Side effects
Depo-Provera is valued for its absence of many side effects, which cannot be said, for example, about some hormonal pills. Due to the injections, the menstrual cycle may change slightly. This shouldn't be much of a concern. But still, if this condition is very worrying, it is better to go to the doctor. This is the only way to get rid of doubts and get recommendations about whether you can continue to use the chosen method of contraception.
But there are also situations in which going to the doctor is not advisable, but mandatory. This applies to cases where serious disruptions are observed during menstruation. For example, monthly bleeding disappears or does not occur in accordance with the usual schedule. A noticeable increase in your own weight, as well as the appearance of headaches and incomprehensible depression, should also alert you. With such symptoms, it may be necessary to stop the protective injections, but the main word remains with the specialist.
Depo-Provera
Progestogen-based contraceptive. Available in the form of a suspension for intramuscular administration (injections) and in the form of tablets. The most popular among doctors and patients is the suspension, which provides protection in a very comfortable way.
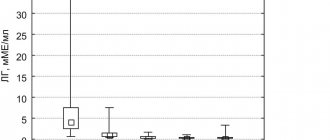
When administered by injection, the drug has a long-term contraceptive effect due to the fact that it suppresses the secretion of hormones produced by the pituitary gland, primarily luteinizing hormone. The consequence of this is the suppression of ovulation and the cessation of follicle maturation. In addition, Depo-Provera increases the viscosity of cervical mucus, which also contributes to the contraceptive effect.
When using Depo-Provera, the following manifestations of positive effects on the body are noted:
- reduction of vasomotor symptoms during menopause (fever, hot flashes, chills),
- reducing the risk of osteoporosis during menopause,
- reducing the risk of inflammatory diseases of the genital organs, vulvovaginal candidiasis,
- Most women with endometrial hyperplastic processes experience partial or complete regression,
- reducing the risk of endometriosis, breast, uterine and kidney cancer.
It is important that Depo-Provera does not affect lactation, and its concentration in breast milk is insignificant. Therefore, this means of contraception can be recommended for women during lactation.
Depo-Provera is prescribed by a gynecologist for contraception purposes, especially in women of late reproductive age (35+), as well as for:
- treatment of endometriosis,
- diagnosis of primary and secondary amenorrhea,
- therapy during menopause,
- treatment of premenstrual syndrome,
- prevention and treatment of osteoporosis during menopause,
- treatment of tumor formations in the area of the kidneys, breast, endometrium (including with metastases).
[[see_also_3]]
Contraindications to the use of Depo-Provera are:
- pregnancy,
- tumors of the genital organs or breast (in some cases),
- bleeding from the genital tract of unknown origin.
If you have a history of diseases such as thrombophlebitis, thromboembolism or stroke (including the risk of stroke), liver failure, hypercalcemia, epilepsy, migraine, bronchial asthma, heart or kidney failure, diabetes mellitus, frequent depression, be sure to tell us about it doctor. For such diseases, the doctor must take special care when prescribing contraception.
Side effects:
- headache, dizziness, causeless irritability, depression;
- insomnia or, conversely, drowsiness;
- increased fatigue;
- nausea, pain and discomfort in the abdomen;
- thromboembolic disorders;
- allergic reactions (urticaria, itching, rash);
- increased sensitivity of the nipples of the mammary glands;
- cervical erosion, dysmenorrhea, spotting;
- “vulgar” acne, hirsutism, changes in body weight;
- alopecia (hair loss).
Immediately after the injection, there may be pain, slight lumps for some time, and the color of the skin may change slightly. These manifestations are temporary.
Reception scheme
For contraceptive purposes, an intramuscular injection of 150 mg is given every three months. In order to exclude the possibility of pregnancy at the time of the first injection, it is recommended to do it within five days after the start of the next menstruation or before six weeks after childbirth.
For other purposes - for the treatment of dysfunctional uterine bleeding, endometriosis, cancer, osteoporosis - tablets are prescribed. The dosage regimen and dosage are determined by the doctor individually.
Other things to consider
When planning to resort to this method of contraception, it is important to remember the following points:
- It is prohibited to injure the injection site in any way. The area should not be rubbed, combed or massaged. It is better to spend the first hours after the injection relaxing, in a calm environment.
