Lichen planus
Warts
7371 24 August
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Lichen planus: causes, symptoms, diagnosis and treatment methods.
Definition
Lichen planus is a chronic inflammatory disease of the skin and mucous membranes of unknown etiology. It is quite rare (according to WHO, 0.5% of all skin diseases) and, as a rule, occurs in people aged 45 to 60 years.
Causes of lichen planus
The causes of lichen planus still remain unclear. Experts classify it as a group of autoimmune diseases, when the body begins to produce antibodies that destroy its own tissues.
Provoking factors may include stressful situations, taking certain medications, possibly viral hepatitis C, or decreased immunity.
It has been noticed that patients with lichen planus are often characterized by increased excitability, suffer from insomnia and are prone to frequent mood swings. Some scientists believe that lichen planus is a delayed hypersensitivity reaction to various chemicals.
Proponents of the infectious nature of the disease talk about cases of the development of lichen planus after various injuries.
Classification of the disease
In patients with lichen planus, the following most common forms of skin lesions are distinguished:
- typical (the same type of rash in the form of papules),
- hypertrophic (warty rashes with indentations),
- bullous (blisters turning into plaques),
- actinic (large plaques, light at the edges and dark in the center),
- ring-shaped, or anular (rashes in the form of rings with raised edges),
- atrophic (nodules that rise above the skin and leave behind scars),
- pigmented (brown rashes merging into lesions),
- erosive-ulcerative (in addition to papules there are erosions and, less commonly, ulcers),
- follicular (pointed papules covered with dense horny scales).
Symptoms of lichen planus
In lichen planus, rashes appear on the skin, localized symmetrically on the flexor surfaces of the limbs, torso, as well as on the mucous membranes of the oral cavity, sometimes the esophagus, perineal area and anus; less often, nails, hair, palms, soles and face are affected.
Patients are bothered by itching, the severity of which depends on the form of the disease. The presence of papules on the oral mucosa causes discomfort; in the erosive-ulcerative form, bleeding of the gums is possible; there are complaints of dry mouth and pain when eating hot food. Ulcerative skin lesions in the erosive-ulcerative form are characterized by pain that intensifies during movement if they are located on the lower extremities.
In rare cases, the disease affects the nails. You can observe thinning of the nail plate, longitudinal grooves, splitting of the nail, discoloration of the nail plate and even its rejection from the nail bed.
Diagnosis of lichen planus
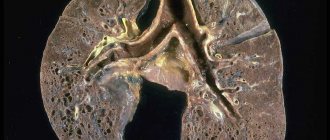
In most cases, the diagnosis of lichen planus is made based on the clinical picture. However, if patients have hypertrophic, atrophic, pigmentary, cystic, erosive-ulcerative and follicular forms, the typical elements inherent in this disease may be absent. To clarify the diagnosis, a biopsy of skin lesions is performed, followed by histological examination.
Before prescribing drug therapy, it is necessary to conduct laboratory tests, including a general (clinical) blood test, a general urinalysis, a biochemical blood test: AST, ALT, total bilirubin, triglycerides, cholesterol, total protein.
Damage to the oral mucosa in LLP
Topical and systemic corticosteroids
Topical corticosteroids are first-line drugs for the treatment of localized forms of LP of the oral mucosa. Strong and very strong drugs - clobetasol, triamcinolone, betamethasone, fluocytonide, fluticasone - have proven effectiveness and safety. These drugs are usually applied 2 times a day, either undiluted (eg clobetasol propionate 0.05%) or mixed with Orabase (eg triamcinolone) for 1-2 months, followed by maintenance use. It is also possible to use GCS in the form of intralesional injections, but there is insufficient data to support the advantage of this method over others (there are only isolated clinical cases). Systemic therapy using oral corticosteroids may be indicated in case of significant severity of the disease, in case of refractory to external therapy, however, the evidence base for this approach is insufficient; adequate placebo-controlled studies have not been conducted. Taking into account the wide range of side effects associated with the use of systemic corticosteroids, this group of drugs is used in the form of a short course with subsequent transition to topical therapy.
Topical calcineurin inhibitors
Interest in the possibility of using topical calcineurin inhibitors was attracted primarily by their anti-inflammatory effect, which is different from tGCs. The mechanism of action of the drugs is realized by suppressing the activity of T cells at the level of transcription factors. Published studies examining the effectiveness of this group of drugs are very contradictory - a meta-analysis performed in 2012, evaluating 3 randomized controlled trials, showed that the effectiveness of pimecrolimus was no greater than placebo. Subsequent studies were more encouraging - according to the data obtained, the effectiveness of topical calcineurin inhibitors was comparable to the effect of tGCs. A 2014 study found that pimecrolimus was slightly more effective than tacrolimus, while more recent studies found that tacrolimus and pimecrolimus were equivalent. These data were confirmed in an open randomized controlled trial (2017), a pilot randomized controlled trial, and a subsequent meta-analysis. Many physicians have found tacrolimus to be more effective in their clinical practice. Side effects of topical calcineurin inhibitors include local irritation and burning, especially on eroded lesions (which limits their use in the case of the erosive form of LP), but in general their safety profile is not inferior to long-term use of corticosteroids. The absence of side effects of TGCS determines increasing interest in the use of these drugs in clinical practice.
