Psychiatry Psychiatry and psychopharmacotherapy named after. P.B. Gannushkina No. 09 2003
Introduction
Since the introduction into clinical practice of the first thymoanaleptics—tricyclic antidepressants (TCAs) and nonselective, irreversible MAO inhibitors (MAOIs), the constant search for new drugs for the treatment of depression continues. Today, there is a wide variety of thymoanaleptics that differ in chemical structure and mechanisms of action, which makes it very difficult for a doctor to choose the most adequate antidepressant for the treatment of a specific depressive condition. In accordance with the recommendation issued by the British Association for Psychopharmacology in 1993, the following factors are essential when choosing an antidepressant: severity of side effects, effectiveness, risk of overdose, price. Taking into account these 4 factors is complicated by their significant differences in individual drugs, especially in the traditionally used TCAs and MAOIs, as well as in new groups of antidepressants that have appeared in recent years - selective serotonin reuptake inhibitors (SSRIs) and reversible selective MAO type A inhibitors (RSMAs). This primarily relates to the significant difference in the occurrence of psychomotor and cognitive impairment caused by TCAs and SSRIs, especially in patients undergoing treatment in an outpatient setting and maintaining their daily and work activities. The results of numerous studies of adverse side effects have shown that cognitive and psychomotor impairment, as well as sedation caused by TCAs, significantly limit their use, since many of them develop at therapeutic doses (M. Dukes, L. Beeley, 1998) and require transfer of the patient to suboptimal dosages, which leads to prolongation of therapy. SSRIs are better tolerated than TCAs, however, in numerous studies (J. Edwards, 1992; P. Finley, 1994; S. Montgomery, S. Kasper, 1995), confirmed by a meta-analysis of 55 published papers (J. Anderson, B. Tomenson, 1994 ), SSRIs have been convincingly shown to be inferior to TCAs, especially in the treatment of severe depression. In this regard, there is a need to develop a new antidepressant that combines the mechanisms of action of TCAs (non-selective inhibition of monoamine reuptake) and SSRIs (selective inhibition of serotonin reuptake without affecting postsynaptic receptors). The integrative mechanism of action of such a thymoanaleptic allowed us to hope for a new, more advanced drug in the arsenal of antidepressants. One of these drugs is the thymoanaleptic Ixel (milnacipran hydrochloride), a non-selective serotonin and norepinephrine reuptake inhibitor, produced by Pierre Fabre Medicament, France. Unlike most TCAs, Ixel has no affinity for cholinergic (muscarinic), adrenergic, or histaminergic H1 receptors. However, Ixel also has no affinity for dopaminergic receptors D1 and D2, benzadiazepine and opioid receptors. Ixel is well absorbed when taken orally. Bioavailability is about 85%, does not depend on the nature and diet. The maximum plasma concentration (Cmax) is reached approximately 2 hours (Tmax) after administration. After a single dose of 50 mg, it is approximately 120 ng/ml. The concentration in the blood plasma increases in proportion to the dose taken, reaching up to 200 mg after a single dose. After repeated doses, equilibrium is achieved within 2–3 days with an increase in concentration from approximately 70 to 100% relative to a single dose (Cmax = 216 ng/ml). Interindividual differences are weak. Plasma protein binding is weak (13%) and is not accompanied by saturation. The volume of distribution of Ixel is approximately 5 l/kg with a total excretion coefficient of 40 l/h. Renal and non-renal clearances are equal. The metabolism of Ixel is limited primarily to conjugation with glucuronic acid. There is no active metabolite. The half-life is 8 hours. It is excreted primarily by the kidneys (90% of the dose taken) with secretion of unchanged drug by the renal tubules. After repeated doses, Ixel is completely eliminated from the body 2-3 days after discontinuation of the drug. At a therapeutic dose, the concentration of the drug in the blood plasma is constantly at a level corresponding to the inhibition of the reuptake of norepinephrine and serotonin from 50 to 90%. The pharmacological effects observed in the digestive and genitourinary systems appear to be associated with inhibition of norepinephrine uptake, which has an antagonistic effect on acetylcholine (indirect anticholinergic effect). Ixel does not cause changes in repolarization or cardiac conduction system. It does not affect the patient's responses to cognitive tests and has a mild sedative effect. Depressed patients treated with Ixel note a decrease in sleep disturbances. The period of falling asleep is shortened, the number of night awakenings is reduced, and the latency period for the onset of REM sleep increases, as well as the duration of sleep itself.
