of overdose have yet been described.
Best before date
3 years. The medicine cannot be used after the expiration date indicated on the packaging.
Storage conditions
Store at a temperature not exceeding 25°C. Keep the tube tightly closed. Keep out of the reach of children.
Package Contents
50 g of gel in an aluminum tube. 1 tube with package insert in a cardboard box.
Vacation conditions
By doctor's prescription.
Manufacturer
Salutas Pharma GmbH, Osterwedingen, Germany
Buy Ketonal gel 25mg/g 50g No. 1 in the pharmacy
Price for Ketonal gel 25mg/g 50g No. 1
Instructions for use for Ketonal gel 25mg/g 50g No. 1
Gel and ointment - difference in shelf life
Expiration dates are usually given for sealed medications. As a rule, manufacturers write how long a substance can be stored unopened. In general, ointment-based preparations last longer than gel-based preparations because the fats they contain prevent drying out.
Store medications as recommended by the manufacturer.
When storing ointment, pay attention to the manufacturer's recommendations. In the refrigerator, the medicine can harden, and at a crucial moment you simply cannot get it out of the tube.
Gel-like preparations are more convenient to use than ointment-like preparations with a similar effect, and therefore cost a little more.
Gel or ointment – which is better in emergency situations?
The gel is absorbed much faster than ointment. Therefore, in a situation where you urgently need to relieve pain, for example, a joint, it acts faster. If you need to provide a longer analgesic effect, relieve inflammation, ointment is preferable.
In addition to the duration of action, the list of ways in which an ointment differs from a gel includes the ability to adhere to the surfaces being treated. Gel-like medications adhere better to wet, wet surfaces, from which ointment-like medications simply slide off.
In general, ointment can penetrate deeper than gel. However, some gel preparations (for example, Traumeel) contain additives that ensure deep penetration of the main active ingredient. Then the difference between gel, cream and ointment is insignificant.
Gels and creams act faster, ointments last longer.
What is the difference between nonsteroidal anti-inflammatory ointments, creams, and gels?
Home / About the problem / What is the difference between non-steroidal anti-inflammatory ointments, creams, gels
Where does it hurt?
Inflammatory diseases of the musculoskeletal system, for example, arthritis, myositis, osteochondrosis, as well as injuries, including sports and household injuries, such as sprains or bruises, are often accompanied by severe pain and swelling. Therefore, complex therapy usually includes external non-steroidal anti-inflammatory drugs in different release forms. Such drugs help relieve pain, and also help relieve swelling and erythema by suppressing the formation of prostaglandins - substances that contribute to the development of the inflammatory process1. Usually these are gels, ointments and creams, which differ from each other not only in the active substance, but also in the composition of the auxiliary components and the consistency of the base. Their use allows for maximum concentration of the drug in the area of application2.
To make ointments, chemically neutral, soft, fatty and dense substances that do not penetrate the skin well are used as a base. Creams have an emulsion base, lighter in consistency than ointment. Thanks to this, they leave only a slight fatty trace on the skin. Gels are gelatinous dosage forms produced on hydrophilic, that is, aqueous, bases3.
To determine which ointment or gel is better suited for use in a particular case, it is necessary to take into account the specifics of the damage. For example, ointments are used for chronic processes or when there is dryness, scales or crusts on the affected area. The fatty base of the ointment softens the stratum corneum, increasing its permeability to the active substance4. However, they are difficult to apply daily, as they leave a greasy and sticky residue on the surface that does not dry out.
Aertal® cream is a non-steroidal anti-inflammatory drug based on aceclofenac, which has anti-inflammatory and analgesic effects. The concentration of the active substance in it is 1.5%, while it is in the cream in micronized form. The base of Aertal® cream includes emulsion wax and liquid paraffin, as well as some other excipients.
Emulsion wax and liquid paraffin, which form the basis of Airtal® cream, are substances widely used in the pharmaceutical and cosmetic industries. They improve the consistency of the cream and facilitate uniform absorption of the active substance. At the same time, emulsion wax moisturizes and nourishes the skin, but does not leave a greasy mark on it5. This property allows you to use anti-inflammatory creams based on it daily. In addition, the cream, unlike the gel, allows you to retain the active substance in the painful area for a longer time.
When using Aertal® cream, aceclofenac practically does not enter the systemic circulation, and therefore the risk of systemic side effects, including on the gastrointestinal tract, is minimized6.
Airtal® cream should be applied to the painful area three times a day, using gentle massage movements. The application dose is determined by the size of the affected area, and it should be taken into account that 1.5–2 g of cream corresponds to a strip of 5–7 cm.