Topical and systemic retinoids
Retinoids have certain immunomodulatory effects due to their direct effects on T cells through nuclear retinoic acid receptors. Topical retinoids are an alternative to corticosteroids for non-erosive LP and are recommended as a second-line drug according to World Workshop in Oral Medicine IV. Despite the proven effectiveness of topical tretinoin and isotretinoin 0.1% (in placebo-controlled studies), one study showed lower effectiveness compared to tGCs. Side effects include local irritation, photosensitivity, and teratogenicity. The possibility of disease relapse within 2-5 weeks after stopping use of the drug significantly limits the widespread use of topical retinoids in everyday practice. The use of systemic retinoids (etretinate, isotretinoin) is limited due to an insufficient risk-benefit ratio, however, the use of alitretinoin may be more successful.
Tests and diagnostics
In a typical course, establishing a diagnosis does not present significant difficulties. Difficulties in making a diagnosis may arise with atypical forms of lichen planus and come down to differential diagnosis with other skin diseases, such as candidiasis , erythema multiforme , leukoplakia , toxic-allergic reactions , cutaneous lupus erythematosus ( cleft lichen , squamous cell carcinoma in the early stages, etc. ). Therefore, if necessary, a biopsy is performed with histological examination of the obtained material.
Prevention
Specific prevention of the disease has not been developed. Nonspecific special prevention measures include:
- sanitation/treatment of foci of chronic infection;
- normalization of lifestyle (avoid stress/overwork);
- treatment of psychoneurological disorders;
- maintaining proper oral hygiene;
- timely treatment of somatic/dental diseases;
- following a special diet (excluding chocolate, honey, coffee, spices, alcohol from the diet);
- rejection of bad habits.
Diet
Diet for skin diseases
- Efficacy: therapeutic effect after a month
- Time frame: three months or more
- Cost of products: 1400-1500 rubles per week
Despite the fact that there is no specific diet for lichen planus, the results of patient treatment convincingly demonstrate the significant importance of diet therapy in the complex treatment of the disease. Diet for Skin Diseases can be taken as the basis for diet therapy , which provides recommendations on the choice of products and the formation of a diet. For inflammatory itchy skin diseases, especially during exacerbations, it is necessary to sharply limit or completely eliminate the consumption of fried, canned, spicy, salty, smoked foods and extractive foods (broths based on meat, fish, mushrooms), as well as alcohol-containing drinks. allergic skin diseases, it is necessary to avoid protein allergens (usually fish and egg proteins). In cases of allergic genesis of lichen planus, it is necessary to exclude products with allergenic activity (milk, chocolate, eggs, citrus fruits, etc.). For skin diseases, it is necessary to limit simple carbohydrates in the diet, especially sugar, baked goods, and confectionery, replacing them with complex carbohydrates in the form of whole grain bread, cereals, vegetables, bran, and fruits.
Vegetable fats are recommended because the vitamins A and E weaken allergic manifestations and help accelerate skin healing. It is recommended to include lean meats/poultry, various cereals, fermented milk products, cottage cheese, and boiled/baked vegetables in your diet. Regular fasting days and short-term therapeutic fasting are recommended.
Causes
The causes of lichen planus have not yet been fully established. Presumably, this is a polyetiological disease, the development of which is facilitated by many exogenous/endogenous factors that cause metabolic disorders and changes in the immune response to the actions of the provoking factor, which causes an inadequate tissue reaction (hypersensitivity). Among the causes of lichen planus, a hereditary predisposition can be traced. Lichen planus can develop under the influence of:
- Some toxic drugs ( bismuth , tetracycline ).
- Skin irritating chemicals.
- Stress factors.
- Allergens of various origins
- Diseases of the gastrointestinal tract, liver, pancreas.
- Chronic diseases accompanied by impaired immunity.
- Endocrine disorders ( diabetes mellitus ).
- Injuries to the oral mucosa (sharp teeth, dentures).
Pathogenesis
According to modern theory, it is understood that the pathogenesis of lichen planus is based on a specific delayed-type hypersensitivity reaction that develops in response to exposure to an unidentified (undetected) epidermal antigen. Under its initiating influence, cytotoxic lymphocytes are activated, producing a number of cytokines that, interacting with activated lymphocytes, induce the process of their proliferation and are a factor that triggers cytotoxic mechanisms. The leading pathogenetic mechanism of cell death (keratinocytes) is apoptosis. Morphological changes in the skin/mucosa are the result of a combination of keratinocyte damage/regeneration processes.
List of sources
- Slesarenko N. A., Utz S. R., Artemina E. M., Shtoda Yu. M., Karpova E. N. Comorbidity in lichen planus // Clinical dermatology and venereology. 2014. No. 5. P. 4–10.
- Fedotova K. Yu., Zhukova O. V., Kruglova L. S., Ptashinsky R. I. Lichen planus: etiology, pathogenesis, clinical forms, histological picture and basic principles of treatment. Clinical dermatology and venereology. - 2014 - No. 12(6), pp. 9-20.
- Gadzhimuradov M. N., Gunaeva A. A. Atypical forms of lichen planus: clinical manifestations, differential diagnosis and treatment // Clinical dermatology and venereology. 2009, No. 3, p. 85–80.
- Manukhina O. N. Clinical course of lichen planus of the oral mucosa against the background of decreased functional activity of the thyroid gland. M.: Science to Practice, 2008. pp. 145–147.
- Chuikin S.V., Akmalova G.M. Lichen planus of the oral mucosa: clinical forms and treatment // Kazan Medical Journal. 2014. No. 5. P. 680.