- You should not lose vigilance at the initial stage of using such contraception. In the next two weeks after the first administration of the drug, it is necessary to protect yourself by using an additional method of protection against pregnancy, for example a condom. It is contraindicated to take hormonal substances.
- If you miss the deadline for your next injection, you must make sure that you are not pregnant. Only if you are sure of this is it permissible to take a contraceptive injection again. After it, as at the very beginning of using the method, you need to use additional protection for two weeks.
- It should be borne in mind that the purpose of Depo-Provera is only to prevent conception, but such injections are not capable of protecting against dangerous sexually transmitted diseases. Therefore, if you are not confident in your partner, you should think about how to eliminate the risk of infection.
When planning to conceive a child, you must stop taking injections several months before.
Depo-provera®
Before prescribing Depo-Provera, the patient should be thoroughly examined.
If signs and/or symptoms of thromboembolism occur, the risk-benefit ratio should be assessed before continuing use of the drug.
If the Itsenko-Cushing symptom complex (moon face, fluid retention, decreased glucose tolerance, increased blood pressure) appears while taking the drug in high doses, the dose should be reduced if possible and the patient's condition should be carefully monitored.
Use of the drug in high doses may cause weight gain and fluid retention. Therefore, caution should be exercised when treating patients whose condition may be adversely affected by weight gain or fluid retention.
Patients with a history of treatment for depression should be carefully monitored. During therapy with Depo-Provera, some patients complain of depression similar to premenstrual depression.
When conducting a cytological or histological examination of the endometrium or cervix, it is necessary to notify the histologist about the therapy being carried out.
The drug should be used with caution in the postpartum period due to the increased risk of heavy and prolonged uterine bleeding.
It is believed that the use of Depo-Provera may increase the risk of developing osteoporosis.
You should stop using the drug if there is a sudden partial or complete loss of vision, or if you develop bulging eyes, double vision, or migraine attacks. If the examination reveals damage to the fiber vessels or swelling of the optic nerve nipple, Depo-Provera should also not be used.
If jaundice develops, you must stop using the drug.
The use of the drug may affect the results of the following laboratory tests: determination of gonadotropin levels (downward); determination of blood plasma levels of progesterone, cortisol, estrogens (towards a decrease); determination of the level of pregnanediol in urine (downward); determination of testosterone levels in blood plasma (towards a decrease); determination of the level of specific globulin that binds sex hormones (towards a decrease); performing a sugar load test (glucose tolerance test); metapyrone test; can change the results of the test for prothrombin (factor II) and blood clotting factors VII, VIII, IX, X (increasing); increases the value of liver function indicators.
Depo-Provera suspension for injection 500 mg/3.3 ml, 1 pc.
Mechanism of action.
Medroxyprogesterone acetate is a synthetic progestin that is structurally similar to the endogenous hormone progesterone. The following pharmacological effects on the endocrine system were observed:
- inhibition of the synthesis of pituitary gonadotropic hormones (FSH and LH)
- decrease in ACTH and hydrocortisone levels in the blood
- decreased levels of circulating testosterone;
- decrease in the level of circulating estrogen (due to inhibition of the synthesis of follicle-stimulating hormone and enzymatic induction of reductase in the liver, which leads to an increase in the clearance of testosterone and, as a consequence, to a decrease in the conversion of androgens to estrogens).
All this leads to a number of pharmacological effects described below.
Contraception.
Medroxyprogesterone acetate, when used parenterally by women at the recommended dose, inhibits the secretion of gonadotropic hormones, prevents follicle maturation and the onset of ovulation, and causes thickening of the cervical mucus, which prevents sperm from entering the uterus.
Gynecology.
Medroxyprogesterone acetate, when administered orally or parenterally in recommended doses by women with sufficient levels of endogenous estrogen, leads to the transformation of proliferative endometrium into secretory endometrium. Its androgenic and anabolic effects have been noted, but it is clear that this drug does not have significant estrogenic activity. When administered parenterally, medroxyprogesterone acetate suppresses the formation of gonadotropic hormones, prevents follicle maturation and the onset of ovulation. Current available evidence suggests that this does not occur with a single dose of the usual recommended oral daily dose.
Oncology.
Medroxyprogesterone acetate has antitumor activity. When used in high doses (orally or intramuscularly), medroxyprogesterone acetate is effective in the palliative treatment of hormone-dependent malignancies.