1 Kukes V.G. Clinical pharmacology. 2006. pp. 534–543.
2 Gavrilov A. S. Pharmaceutical technology. Manufacturing of medicines: textbook / A. S. Gavrilov. M.: GEOTAR - Media, 2010.
3 Krasnyuk I.I.. Pharmaceutical technology: Technology of dosage forms: Textbook for students. avg. prof. schools, institutions. - M.: “Academy”, 2004.
4 Dermatovenereology: textbook for medical universities / A. V. Samtsov, V. V. Barbinov.-SPb. : SpetsLit, 2008.
5 Kunder E. V. Analgesic therapy of inflammatory and degenerative joint diseases // International reviews: clinical practice and health. 2015. No. 1 (13). Ss. 56–63.
6 AIRTAL® (AIRTAL®) instructions for use.
About the cream
Airtal® cream has anti-inflammatory, analgesic and anti-edematous effects.
Injuries
Country injuries: protective measures and first aid
Chronic pain
Back pain: causes and treatment
Gel or cream – which is better to use for cosmetic purposes?
Cosmetics for hands, face and body are also made in the form of gels and creams.
- Cosmetic gel consists of 75−85% water. The remaining 15−25% are microparticles with the ability to retain moisture and other special properties. The high water content allows gel-like products to be easily absorbed into the skin, perfectly moisturize it, and avoid the formation of an unpleasant greasy film. They are recommended for young, combination, oily and problematic skin.
- Creams contain much less water than gel products. But they contain a lot of oils that provide different effects: nutrition, whitening, smoothing out fine wrinkles, etc. Creamy products are suitable for mature, dry and combination skin. They often leave an oily sheen and may not be completely absorbed. It is dangerous to apply them to problem skin - fats can clog pores and provoke even greater inflammation.
Problem skin loves gel, while normal skin loves cream.
The main difference between gel and ointment and cream is the time of use: gel-like substances are best used in the morning and afternoon, and cream-like substances are best used before bed. There are day creams, which are similar in structure to a gel, and night creams, which are more like an ointment.
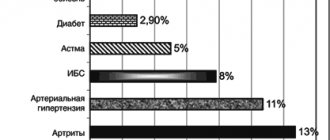
Ketonal cream in the treatment of lesions of various structures of the musculoskeletal system
1. A variety of causes leading to clinical symptoms (trauma, cartilage degeneration, inflammation, infection, congenital dysplasia, osteoporosis, etc.) [1]. 2. Various genesis of pain syndrome (inflammatory, mechanical, vascular, neural, etc.) [2]. 3. An increase in the frequency of pain in the musculoskeletal system with age, that is, in patients who often have concomitant pathologies and require complex drug treatment of comorbid conditions [3]. 4. The chronic nature of most diseases of the musculoskeletal system, which requires the use of not only effective, but also safe methods of treatment. According to the main pathogenetic mechanism, inflammatory lesions of the joints and periarticular tissues (arthritis, tenosynovitis, myositis), degenerative lesions of the joints of both the synovial type and intervertebral joints (osteoarthrosis, spondyloarthrosis), pathology of the intervertebral discs (osteochondrosis), traumatic lesions (post-traumatic arthritis, sprains) are distinguished. and ligament ruptures, etc.). Various nonsteroidal anti-inflammatory drugs (NSAIDs) are widely used to treat these conditions. These drugs, usually prescribed in tablet or capsule form, have proven to be highly effective, having, in addition to antipyretic, a distinct analgesic and anti-inflammatory effect. However, the use of NSAIDs also has negative sides. Most of them have undesirable effects on the gastrointestinal tract (dyspepsia, erosion, ulcers, which may be complicated by bleeding), kidneys (reduced sodium excretion, negative effects on long-term use on the interstitium of the kidneys), microcirculation and platelet aggregation, bronchi (bronchospasm) [4,5,6]. In addition, there is information that the frequency of adverse reactions from the gastrointestinal tract (ulcers of the gastric and duodenal mucosa, bleeding) while taking NSAIDs is higher in patients with damage to the musculoskeletal system than in patients suffering from other types of chronic pain [7]. These adverse reactions of many non-selective NSAIDs are associated with the main mechanism of their action - suppression of the synthesis of both isoforms of cyclooxygenase (COX) in the arachidonic acid cascade [8], responsible for the synthesis of both pro-inflammatory (COX-2) and physiologically significant (COX-1) prostaglandins . In recent years, drugs have appeared with a predominant suppression of COX-2 (meloxicam, nimesulide, nabumetone), which to a much lesser extent suppress the expression of COX-1 and, accordingly, the synthesis of prostaglandins involved in