Ketonal (ketoprofen) in the practice of a rheumatologist and therapist
IN
In clinical practice, the most common complaint of patients is pain in the joints, ligamentous-tendon apparatus, and spine.
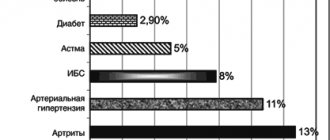
According to international statistics, diseases of the joints and spine confidently compete in frequency with such common diseases as arterial hypertension and coronary heart disease [1,2]. Pain syndrome is most often associated with inflammation of the synovium (synovitis). Inflammatory joint diseases represent an important therapeutic problem not only due to their widespread prevalence among the population, but also due to their chronic course in most cases. The chronic nature of arthritis in various nosological forms (rheumatoid arthritis - RA, ankylosing spondylitis, psoriatic arthritis) dictates the need for long-term anti-inflammatory therapy. The presence of secondary synovitis in arthrosis is an obligatory sign of this disease, which develops in the second half of life, that is, in people who have certain risk factors for the development of complications of anti-inflammatory therapy - age, concomitant diseases and the need for concomitant drug therapy requires treatment taking into account the development of possible complications. Acute arthritis associated with the presence of crystals in the synovial cavity (gout, pseudogout), bacterial infection, trauma, can be stopped in a relatively short period of time, but the severity of the pain syndrome in them requires the prescription of drugs with pronounced analgesic and anti-inflammatory activity. Nonsteroidal anti-inflammatory drugs
are used to treat all of these conditions .
Since the 70s of the last century, NSAIDs have appeared on the market, which have a sufficient anti-inflammatory effect and are relatively well tolerated compared to derivatives of acetylsalicylic acid or phenylbutazone (the latter are currently no longer used due to high toxicity). However, NSAIDs are not free from the development of adverse reactions, which is associated with the mechanism of action of these drugs. As can be seen from Figure 1, all classical NSAIDs bind approximately equally to cyclooxygenase (COX) types 1 and 2, an enzyme involved in the breakdown of arachidonic acid (a derivative of phospholipids of cell membranes that disintegrate when cells are damaged during inflammation) [3] (Table . 1). The discovery of the role of COX-1 and COX-2 is one of the most important in studying the possibilities of treating inflammatory processes. It is known that suppression of COX-1 activity leads to a decrease in the production of physiologically necessary prostaglandins (Table 1), which ensure the normal functioning of the mucous membrane of the gastrointestinal tract (GIT), microvessels, renal interstitium, liver cells, and platelet aggregation. The effect of NSAIDs specifically on COX-1 leads to ulcerative-erosive damage to the gastrointestinal mucosa in more than 30% of patients, to the development of arterial hypertension and peripheral edema, interstitial nephritis, hepatopathy, platelet disaggregation and increased bleeding [4]. Endoscopic technology has made it possible to clarify the frequency of damage to the gastrointestinal mucosa, since in 50–80% of patients NSAID-induced ulcers are asymptomatic [5]. It was noted that a greater number of adverse reactions develop when using NSAIDs with a pronounced anti-inflammatory and analgesic effect, as well as with a long half-life. Among the classical NSAIDs, the most tolerated are ibuprofen and flurbiprofen, propionic acid derivatives. The drug ketoprofen ( Ketonal
) also belongs to the group of propionic acid derivatives and, like other propionates, has a short half-life of about 2 hours. However, the pronounced analgesic effect of Ketonal suggested an extreme degree of suppression of not only COX-2, but also COX-1. This led to the fact that Ketonal began to be used to relieve acute pain in surgery [6,7], oncology [8], and gynecology [9].
Rice. 1. Mechanism of action of NSAIDs
In rheumatological practice, Ketonal has become widely used only in recent years. Ketonal is available in various dosage forms - capsules of 50 mg and tablets of 100 mg (Forte), retard form of 150 mg, suppositories of 100 mg, ampoules of 100 mg, 5% cream, which makes it convenient to select an individual dose and method of administration drug. The daily dose varies from 100 to 300 mg.