Clinical researches.
Study of bone mineral density.
Changes in bone mineral density in adult women.
In a non-randomized controlled clinical trial comparing adult women receiving Depo-Provera injections (150 mg intramuscular) for contraception for up to 5 years with women not using hormonal contraception, 42 participants , used Depo-Provera® injections, completed 5 years of treatment, and provided results of at least one bone mineral density measurement during the follow-up period after discontinuation of Depo-Provera®. In women who used Depo-Provera®, a decrease in bone mineral density was observed during the first two years of use; in subsequent years the decrease was insignificant. After 1, 2, 3, 4 and 5 years of use, the average changes in bone mineral density of the lumbar spine were -2.86%, -4.11%, -4.89%, -4.93% and -5, respectively. , 38%. The mean decrease in bone mineral density of the total hip and femoral neck was approximately the same. Women in the control group did not experience significant changes in bone mineral density over the same time period.
Restoration of bone mineral density after cessation of treatment in adult women.
In the same study, partial recovery of bone mineral density to baseline levels was observed over a 2-year period after completion of Depo-Provera® injections (150 mg intramuscular).
After 5 years of treatment with Depo-Provera® injections (150 mg intramuscular), compared with baseline, the average percentage change in bone mineral density of the spine, hip and femoral neck was -5.4%, -5.2% and -6.1% respectively. At that time, corresponding values in control women who did not receive treatment for the same period of time showed average deviations from baseline of +/- 0.5% or less in the same skeletal regions. Two years after discontinuation of Depo-Provera injections, mean bone mineral density values at the spine, hip, and femoral neck increased at all three skeletal sites, but deficiency persisted: -3.1%, -1.3%, and -5. 4% respectively. During the same period of time, women in the control group had the following mean changes in spine, hip, and femoral neck bone mineral density compared to baseline: 0.5%, 0.9%, and -0.1%, respectively.
Changes in bone mineral density in adolescent girls (12-18 years old).
The effects of Depo-Provera® (administered intramuscularly at a dose of 150 mg) on bone mineral density were assessed over 240 weeks (4.6 years) in an open-label, single-arm clinical trial involving 159 adolescent girls (aged 12-18 years) who were selected for treatment with Depo-Provera®; 114 of 159 participants used Depo-Provera® chronically (4 injections during each 60-week period) and bone mineral density measurements were taken at 60 weeks. Bone mineral density decreased during the first 2 years of use and with little change during subsequent years. After 60 weeks of use with Depo-Provera®, the mean percentage changes from baseline in spine, hip, and femoral neck bone mineral density were -2.5%, -2.8%, and -3.0%, respectively. A total of 73 participants continued Depo-Provera® for 120 weeks, with mean percentage changes from baseline in spine, hip, and femoral neck bone mineral density of -2.7%, -5.4%, and -5.3% respectively. A total of 28 participants continued Depo-Provera® for 240 weeks, with mean percentage changes from baseline in spine, hip, and femoral neck bone mineral density of -2.1%, -6.4%, and -5.4% respectively.
Restoration of bone mineral density after treatment cessation in adolescents.
In the same study, 98 adolescent participants received less than 1 injection of Depo-Provera® and provided at least one bone mineral density measurement during the follow-up period after stopping Depo-Provera® while being treated with Depo-Provera® during the period up to 240 weeks (equivalent to 20 injections of Depo-Provera®) and during the follow-up period after completion of treatment until 240 weeks after the last injection of Depo-Provera®. The median number of injections received during the treatment phase was 9. At the time of the last injection of Depo-Provera®, the percentage change in bone mineral density of the spine, hip and femoral neck compared to baseline was -2.7%, -4 .1% and -3.9% respectively. Over time, these average levels of insufficient bone mineral density were completely leveled out after discontinuation of Depo-Provera®. It took 1.2 years for the complete restoration of the lumbar spine, 4.6 years for the hip joint, and 4.6 years for the femoral neck. Long duration of treatment and smoking were associated with slower recovery (see section "Peculiarities of application").
Incidence of fractures in women using Depo-Provera® injection (150 mg intramuscularly) or without using the drug during reproductive age.