the physiological functions of the body. New generation drugs are specific COX-2 inhibitors (celecoxib, rofecoxib), which allow adequate treatment of patients with risk factors for side effects (ulcer history, old age). However, selective drugs are inferior to non-selective COX inhibitors in the severity of the analgesic effect, in addition, recent data dictate the careful use of systemically used NSAIDs in individuals with cardiovascular diseases or the risk of developing acute cardiovascular accidents (myocardial infarction, stroke) [9]. Local therapy for lesions of the musculoskeletal system is a very effective additional treatment method, and in some cases has distinct advantages over the use of oral forms of NSAIDs. Currently, the pharmacy chain has a fairly large number of different ointments, gels, and creams that are used to relieve pain in joints, muscles, and ligamentous-tendon structures. These products are created on the basis of NSAIDs, have different concentrations of the active substance, and often contain other medicinal substances, some of which are contraindicated for the treatment of inflammation (irritating and distracting components). When choosing a local therapy, the doctor must take into account which active ingredient is included in the base of the cream or ointment, and choose products that have advantages over other NSAIDs. In addition, it should be noted that doctors rarely pay attention to the concentration of the active substance in the local therapy (Table 1). Ketonal cream has a high concentration (5%) of the active substance - ketoprofen, a derivative of propionic acid. It is propionic acid derivatives (ibuprofen, flurbiprofen, ketoprofen) that have established themselves as the safest non-selective NSAIDs [10]. As data from domestic and foreign authors have shown, Ketonal is distinguished from other NSAIDs by the most pronounced analgesic effect [11]. In its analgesic and anti-inflammatory activity, Ketonal is superior to diclofenac in both tablet and parenteral form [12]. Ketonal's tolerability, shown by both domestic [13,14] and foreign authors [15], is also unusually good for drugs that non-selectively suppress the activity of cyclooxygenase (COX). The effectiveness of local therapy depends on the ability of the drug to overcome the skin barrier and on the choice of the daily dose of the drug. When using NSAIDs in tablet form, the doctor, as a rule, is well versed in the range of daily doses of the drug, and when using local therapy, he does not always focus the patient’s attention on the dosage of the ointment or cream. As with any therapeutic agent, it is necessary to prescribe an optimal therapeutic dose that provides an analgesic and anti-inflammatory effect. The low concentration of the active substance and incomplete passage of the drug directly to the site of inflammation (Fig. 1) dictate the need for repeated application of ointment or gel to the affected area during the day. Data from many clinical trials have shown that the minimum is 4 times the application of a local product per day, and with active inflammation, the frequency of application of the drug can increase to 5-6 times a day. The amount of the drug applied depends on the size of the joint: a strip of ointment or gel 5 to 10 cm long should be applied to the area of large joints (knee, shoulder), and a strip of ointment or gel 5 to 10 cm long should be applied to the area of medium-sized joints (ankle, wrist, elbow) - from 3 to 5 cm and in the area of small joints of the hands and feet – 1–2 cm [5-8]. It is necessary to take into account the condition of the skin in the area of application of the local therapy product. Thus, in elderly people, the absorption of the drug into the skin decreases, which serves as an indication to increase the amount of cream applied or to increase the frequency of application of the drug. The passage of the skin barrier largely depends on the base of the anti-inflammatory ointment, cream or gel. The gel form is certainly convenient for use (more hygienic). It is believed that local therapy products in the form of a gel penetrate the skin more easily and quickly. A very interesting study by Gurol Z. et al. [18], who assessed the amount of ketoprofen released, its percutaneous absorption, and the anti-inflammatory effect of topically applied ketoprofen in experimental arthritis in mice depending on the drug base used. A comparison was made between a gel (water soluble) base and a hydrophobic ointment as a water insoluble base. The severity of the suppression of the inflammatory process largely depends on the amount of anti-inflammatory agent that can be released from the base on which it is created. The amount of ketoprofen released in vitro was higher from the gel base at concentrations of the substance from 1.3 to 5%, and