The drug, when used in tablet form, is distinguished by a pronounced analgesic effect, which, according to foreign and domestic authors, exceeds the analgesic ability of such well-known NSAIDs as diclofenac, ibuprofen, indomethacin. In addition, many researchers have noted a high percentage of patients who “respond” positively to the use of Ketonal (reduction of pain and inflammatory syndromes), which, according to our data, is 93% when Ketonal is prescribed in oral form (Fig. 2). For most NSAIDs, the response rate is 70–80%.
Rice. 2. The frequency of development of a positive effect when prescribing various NSAIDs to patients with chronic inflammatory diseases of the joints
Some features of the pharmacodynamics and pharmacokinetics of Ketonal have become known - rapid absorption in the gastrointestinal tract, easy penetration into the joint cavity and long-term retention of the drug in the synovial fluid, which, combined with a short half-life (up to 2 hours), rapid elimination of the drug, reduces the risk of developing serious side effects manifestations.
Indeed, according to a meta-analysis of studies on a large cohort of patients (about 20,000), Ketonal has a low risk of developing gastrointestinal complications
(Table 2) [10]. We obtained the same data in our clinical endoscopic study [11] (Fig. 3). Despite the high efficiency, the incidence of ulceration with many months of use of Ketonal was low, no different from that with the use of celecoxib, a selective COX-2 inhibitor.
Rice. 3. The incidence of ulceration during treatment with Ketonal in patients with active rheumatoid arthritis compared with other NSAIDs
In clinical practice, diclofenac (75 mg ampoules) is traditionally often used from intramuscular forms. We conducted a comparative study of the effectiveness and tolerability of the ampoule form of Ketonal for intramuscular injection with a similar form of diclofenac. The study included 30 patients with active RA: 15 of them received 200 mg of Ketonal IM and 15 received diclofenac 150 mg IM daily for 2 weeks. In 3 patients, the dose of Ketonal during treatment was increased to 300 mg/day. The groups of patients did not differ in gender (1 and 2 men, respectively), age (41.54±16.23 and 44.09±12.79 years), duration of RA (7.18±2.98 and 6.71±4 ,89 years old). In both groups there were predominantly patients with II (13 and 12 people) degree of activity, III degree of activity occurred in 2 patients receiving Ketonal, and in 3 patients receiving diclofenac. The severity of the joint syndrome was also the same: the number of painful joints (PJ) was 20.46±10.76 and 21.3±13.3; number of inflamed joints (INJ) – 13.73±6.3 and 11.77±7.12, respectively. As can be seen from Figures 4 and 5, Ketonal is not only not inferior to diclofenac in suppressing inflammation and pain in patients with active RA, but also surpasses it in the severity of pain relief, reducing the number of painful and swollen joints. The overall assessment of the effect of therapy is presented in Table 3. According to this study, the frequency of development of a pronounced effect when using intramuscular injections of Ketonal was achieved in 60% of cases (very good and good effect), and when prescribing intramuscular injections of diclofenac in 33% of cases ( good effect).
Rice. 4, 5. Dynamics of RA activity parameters under the influence of intramuscular administration of ketonal and diclofenac. Note: SB - pain score; SI—articular index; PI—swelling index; NBS - number of painful joints; FMC - number of inflamed (swollen) joints; HAQ - Health Questionnaire (functional test)
Thus, the drug Ketonal has proven itself to be a highly active anti-inflammatory agent, the effect of which is at least as good as diclofenac when administered orally or by injection.
At the same time, Ketonal demonstrates good tolerability not only for the treatment of acute situations, but also for long-term treatment of inflammatory processes. Recently obtained information that Ketonal does not have a negative effect on cartilage [12], combined with the safety of using this effective medicine, allows us to recommend it for use in elderly people for the treatment of secondary synovitis in arthrosis, especially since Ketonal is also available in retard forms. Literature:
1. E.L. Nasonov “Pain syndrome in pathology of the musculoskeletal system” Doctor, No. 4, 2002, pp. 15–19.
2. Adams PF, GE Hendershot, and MA Marano. Current Estimates from the National Health Interview Survey, 1996. National Center for Health Statistics. Vital Health Stat 10(2000). 1999.