A retrospective cohort study of 312,395 women using contraception was conducted in the UK. The purpose of the study was to evaluate the association between Depo-Provera® injections and the incidence of fractures. The incidence of fractures was compared before and after initiation of Depo-Provera® and between women who used Depo-Provera® and those who used other methods of contraception in the absence of documented use of Depo-Provera®. Among women who used Depo-Provera®, use of the drug was not associated with an increased risk of fractures (incidence ratio = 1.01, 95% CI (confidence interval) 0.92-1.11, compared with the follow-up period before 2 years preceding the use of Depo-Provera®). However, women who used Depo-Provera® had more fractures compared with those who did not use this drug, as after the first use of this contraceptive (incident ratio = 1.23, 95% CI 1.16-1. 30) and before (case ratio = 1.28, 95% CI 1.07–1.53).
In addition, fractures of specific bone sites characteristic of osteoporotic fractures (spine, hip, pelvis) were not more common in women taking Depo-Provera® compared to those women not using the drug (incidence ratio = 0.95 , 95% CI 0.74-1.23), and there was no evidence that longer-term use of Depo-Provera® (for 2 years or longer) causes a higher risk of fractures compared with use over a period of less than 2 years.
Data show that women who use Depo-Provera® have distinctly different fracture risk profiles compared to women who do not use this drug for reasons unrelated to their use of Depo-Provera®.
The maximum follow-up period in this study was 15 years, so possible effects of Depo-Provera® that may extend beyond the 15 year follow-up period cannot be determined.
— Women's Health Initiative Study.
The Women's Health Initiative study of combined conjugated estrogens (0.625 mg)/medroxyprogesterone acetate (2.5 mg) to evaluate the risks and benefits of this combination therapy compared with placebo in preventing the development of certain chronic diseases was conducted in 16,608 women during the period postmenopausal women aged 50-79 years with an intact uterus at baseline. The primary endpoint was the incidence of coronary heart disease (non-fatal myocardial infarction and death attributable to coronary heart disease), and invasive breast cancer was considered the primary adverse outcome. The study was terminated early during follow-up, which averaged 5.2 years (planned duration 8.5 years), because the increased risk of breast cancer and cardiovascular events outweighed the reported benefit, based on prespecified study termination criteria. included in the “general indicator” (see section “Application Features”).
Combination therapy with conjugated estrogens/medroxyprogesterone acetate caused a significant reduction in the incidence of osteoporotic fractures (23%) and the overall incidence of fractures (24%).
- The Million Women Study.
The Million Women Study was a prospective cohort study conducted in the UK involving 1,084,110 women aged 50–64 years, of whom 828,923 were included in the main analysis of the risk of breast cancer associated with hormonal hormone replacement at some time after menopause. therapy. A total of 50% of the study population were using hormonal therapy at some point in time. Women who received hormone therapy at baseline used medications containing estrogen alone (41%) or a combination of estrogen and progestin (50%). The mean follow-up period was 2.6 years for the cancer incidence analysis and 4.1 years for the mortality analysis (see Section "Peculiarities of Application").
- Heart and Estrogen/progestin Replacement Studies
The Cardiac Estrogen/Progestin Replacement Therapy Study (HERS Study and HERS II) were 2 randomized, prospective secondary prevention trials that examined the long-term effects of oral continuous conjugated estrogens/medroxyprogesterone acetate combination therapy (0.625 mg conjugated estrogens and 2 5 mg medroxyprogesterone acetate). ) in women with coronary heart disease during the postmenopausal period (see section “Peculiarities of use”). This study included 2763 postmenopausal women with an intact uterus, with a mean age of 66.7 years. The mean follow-up period was 4.1 years for the HERS study and an additional 2.7 years (6.8 years total) for the HERS AI study (see Application Considerations).
- Women's Health Initiative Memory Study.
The Women's Health Initiative Memory Study, a subset of the Women's Health Initiative, included 4,532 predominantly healthy postmenopausal women aged 65 to 79 years and assessed the effects of conjugated estrogen therapy/medroxyprogesterone acetate (0.625 mg conjugated estrogen and 2.5 mg medroxyprogesterone acetate) or conjugated estrogens alone (0.625 mg) on the incidence of dementia compared with placebo. The average follow-up period was 4.05 years for the conjugated estrogens/medroxyprogesterone acetate group (see Section "Peculiarities of Use").