at ketoprofen concentrations of 5% and higher, it was released in greater quantities when using the ointment base (p < 0.05). As shown in Figure 2, when using a fat base, the proportion of released ketoprofen was in direct proportion to its concentration in the ointment (from 1 to 10%), and the amount of ketoprofen released from the gel increased only with an increase in its concentration from 1 to 3%, and a further increase no release of the active substance occurred. When analyzing the degree of release of the active substance from the gel and ointment bases in vivo, it did not differ at any concentration of ketoprofen. The authors note that the degree of release of ketoprofen from the base correlated well with a decrease in experimental inflammation and that a 3% concentration of ketoprofen in the ointment or gel was sufficient to achieve an anti-inflammatory effect. But at the same time, suppression of carrageenan edema (experimental arthritis) when using the ointment was noted by 69%, and when using the gel - by 1.43%, which is explained by the effect of interaction of the gel base with sodium sulfates of the skin [19]. Based on the ability to pass the human skin barrier, two categories of drugs are distinguished: for lipophilic substances, the permeability coefficient through the skin correlates with the drug release coefficient, and for hydrophilic substances, the permeability coefficient is most often constant [20]. In addition, slower elimination of fat-based ketoprofen in the area of inflammation allows for a longer presence of the anti-inflammatory agent in the area of inflammation and, accordingly, a more pronounced anti-inflammatory effect. Similar data were obtained in another study [21]: when comparing the skin penetration of lipophilic NSAIDs (ibuprofen, flurbiprofen, ketoprofen) and hydrophilic NSAIDs (diclofenac, antipyrine), it was shown that the penetration of lipophilic drugs through human skin and the hairless skin of rats was higher than water-soluble drugs. The clinical conclusion from these studies may be the following: in terms of therapeutic effect, gel-based NSAIDs do not have any clear advantages over ointment or cream forms. In accordance with the pharmacokinetics of ketoprofen, the speed of its release from the fatty base and longer preservation in tissues allow the use of a less frequent application regimen than when using a gel (3-4 times a day) and in cases of severe inflammatory processes. We assessed the analgesic and anti-inflammatory effect of 5% Ketonal cream in patients with active rheumatoid arthritis (RA) admitted to the hospital due to the insufficient effect of anti-inflammatory therapy. A mandatory criterion for inclusion of a patient in such a study was severe arthritis of a large joint (knee in 14 patients and wrist in 1 patient) against the background of selected therapy with NSAIDs and basic drugs. The cream was applied to the joint 4 times a day in the amount of 5 cm strips (knee joint) or 3 cm strips (wrist joint). Before the start of therapy and after 2 weeks of treatment with Ketonal cream, the following parameters were assessed: 1) pain as assessed by the patient (pain score); 2) pain during palpation (according to the Ritchie method), severity of swelling in points (0 - no swelling, 1 - questionable swelling, 2 - obvious swelling and 3 - severe swelling); 3) joint volume (in cm); 4) limitation of movements in the joint in points (1 - violation of flexion or extension, 2 - violation of flexion and extension, 3 - minimal range of motion in the joint). The positive effect of Ketonal cream was noted in 100% of cases, which was expressed in a significant decrease in pain (both independent pain and pain during palpation), a significant decrease in the volume of the knee joints and an increase in the range of motion in the affected joint. None of the patients had any side effects of therapy (neither local nor systemic) [16]. When treating arthritis, inflammatory processes in periarticular tissues, and back pain, Ketonal cream is usually prescribed without combination with other drugs. When treating phlebitis of various etiologies (post-traumatic, due to varicose veins) and soft tissue bruises, you can combine the use of Ketonal cream with gels and ointments containing heparin. The combined use of anti-inflammatory creams and gels and heparin-containing drugs is also used in traumatology in the treatment of soft tissue bruises, the most common type of traumatic injury [17]. In addition to pain and swelling, hemorrhage is clinically significant with soft tissue contusions. Obstruction of venous outflow and impaired vascular permeability lead to disruption of microcirculation in the bruise area, which can cause the development of post-traumatic thrombophlebitis or exacerbation of the pathology of the venous