Clinic of mitral valve lesions
Severe mitral stenosis leads to severe shortness of breath, which sharply reduces exercise tolerance.
Left atrial pressure almost always exceeds 25 mmHg. Art., the course of the disease is complicated by pulmonary hypertension, atrial fibrillation, thromboembolic syndrome. Atrial fibrillation: occurs with hemodynamically significant mitral stenosis in 80% of cases and can lead to a sharp deterioration of the condition as a result of a sudden increase in left atrial pressure and pulmonary edema. Thromboembolism of the arteries of the great circle occurs in 20% of cases, 80% of such patients have atrial fibrillation. Embolisms are multiple, repeated in 25% of cases; in half of the cases, cerebral artery embolism occurs. With severe pulmonary hypertension (more than 50 - 60 mmHg), survival rate is less than 3 years.
Publications in the media
Mitral stenosis (MS) is a narrowing of the left atrioventricular orifice, which prevents the physiological flow of blood from it into the left atrium during systole of the left atrium.
Frequency. 0.05–0.08% of the population. In 90% of cases of all acquired heart defects, damage to the mitral valve is detected, 40% of mitral stenoses are isolated. The predominant age is 40–60 years. The predominant gender is female (2:1–3:1).
Etiology • The vast majority of cases (more than 95%) are of rheumatic etiology • A clear rheumatic history can be collected in 50–60% of patients • Almost always debuting before the age of 20 years, after 10–30 years the defect becomes clinically evident • Non-rheumatic cases of the defect include severe calcification of the leaflets and mitral valve rings, congenital anomalies (for example, Lutembashe syndrome - 0.4% of all congenital heart diseases), neoplasms and thrombi in the mitral valve and left atrium, massive vegetations on the mitral valve with infective endocarditis, restenosis after mitral commissurotomy or implantation of prostheses into the mitral position.
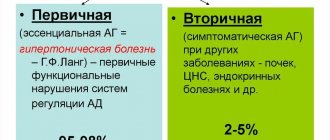
Pathophysiology • The normal area of the mitral orifice is 4-6 cm2 • Narrowing of the left AV orifice impedes the flow of blood from the left atrium to the left ventricle • Diastolic volume and pressure in the left atrium increase (usually in the range of 15-20 mmHg), an increased transmitral gradient occurs (usually within 10–15 mm Hg) • This leads to hyperfunction of the left atrium, its hypertrophy and tonogenic dilatation • The left atrium is a weak part of the heart, and the period of compensation for MS does not last long: the pressure in the heart increases even more left atrium, and then - at the mouths of the pulmonary veins, which leads to passive venous pulmonary hypertension, as well as active hypertension in the pulmonary circulation due to the prolonged Kitaev reflex (spasm of the arterioles of the pulmonary circulation in response to increased pressure at the mouth of the pulmonary veins) • Difficult work of the right ventricle, its hyperfunction, hypertrophy develop, myogenic dilatation, relative tricuspid valve insufficiency and congestion in the veins of the systemic circulation develop quite quickly • Supraventricular tachyarrhythmias are often observed • There are four degrees of MS: minor (mitral orifice area [MO] is more than 3, 0 cm2), moderate (MO area - 2.3-2.9 cm2), pronounced (MO area - 1.7-2.2 cm2) and critical (MO area - 1.0-1.6 cm2).
Clinical picture and diagnosis
• Complaints •• Increased fatigue (20% of all cases) • Interruptions in the work of the heart • Dyspnea (occurs when the area of the heart muscle narrows to less than 2.0 cm2) or cardiac asthma (the most sensitive symptom) • Cough, hemoptysis (the most specific symptom found in 10% of patients) • Ortner's syndrome - hoarseness • History of rheumatic attacks and systemic emboli (20% of all patients and 80% of patients with atrial fibrillation, of which 25% are multiple and repeated) • Angina occurs in 10–15% of cases ( causes - concomitant coronary atherosclerosis, coronary artery embolism, subendocardial ischemia with severe pulmonary hypertension).