3. The role of COX-1 and COX-2
4. Side effects of NSAIDs
5. Asymptomatic NSAID ulcers
6. P.S. Vetshev, M.S. Vetsheva Principles of analgesia in the early postoperative period. Surgery, 2002, No. 12, 49–52
7. P.A. Kirienko, B.R. Gelfand, D.A. Levanovich et al. Comparative assessment of the effectiveness of non-steroidal anti-inflammatory drugs used for postoperative pain relief. Consillium medicum, Surgery No. 2, 2002
8. G.A. Novikov, M.A. Weissman, B.M. Prokhorov et al. Ketonal in the treatment of pain in patients with common forms of malignant neoplasms. Palliative medicine and rehabilitation, No. 3, 2002, 48–51
9. E.K. Aylamazyan, D.A. Niauri, G.M. Ziyatdinova Clinical and economic rationale for the use of ketonal for pain relief after endoscopic interventions in gynecology. Russian Bulletin of Obstetrician and Gynecologist, No. 6, 2002, 51–53.
10. Vey experiences BM “20 years with ketoprofen.” Scand.J.Rheum., 1993, Suppl.90: 1–44
11. Chichasova N.V., Imametdinova G.R., Karateev A.E. and others. Efficacy and safety of ketoprofen (ketonal) for rheumatoid arthritis (clinical and endoscopic study). Scientific and practical rheumatology, 2001; 1:47–52. Our clinical and endoscopic study
12. Huber–Brunning O., Willbrinck B., Vanroy J., Vanderveen MJ Potential influences of ketoprofan on human healthy and osteoarthritic cartilage in vitro. Scand. J Rheum 1989;18:29–32.
Ketonal solution for intravenous and intramuscular administration 100 mg ampoules of 2 ml 10 pcs.
From the hematopoietic and lymphatic systems: rarely: hemorrhagic anemia, hemolytic anemia, leukopenia; frequency unknown: agranulocytosis, thrombocytopenia, bone marrow dysfunction. From the immune system: frequency unknown: anaphylactic reactions (including anaphylactic shock). From the nervous system: often: insomnia, depression, asthenia; uncommon: headache, dizziness, drowsiness; rarely: paresthesia, confusion or loss of consciousness, peripheral polyneuropathy; frequency unknown: convulsions, taste disturbances, emotional lability. From the senses: rarely: blurred vision, tinnitus, conjunctivitis, dry mucous membrane of the eye, pain in the eyes, hearing loss; frequency unknown: optic neuritis. From the cardiovascular system: uncommon: tachycardia; frequency unknown: heart failure, increased blood pressure, vasodilation. From the respiratory system: rarely: exacerbation of bronchial asthma, nosebleeds, laryngeal edema; frequency unknown: bronchospasm (especially in patients with hypersensitivity to NSAIDs), rhinitis. From the gastrointestinal tract: often: nausea, vomiting, dyspepsia, abdominal pain, NSAID gastropathy; uncommon: constipation, diarrhea, bloating, gastritis; rarely: peptic ulcer, stomatitis; very rare: exacerbation of ulcerative colitis, Crohn's disease, gingival, gastrointestinal, hemorrhoidal bleeding, melena, perforation of the gastrointestinal tract. frequency unknown: gastrointestinal discomfort, stomach pain. From the liver and biliary tract: rarely: hepatitis, increased activity of liver enzymes and bilirubin. From the skin: uncommon: skin rash, itching; frequency unknown: photosensitivity, alopecia, urticaria, exacerbation of chronic urticaria, angioedema, erythema, bullous rash, including Stevens-Johnson syndrome, toxic epidermal necrolysis, purpura. From the urinary system: rarely: cystitis, urethritis, hematuria; very rarely: acute renal failure, interstitial nephritis, nephrotic syndrome, abnormal values of renal function indicators; frequency unknown: fluid retention in the body and, as a result, weight gain, hyperkalemia. Other: uncommon: peripheral edema, fatigue; rarely: hemoptysis, menometrorrhagia, shortness of breath, thirst, muscle twitching.