system. Isolated use of heparin-containing drugs such as heparin sodium gel can lead to a significant reduction or disappearance of pain after 3–5 days in 48.4% of patients, and the combined use of heparin sodium gel and an anti-inflammatory local agent - in 71.9% of patients in the same period. deadlines. A similar effect has been demonstrated for edema in the area of injury [17]. An increase in the severity of the analgesic effect and its prolongation were also noted when treating the skin of patients before applying products containing heparin and NSAIDs with a semi-alcohol solution. This made it possible to reduce the frequency of drug application from 3 to 2 times a day in some patients, and in 11% of patients with mild pain, use the drug even once a day. Thus, Ketonal cream has a high (5%) concentration of a very active non-steroidal anti-inflammatory drug - ketoprofen, has pronounced analgesic and anti-inflammatory activity, is effective in patients with a high degree of joint inflammation when prescribed in optimal therapeutic doses in 100% of cases. The drug does not contain irritating substances, which is reflected in its good local tolerability. Literature 1. Nasonov E.L. Pain syndrome in pathology of the musculoskeletal system Vrach, 2002 4, pp. 15-19 2. Chichasova N.V. Pain syndrome in rheumatology breast cancer, 2002, volume 10, no. 6, 312-315 3. Ruoff G. Management of pain in patients with multiple health problems: a guide for the practicing physician. Amer. J. Med., 1998; 105(1B):53S-60S. 4. Chevat C., Pena BM, Al MJ et.al. Healthcare resource utilization and costs of treating NSAID-associated gastrointestinal toxicity: a multinational perspective. Lancet, 1991, 336: 810-815. 5. MacMahon S., Peto R., Culter J. et.al. Blood pressure, stroke, and coronary heart disease, part 1: prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet, 1990, 335: 765-774. 6. Breedveld F. “Pharmacological approaches to pain management in musculoskeletal diseases: choices and rational combination.” In: “Pain in musculo-skeletal diseases: New concepts for an age-old question”, Excerpta Medica Asia, Hong Kong, 1998, P. 7-9. 7. Janssen M., Dijkmans B., van der Sluijs FA “Upper gastrointestinal complaints and complications in chronic rheumatic patients in comparison with other chronic diseases” Br.J.Rheum., 1992., Vol.31: 747-752. 8. Brooks P., Emery P., Evans JF et. al. Interpreting the clinical significance of the differetial inhibition of cyclooxigenase-1 and cyclooxigenase-2. Rheumatology, 1999, 39: 779-788. 9. Mareev V.Yu. Is the cardiac safety of non-steroidal anti-inflammatory drugs real? Heart, 2003, volume 2, no. 4, 1-6 10. Scholes D., Stergachis A., Penna PM, Hansten PD Nonsteroidal anti-inflammatory drug discontinuation in patients with osteoarthritis. J.Rheum., 1995, V.22: 708-712 11. Nasonov E.L., Chichasova N.V. Ketoprofen: new prospects for use in rheumatology Ross. rheumatologists, 1999, No. 3b 8-14 12. Chichasova N.V., Imametdinova G.R., Igolkina E.V. Ketonal (ketoprofen) in the practice of a rheumatologist and therapist. RMJ, volume 11, 23 (195), 2003, pp. 1288-1290 13. Chichasova N.V., Imametdinova G.R., Karateev A.E. and others. Efficacy and safety of ketoprofen (ketonal) for rheumatoid arthritis (clinical endoscopic study). Scientific and practical rheumatologists, 2001; 1: 47-52. 14. Lazebnik L.B., Drozdov V.N., Kolomiets E.V. Comparative effectiveness and safety of the use of ketoprofen, lornoxicam, nimesulide and celecoxib in patients with osteoarthritis. RMJ, 2004, volume 12, no. 14, 844-847 15. Veys BM 20 years experience with ketoprofen. Scand.J.Rheum., 1993, Suppl.90: 1-44 16. Chichasova N.V., Nasonov E.L., Alekberova Z.S., Imametdinova G.R., Karateev D.E., Reshetnyak T. .M. Efficasy and tolerability of various ketoprophen forms (Lek, Slovenia) in short-term and long-term treatment of patients with active rheumatoid arthritis. Ann. Rheum. Dis., 1999, Abstract of XIV EULAR Congress, 201(835) 17. Silin L.L., Brovkin S.V. The use of gels in the complex treatment of closed soft tissue injuries. Medical assistance, No. 2. 2001, 11-13. 18. Z. Gurol, S., Hekimoglu, R., Demirdamar M. Percutaneous absorption of ketoprofen. In vitro release and percutaneous absorption of ketoprofen from different ointment bases Pharm. Acta Hel., 1996, V.71: 205-212 19. Froebe CL, Simion FA, Rhein LD et.al. Stratum corneum lipid removal by surfactants: relation to in vivo irritation Dermatology, 1990, V.181: 277-283 20. Walters KA Penetration enhancers and their use of transdermal therapeutic systems In Hadgraft J. and Guuy RH (Eds.), Transdermal Drug delivery , Marcel Dekker, Inc., New York. P.197 21. Morimoto Y., Hatanaka T., Sugibayashi K., Omiya H. Prediction of skin permeability of drugs: comparison of human and hairless rat skin J. Pharm. Pharmacol., 1992, V.8: 634-639