• Symptoms associated with enlargement of the left atrium •• Cassio's symptom - delay of the first tone after the apical impulse •• Nesterov's symptom, or two hammers - palpable alternating impulses of the left atrium and left ventricle •• Popov's symptom - reduced filling of the pulse in the arteries of the left upper limb •• Botkin-I symptom - visual decrease in the left half of the chest •• Botkin-II symptom - crepitus and wheezing along the left edge of the sternum •• Auenbrugger symptom - epigastric pulsation of the left ventricle.
• Valvular symptoms •• Diastolic cat purring at the apex of the heart •• Romberg's symptom - flapping 1st sound at the apex of the heart •• The sound of the mitral valve opening (heard at the apex of the heart no later than 0.12 seconds after the 2nd sound), creating, together with Romberg's murmur auscultatory picture of the melody of mitral stenosis, or the rhythm of a quail •• At the apex, low-frequency diastolic murmur is determined in different variants - presystolic, protodiastolic, holodiastolic with proto- and presystolic amplification •• Presystolic murmur is heard with a normal rhythm, the murmur disappears with atrial fibrillation, which often complicates mitral stenosis •• With pronounced stenosis, the murmur may completely disappear •• Often, along with diastolic murmur, systolic murmur is also heard, due to concomitant mitral insufficiency, relative tricuspid insufficiency, and systolic murmur can also be of intraventricular origin •• The murmur of mitral insufficiency is carried out in the left axillary region, tricuspid insufficiency - to the right (on the sternum and to the right of it), intraventricular murmur - upward, the murmur of mitral stenosis intensifies with load (squats, raising legs) and does not go anywhere (“dies where it originates”).
• Symptoms caused by a violation of the pumping function of the heart •• Diffuse moist rales of different sizes, better heard in the basal sections •• Strengthening of the second tone over the pulmonary artery •• Facies mitralis - blush on the cheeks and cyanosis of the lips •• Graham Still's murmur with relative insufficiency of the pulmonary valve •• Expansion of the borders of the heart to the right and push of the right ventricle with its hypertrophy •• Swelling of the neck veins, edema, ascites, enlarged liver, Plesch's symptom - with the development of stagnation in the systemic circulation.
• Symptoms of the underlying disease (rheumatism, congenital heart disease).
Special studies
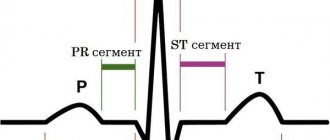
• ECG •• Signs of hypertrophy of the left atrium and right ventricle •• Supraventricular tachyarrhythmias, most often - atrial fibrillation.
• X-ray of the chest organs •• Bulging of the arch of the left atrium, pulmonary artery and right ventricle •• Smoothing of the waist of the heart (mitral configuration) •• Deviation of the contrasted esophagus along a small radius arch •• Widening of the shadows of the vena cava •• Calcification of the mitral valve •• Widening of the shadows roots of the lungs •• Strengthening the pulmonary pattern, Kerley V. lines.
• EchoCG •• Determination of the area of the MR in Doppler mode using peak and average transmitral pressure gradients and in B-mode (to assess the severity, the smallest number is taken as a basis), deformation and calcification of the valve apparatus •• With fusion of the mitral valve leaflets when scanning along the short axis The MO has the shape of a “fish mouth”; during contraction of the left atrium, the anterolateral leaflet bulges into the cavity of the left ventricle, and in the M-mode the characteristic U-shaped movement of the anterior leaflet of the mitral valve is determined •• Enlargement of the left atrium, right ventricle •• In pulsed wave Doppler mode peak E disappears in the spectrum of transmitral blood flow •• Transesophageal echocardiography is performed in all patients to exclude thrombosis of the left atrium and vegetations, even with a normal rhythm, as well as to determine the degree of valve calcification (I degree - calcification is located along the free edges of the leaflets or in the commissures in separate nodes, II degree - calcification of the valves without transfer to the fibrous ring, III degree - transition of calcium masses to the fibrous ring and surrounding structures).
