Mitral valve prolapse - symptoms and treatment
Diagnosis criteria
Mitral valve prolapse is most often diagnosed using non-invasive examination methods - the doctor takes into account the patient’s complaints and heredity. But the final diagnosis is made using transthoracic echocardiography.
Instrumental diagnostic methods
During auscultation (listening to the heart) with a stethoscope, the doctor may hear a characteristic systolic click and/or late systolic murmur over the apex of the heart. With the patient standing, the systolic click and murmur appear at the beginning of systole (contraction). With the patient lying or squatting, these sound phenomena are reduced.
The electrocardiogram can detect nonspecific changes in the ST segment and T wave in leads III and aVF. In the presence of mitral valve prolapse, the ECG can diagnose the phenomenon of pre-excitation (“short PQ syndrome”), supraventricular (atrial) tachycardia, and ventricular extrasystole.
chest x-ray Cardiac enlargement may be diagnosed in some patients with a very small anteroposterior chest size.
Transthoracic echocardiography ( Echo-CG) . It is carried out using an ultrasound sensor placed by a doctor on certain points of the chest. It is the most important routine examination in the diagnosis of mitral valve prolapse. Distinctive and important echocardiographic signs of this pathology include deflection of the posterior or both leaflets of the mitral valve into the cavity of the left atrium in mid-systole, in late systole or throughout systole. Deflection (sagging) of the mitral valve in mid-systole is more common, which corresponds to the data obtained by auscultation and angiography.
There are other echocardiographic signs, they are nonspecific, but highly sensitive:
- dilatation (expansion) of the mitral ring;
- increased range of motion of the mitral valve, diastolic contact of the leaflets with the interventricular septum;
- an increase in the range of diastolic divergence of the leaflets and the speed of opening of the anterior valve leaflet;
- systolic displacement of the anterior and posterior leaflets of the mitral valve (more than 3 mm) into the left atrium below the closure of the mitral line;
- thickening of the mitral valve leaflets;
- signs of disruption of the internal structure of the valve tissue (myxomatous valve degeneration);
- reverse blood flow;
- signs of increased pressure in the pulmonary artery.
Transthoracic echocardiography is recommended every 6 to 12 months in all asymptomatic patients with moderate to severe mitral regurgitation. This is necessary to assess the ejection fraction (pumping function of the heart, normally it should be at least 55%) and end-systolic size.
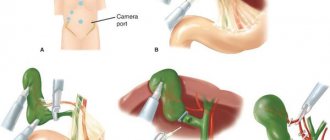
Transesophageal echocardiography. This is an ultrasound test in which a probe is inserted into the esophagus. Indicated only in the absence of contraindications in the following cases:
- Echo-CG does not assess the severity and mechanism of mitral regurgitation and/or the state of left ventricular function;
- The patient is about to undergo valve surgery; during the examination, the question of the nature of the surgical intervention is decided.
A type of prolapse is the so-called valve . It is usually detected by rupture of the chordae or avulsion of the papillary muscle (more common in acute myocardial infarction). With echocardiography in B-mode, the freely moving papillary muscle and the “dangling” mitral valve leaflet are clearly visible. The valve makes irregular, voluntary movements during diastole (the period of relaxation of the heart muscle) and “falls” into the cavity of the left atrium during ventricular systole. In M-mode, characteristic echocardiographic signs of such a valve are the presence of:
- additional echo signals from the mitral valve leaflet in the cavity of the left atrium during the period of ventricular contraction;
- diastolic vibration of the anterior valve leaflet or paradoxical movement of the posterior mitral leaflet in systole and diastole.
Radionuclide equilibrium ventriculography is performed to assess ejection fraction and assess the severity of heart failure. The method is based on the intravenous administration of a radionuclide with its fixation on red blood cells and subsequent quantitative assessment of the contractility of the heart.
Differential diagnosis
The strategy and tactics of patient management depend on the origin of the prolapse - congenital or acquired, therefore differential diagnosis is carried out only between these types of mitral valve prolapse.
Publications in the media
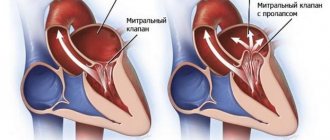
Mitral valve prolapse (MVP) is a pathological sagging (bending) of one or both mitral valve leaflets into the left atrium during left ventricular systole. Statistical data. MVP is found in 3–8% of people in the general population (apparently, the data is overestimated). Manifestations of MVP are first recorded at the age of 10–16 years; after 10 years, girls are observed 2 times more often.