• Catheterization of all chambers of the heart •• Increased pressure in the left atrium and pulmonary artery, as well as the transmitral pressure gradient •• Increased pressure in the right parts of the heart with right ventricular failure •• Conducting functional tests with aminophylline and oxygen to determine the reversibility of pulmonary arterial hypertension and surgical prognosis treatment •• The study is carried out if the clinical picture does not correspond to the echocardiography data.
• Left atriography and ventriculography •• Increased volume of the left atrium •• Slow expulsion of contrast from the left atrium (usually in a thin stream) •• Funnel-shaped border between the left atrium and left ventricle •• The study is carried out if the clinical picture does not correspond to the echocardiography data.
• Coronary angiography. Performed in the presence of episodes of angina and positive results of stress testing, as well as in all women over 45 years of age, men over 40 years of age and all candidates for mitral valve replacement.
TREATMENT
• Drug therapy •• Prevention of infective endocarditis (see Infectious endocarditis) •• Diuretics under the control of echocardiography (possibility of reducing the transmitral gradient and reducing cardiac output) •• b-blockers, incl. in patients with sinus rhythm, by reducing heart rate, they reduce pressure in the left atrium against the background of exercise •• Indirect anticoagulants (maintain INR at 2.0–3.0) for atrial fibrillation, a history of thromboembolism and a sharp increase in the left atrium •• B in the acute period of thromboembolism, heparin is prescribed (activated PTT is maintained 1.5–2 times higher than normal), having previously performed a CT or MRI of the head to exclude intracranial hemorrhages and echocardiography to detect thrombosis of the left atrium and vegetations on the mitral valve •• In case of repeated thromboembolism, a dose of indirect anticoagulants increase until the INR is maintained at 3.0–4.5 and antiplatelet agents are added (for example, acetylsalicylic acid at a dose of 80–160 mg/day).
• Surgical treatment •• Indications ••• Severe and critical stenosis, regardless of the presence of clinical symptoms ••• Moderate stenosis with III-IV functional class of circulatory failure or repeated embolisms •• Contraindications ••• Severe concomitant pathology that threatens the patient’s life •• • Terminal stage of circulatory failure ••• Negative test result with aminophylline and oxygen ••• The activity of the rheumatic process is not considered a contraindication to surgical treatment •• Methods of surgical treatment ••• Percutaneous balloon valvuloplasty is performed in the absence or grade I of mitral valve calcification, preservation of the valve device, isolated stenosis or complex mitral disease with a predominance of stenosis and regurgitation no more than grade I, absence of left atrium thrombosis and concomitant ischemic heart disease ••• Closed mitral commissurotomy is rarely performed due to greater invasiveness and a large number of complications for similar indications ••• Because of due to the high frequency of relapses of the defect and the need for reoperations, open mitral commissurotomy under conditions of artificial circulation is actually performed only together with thrombectomy from the left atrium before a planned pregnancy ••• Mitral valve replacement under conditions of artificial circulation using biological prostheses is performed for children or before a planned pregnancy •• • In other cases (and in all cases of infective endocarditis), the affected valve is replaced with a mechanical prosthesis ••• During pregnancy, surgery is recommended at 14–26 weeks, or at 37–39 weeks simultaneously with a cesarean section.
Specific postoperative complications • Thromboembolism • Secondary infective endocarditis of prostheses • Atrioventricular block • Dystrophic changes in biological prostheses, restenosis and the need for re-prosthesis • Specific complications of balloon valvuloplasty: thromboembolism - 1-4%, severe mitral regurgitation requiring mitral valve replacement - 1-3 %, transient AV block - 1%, cardiac tamponade - 1%, ASD - 20% (the ratio of pulmonary minute volume to systemic blood flow is usually below 1.0, in most cases the size of the defect decreases within 3-6 months).
Prognosis • 1-year survival in the natural course of the disease - 78%, 2-year survival - 67%, 5-year - 50%, 9-year - 35% • Mortality with closed mitral commissurotomy - 0.5–1% • Over the next 10 years, 20% of patients experience restenosis • 5-year survival rate after balloon valvuloplasty - 95%, mortality - about 1% • Mortality during operations with artificial circulation - 2-8% • 5-year survival rate after valve replacement - 85 %, 9-year - 78% • 8-year survival rate after complex reconstructive operations on the mitral valve - 87%, number of complications - 6%, reoperations - 7%.
Synonyms • Mitral valve stenosis • Stenosis of the left atrioventricular orifice • Narrowing of the left atrioventricular orifice • Narrowing of the left venous orifice
Abbreviations • MS - mitral stenosis • MO - mitral orifice
ICD-10 • I05.0 Mitral stenosis
Treatment of acquired heart defects can be conservative or surgical
Conservative treatment is effective only in the early stages of the development of heart disease and requires mandatory follow-up by a cardiologist.
PPS should be treated surgically when:
- Heart failure progresses.
- Pathological changes in the valve significantly affect hemodynamics.
- The ongoing conservative therapy does not have the desired effect.
- And there are fears of serious complications.
Types of operations for heart defects
Open heart surgery is performed under artificial circulation through a median sternotomy. Median sternotomy creates optimal conditions for the cardiac surgeon to perform the necessary surgical interventions for various pathologies and to connect the heart-lung machine. The soft tissue incision is approximately equal in length to the length of the sternum (about 20 cm), and the sternum is dissected along its entire length.
The main two types of operations that are currently used for PPS are reconstruction of the affected valves (plastic) or their prosthetics.
Valve-sparing surgery
Performed to eliminate the cause of valve dysfunction.
If the valves do not close (valve insufficiency), then the cardiac surgeon during the operation achieves normalization of the closure of the valve leaflets, performing resection of the valve leaflets, annuloplasty, commissural plastic surgery, and chord replacement. If there is valve stenosis, then the sections of the valves that have fused due to a pathological process are separated and an open commissurotomy is performed.
Valve replacement surgery
If it is impossible to perform plastic surgery, when there are no conditions for this, valve replacement operations for prosthetic heart valves are performed. In case of intervention on the mitral valve, replacement is performed with full or partial preservation of the anterior or posterior valve leaflets, and if impossible, without their preservation.
In valve replacement surgeries, prostheses are used.
- Prosthetics can be made from animal or human tissue. Such prostheses are called biological. Its main advantage is that the patient does not need to take anticoagulant drugs during subsequent years of life, and their main disadvantage is their limited service life (10-15 years).
- Prostheses consisting entirely of mechanical elements (titanium and pyrolytic carbon) are called mechanical. They are very reliable and can serve without failure for many years, without replacement, but after such an operation the patient must always take anticoagulants for life, this is a negative aspect of using a mechanical prosthesis.
Minimally invasive surgeries
Modern surgery, thanks to the creation of new instruments, has the opportunity to modify surgical approaches to the heart, which leads to operations becoming minimally traumatic for the patient.
The point of such operations is that access to the heart is carried out through small incisions in the skin. During minimally invasive operations on the mitral valve, a right-sided lateral minithoracotomy is performed, with a skin incision of no more than 5 cm, this allows one to completely avoid dissecting the sternum and provides convenient access to the heart. To improve visualization, endoscopic video support with multiple magnification is used. With minimally invasive access to the aortic valve, the skin incision is approximately half as large (incision length 8 cm), and the sternum is incised lengthwise in its upper part. The advantage of this method is that the uncut portion of the sternum provides greater stability after surgery, as well as a better cosmetic effect by reducing the size of the suture.