Etiology. MVP can be primary or secondary • Primary MVP •• A disease inherited in an autosomal dominant manner with myxomatous deformation of the mitral valve leaflets •• MVP is also observed in patients with Marfan syndrome and other congenital connective tissue diseases, such as Ehlers-Danlos syndrome, elastic pseudoxanthoma, osteogenesis imperfecta •• In the occurrence of MVP, exposure to toxic agents on the fetus on the 35–42nd day of pregnancy may also be important • Secondary MVP can occur with: •• IHD (ischemia of the papillary muscles) •• rheumatism (post-infectious sclerotic changes) • • hypertrophic cardiomyopathy (disproportionally small left ventricle, change in the location of the papillary muscles).
Pathogenesis • Primary MVP •• Myxomatous degeneration of collagen leads to excessive accumulation of mucopolysaccharides in the middle spongy part of the mitral valve leaflets and its hyperplasia, which causes the appearance of break areas in the fibrous part of the valve. Local replacement of the elastic fibrous tissue of the valve leaflet with a weak and inelastic spongy structure leads to the fact that during systole, under the influence of blood pressure from the left ventricle, the leaflet bulges towards the left atrium (prolapses) •• In the occurrence of primary MVP in Marfan syndrome, it is also important dilatation of the annulus fibrosus of the mitral valve - it does not decrease by 30% in systole, as is normal, which leads to protrusion of one or both leaflets into the cavity of the left atrium • Secondary MVP occurs as a result of thinning and elongation of the tendon threads or their separation or dilatation of the fibrous ring. Lengthening of the tendon threads, separation of part of them lead to the fact that the leaflet is not held in place and begins to prolapse into the left atrium • If the mitral valve leaflet is excessively bowed, mitral regurgitation may occur with dilatation of the left atrium and left ventricle. It should be noted that MVP can be combined with prolapse of other valves: tricuspid valve prolapse in 40% of cases, pulmonary valve prolapse in 10%, aortic valve prolapse in 2%. In this case, in addition to mitral valve insufficiency, manifestations of insufficiency of the corresponding valve will occur. There is often a combination of MVP with other congenital anomalies of the heart - ASD, additional conduction pathways (usually left-sided).
Clinical manifestations • Complaints •• In most cases, MVP is asymptomatic and is detected by chance during a preventive examination •• With more severe prolapse, patients complain of palpitations (ventricular extrasystole, paroxysmal supraventricular tachycardia, less often ventricular tachycardia) •• A common complaint is pain in the chest. It can be either atypical or typical anginal due to spasm of the coronary arteries or ischemia as a result of tension of the papillary muscles •• Shortness of breath during physical exertion, fatigue are also noted by patients with MVP •• Extremely rare manifestations are visual impairment as a result of thromboembolism of the retinal vessels, and also transient ischemic attacks as a result of cerebral thromboembolism. In the occurrence of embolic complications, importance is attached to the separation of fibrin threads located on the atrial side of the mitral valve •• Often the above-described complaints are accompanied by psycho-emotional lability • Upon examination, concomitant congenital abnormalities of the chest shape can be identified - kyphoscoliosis, funnel-shaped chest, pathologically straightened back, reduced anteroposterior chest size cells or signs of Marfan syndrome • Auscultation of the heart (a “silent” form of MVP is possible) •• The main auscultatory sign of MVP is a short mid-systolic high-frequency click (pathognomonic). It appears as a result of sagging of the mitral valve leaflets in systole into the cavity of the left atrium and their sharp tension •• The systolic click may be followed by a mid- or high-frequency late systolic murmur, better heard at the apex of the heart •• To clarify the manifestations of MVP, dynamic auscultation of the heart is used •• • Changes in left ventricular end-diastolic volume result in changes in the timing of the click and murmur. All maneuvers that contribute to a decrease in end-diastolic volume, an increase in heart rate, or a decrease in resistance to ejection from the left ventricle lead to MVP appearing earlier (the click noise approaches the first sound). All maneuvers that increase blood volume in the left ventricle, reduce myocardial contractility or increase afterload increase the time from the beginning of systole to the appearance of a click noise (moves back to the second sound) ••• In the supine position, the click occurs later, the noise is short ••• In the position standing, the click occurs earlier, and the noise is longer ••• In the squatting position, the click occurs later, and the noise is shorter (may even disappear). Instrumental data • Usually no changes are detected on the ECG in patients with MVP. Of the detected deviations, depression of the ST segment or negative T waves in leads III, aVF are most often noted. These changes may reflect ischemia of the inferior wall of the left ventricle as a result of tension in the posterior papillary muscle due to leaflet prolapse. In patients with ECG changes, cardiac arrhythmias also occur. Some patients experience prolongation of the QT interval. Recording an ECG after taking beta-blockers increases the specificity of this method • EchoCG •• In one-dimensional mode, the “hammock” symptom is detected - sagging of one or both leaflets in systole by more than 3 mm •• In two-dimensional mode, sagging of the mitral valve leaflets into the cavity of the left atrium in systole is detected left ventricle, thickening of the leaflets more than 5 mm in diastole, lengthening of the tendon filaments, lengthening of the leaflets, dilatation of the fibrous ring •• There are three degrees of MVP, determined in a four-chamber section ••• I degree (minor) - sagging of the leaflets into the cavity of the left atrium up to 5 mm ••• II degree (moderate) - sagging of the leaflets into the cavity of the left atrium 5-10 mm ••• III degree (severe) - sagging of the leaflets into the cavity of the left atrium more than 10 mm •• Doppler examination can reveal a regurgitation jet in the left atrium. With severe MVP, dilatation of the left atrium and left ventricle occurs, detected in one- and two-dimensional modes. It should be remembered that in the presence of typical auscultatory signs of MVP, its EchoCG signs may be absent in 10% of patients. When conducting the study, you should remember about other congenital heart defects (in particular, ASD). Differential diagnosis • Mitral valve insufficiency of rheumatic origin • Isolated aneurysm of the interatrial septum • Isolated tricuspid valve prolapse • VSD.
TREATMENT Management tactics • Treatment of the underlying disease in secondary MVP • Risk groups for the development of complications (patients with severe systolic murmur, thickened prolapsed mitral valve leaflets, left ventricular hypertrophy, rhythm disturbances, fainting) undergo regular ECG, echocardiography • Prevention of endocarditis is indicated for persons with severe systolic murmur. Treatment of various options • For asymptomatic MVP without signs of mitral valve insufficiency, there is no need for treatment •• The patient should be given recommendations for normalizing lifestyle, optimizing physical activity (a decrease in the tone of the sympathetic nervous system can lead to a decrease in valvular dysfunction) •• EchoCG is recommended -control once every 1–2 years •• It is necessary to avoid drinking strong tea, coffee, alcohol, as well as smoking • For severe MVP •• If there are symptoms of MVP such as tachycardia, palpitations, chest pain, is prescribed -adrenergic blockers in small doses (for example, propranolol at a dose of 30–60 mg/day) •• In case of dilatation of the left atrium and left ventricle, prolongation of the QT interval, a history of fainting, dilatation of the initial part of the aorta, physical activity is prohibited •• Prevention is recommended infective endocarditis using amoxicillin •• For symptoms of embolization, acetylsalicylic acid is prescribed at a dose of 80–325 mg/day •• With significant changes in hemodynamics, increasing symptoms of mitral valve insufficiency, mitral valve replacement or annuloplasty is performed.
Prognosis and complications . Typically, MVP is benign. Complications of MVP most often occur in patients with systolic murmur, thickened, elongated mitral leaflets, or enlarged left ventricular cavity or left atrium. Complications include: • separation of tendon threads • severe mitral valve insufficiency (0.06%) • fibrin deposition on the mitral valve leaflets • cardiac arrhythmias • cerebrovascular pathology (0.02%) • infectious myocarditis (0.02%) • sudden cardiac arrest death (0.06% of cases with severe mitral valve insufficiency). Synonyms • Systolic click-murmur syndrome • Barlow's syndrome • Inflated mitral valve syndrome. Reduction. MVP - mitral valve prolapse.
ICD-10 • I34.1 Prolapse [prolapse] of the mitral valve