Endovascular operations - transcatheter aortic valve replacement (TAVI).
Methods of transcatheter aortic valve implantation:
- The entire operation is carried out through a blood vessel (femoral or subclavian artery). The meaning of the procedure is to puncture the femoral or subclavian artery with a guide catheter and deliver the stent valve against the blood flow to the site of its implantation (aortic root).
- Through the aorta. The essence of the method is to dissect the sternum over a short distance (ministernotomy) and puncture the aortic wall in the ascending section and implantation of a stent valve into the aortic root. The method is used when it is impossible to deliver the valve through the femoral and subclavian arteries, as well as when there is a pronounced bend in the arterial arch.
- Through the apex of the heart. The meaning of the procedure is to make a small incision in the fifth intercostal space on the left (minithoracotomy), puncture the apex of the heart with a guide catheter and install a stent valve. Once the new valve is implanted, the catheter is removed. The new valve starts working immediately.
There are two types of stent valves:
- Self-expanding stent-valve expands to the desired size after removing the restrictive sleeve sleeve from it.
- A balloon-dilatable stent valve that expands to the desired size when the balloon is inflated; After final installation of the stent valve, the balloon is deflated and removed.
To determine whether TAVI surgery is appropriate, the patient must undergo a series of tests, including an ECG, echocardiography, computed tomography (CT) scan, and angiography.
Currently, the TAVI procedure is increasingly used not only for aortic stenosis, but also for aortic insufficiency, as well as their combination. In addition, TAVI surgery is used for dysfunction of the biological prosthetic aortic valve.
TAVI surgery is performed under general anesthesia and requires a multidisciplinary approach. The procedure is performed by a specialized team, which includes an interventional cardiologist, cardiac surgeon, anesthesiologist, and radiologist.
The presence of a stent valve is not an indication for the patient to take the indirect anticoagulant Warfarin (in the absence of other indications).
Diet for mitral stenosis
Diet for heart failure
- Efficacy: therapeutic effect after 20 days
- Timing: constantly
- Cost of products: 1700-1800 rubles. in Week
Mitral valve stenosis is accompanied by the development of heart failure , pulmonary hypertension and an increased risk of thromboembolism , so the lifestyle should be as healthy as possible. It is necessary to exclude any harmful products, as well as alcohol, coffee, strong tea, nicotine or any drugs. In addition to moderate physical activity and avoiding stress, it is recommended to monitor the balance of proteins, carbohydrates and fatty acids, and do not forget about auxiliary vitamin therapy and water balance in the body. It is advisable to cross out from the menu:
- fatty foods, especially those of animal origin;
- roast;
- spicy;
- smoked;
- cholesterol-containing products.
The diet should be enriched with potassium and magnesium salts; it should be based on cereals, fruit, vegetable, milk soups, vegetable side dishes, dishes with cheese, poultry and fish. We must not forget about the regular consumption of berries, vegetable juices, raw fruits, and, of course, citrus fruits, apples, dried apricots, prunes, raisins and grapes. In addition, it is very important to limit your fluid and salt intake.
General information
Mitral stenosis is an acquired monovalvular defect that impairs the activity of the heart muscle as a result of morphological and/or functional changes in the structure of the mitral valve.
Normally, it has a bicuspid (bicuspid) structure and is located on the border of the left atrium and the left ventricle, preventing the reverse flow (regurgitation) of blood into the chamber of the left atrium in systole, that is, during ventricular contraction. However, infectious lesions, inflammation, autoimmune reactions, overload, and enlargement of the heart chambers can cause pathological changes in the valve system in the form of narrowing of the atrioventricular orifice, which leads to disruption of intracardiac hemodynamics and systemic blood flow. The disease is characterized by a slow course - the first symptoms may appear after 40-50 years, although the formation of pathological narrowing usually begins at a young age. A downward change in the diameter of the atrioventricular orifice occurs in approximately 0.05-0.08% of the population, more often in females.
Methods for diagnosing heart defects
In order to establish a diagnosis of heart disease, an anamnesis is collected, the presence of diseases that could lead to deformation of the heart valve is revealed: rheumatic diseases, infectious, inflammatory processes, autoimmune diseases, injuries.
- The patient must be examined to identify the presence of shortness of breath, cyanosis, edema, and pulsation of peripheral veins. Using percussion, the boundaries of the heart are identified and sounds and murmurs in the heart are listened to. The size of the liver and spleen is determined.
- The main method for diagnosing valve pathology is echocardiography
, which allows you to identify the defect, determine the area of the opening between the atrium and the ventricle, the size of the valves, cardiac fraction, pressure in the pulmonary artery.
More accurate information about the condition of the valves can be obtained by performing transesophageal echocardiography. - Electrocardiography is also used in diagnostics, which allows one to assess the presence of atrial and ventricular hypertrophy and identify signs of overload of the heart. Daily Holter ECG monitoring allows you to identify rhythm and conduction disturbances.
- Highly informative methods for diagnosing heart defects are cardiac MRI or cardiac MSCT. Computed tomography scans provide precise and numerous sections, which can be used to accurately diagnose the defect and its type.
- Laboratory tests play an important role in diagnosis, including urine and blood tests, determination of blood sugar, cholesterol levels, and rheumatoid tests. Laboratory tests allow us to identify the cause of the disease, which plays an important role in subsequent treatment and patient behavior.
Tests and diagnostics
In addition to echocardioscopy, Dopplerography, phonocardiography, X-ray, ECG (including daily monitoring to determine heart rhythm), 4 standard diagnostic methods are used:
- Upon examination, against the background of pallor of the skin, a purple, sharply defined so-called mitral flush of the cheeks and cyanosis of the lips, as well as the tip of the nose are visible, while it is possible to detect increased epigastric pulsation of the right ventricle (“heartbeat”) against the background of the absence or weakening of the apical beat, because the walls of the left ventricle are not enlarged and are displaced as a result of the process of hypertrophy of the right ventricle.
- Upon palpation, a cardiac hump is revealed, and in the area of the apex of the heart, especially after performing physical exercises in patients in a position on the left side, when exhaling, a diastolic tremor is “audible” in the form of the so-called “cat purr” caused by fluctuations in the blood during passage through the constricted mitral passage, to identify the symptom of Nesterov’s 2 hammers, it is enough to place the palm of your hands on the top, placing your fingers on the second intercostal space on the left of the sternum, you can detect the flapping initial first sound and feel it as the first beat of the “hammer”, while the second tone causes a recoil in the fingers in in the form of a second “hammer”.
- During percussion, a displacement of the border of absolute relative dullness of the heart muscle is revealed upward and to the right (caused by hypertrophy of the left atrium and expansion of the right ventricle, respectively), to a greater extent than the relative one, due to the expansion of the right ventricle, the heart and the expanded edges of the lungs - it is pressed against the chest wall with its right enlarged half.
- Auscultation makes it possible to detect a fairly strong flapping first sound in places above the apex of the heart, since during diastole the filling of the left ventricle with blood does not occur fully and rapid contraction begins, and auscultation also makes it possible to listen to an additional third sound at the apex, which is associated with the opening of the mitral valve and its sharp movements of the valves, this valve defect is characterized by diastolic murmurs and a three-part sound of two tones with a click of the opening of the bicupidal valve at the apex.
Causes
Most often, mitral stenosis develops as a result of previously suffered rheumatism , in other cases the cause becomes:
- infective endocarditis ;
- chronic valvulitis ;
- carcinoid syndrome;
- mitral valve calcification
- thrombus;
- obstruction during the tumor process and the development of myxoma ;
- heart injuries.
Congenital anomaly of the mitral valve in the direction of narrowing of the atrioventricular orifice is extremely rare, for example, with Lutembasch syndrome .