Material and treatment methods
At the Department of Psychiatry, Federal University of the Russian State Medical University, an open, simple clinical study was conducted to study the therapeutic effectiveness and safety of the use of the drug “Ixel” (capsules of 25 and 50 mg of active substance) in patients with depressive disorders.
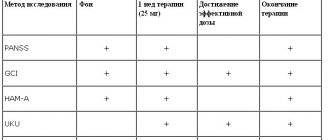
The duration of studying the effect of the drug in each patient was 60 days. The duration of the study was planned to be 6 months, starting from the date of initiation of drug use in the first patient. The study was carried out using the clinical method and standardized rating scales. The dynamics of the patients' condition, the effectiveness and tolerability of treatment were assessed on the basis of clinical data using adequate statistical methods. Ixel was prescribed as monotherapy or, if necessary (see below), in combination with other psychotropic drugs 7 days (“washout” period) after discontinuation of previous treatment. The patients' condition was assessed on the day of Ixel prescription, 3, 10, 20, 30, 45 and 60 days of therapy. The effectiveness of ixel was assessed using unified rating scales: • the Clinical Global Impression Scale (CGI), • the Montgomery-Åsberg Depression Rating Scale (MADRS), • the Hamilton Depression Rating Scale, n-17 (CHDRS), as well as adverse event registration cards (AE) and side effects (AE). Patients who were unable to accept the conditions of the protocol and those with a high probability of refusing to comply with them were excluded from the study. Ixel was also not prescribed to patients with signs of the following disorders according to ICD-10 at the time of the study or within 3 months before the start of the study: • delirium, dementia, amnestic or other cognitive disorders (F.0); • alcoholism, drug addiction (F1); • anxiety-phobic disorders (F40, F41); • obsessive-compulsive disorder (F42); • reaction to severe stress and adaptation disorders (F43); • persons suffering from liver and kidney failure; • patients with prostatic hyperplasia; • patients with arterial hypertension and cardiopathy; • pregnant and breastfeeding women; • persons with hypersensitivity to Ixel; • persons under 18 and over 65 years of age. Ixel was prescribed for moderate or mild depression at a dose of 50 mg (25 mg 2 times a day) or 100 mg (50 mg 2 times a day), increasing the dosage to 100–150 mg/day. To correct anxiety or prevent anxiety disorders at the beginning of therapy, treatment with Ixel was combined with tranquilizers (phenazepam 0.001 g 3 times a day - n=2; seduxen 0.005 g 3 times a day - n=1) and hypnotics (imovan 0.0075 g at night – n=2). Ixel was not combined with the following drugs: • MAO inhibitors, especially non-selective ones (risk of serotonergic syndrome); • lithium salts (risk of serotonergic syndrome); • adrenaline and norepinephrine (hypertensive crisis and heart rhythm disturbances are possible); • clonidine and its derivatives (possible inhibition of the hypotensive effect of clonidine); • sumatriptan (possible increase in blood pressure, suppression of coronary arterial vasoconstriction with suppression of serotonergic effects); • digoxin (risk of potentiation of hemodynamic disorders). As can be seen from the data in table.
1 , the present study included a large group of patients with depressive disorders in terms of diagnostic criteria and characteristics of clinical symptoms. For greater purity of the experiment, patients with current somatic disorders were excluded from the number of outpatients (n=14) and those receiving Ixel in the clinic (n=16). This made it possible to focus more attention on the purely thymoanaleptic effect of Ixel, followed by a multifaceted assessment of it as an antidepressant.
The present study included mainly middle-aged (most able-bodied) individuals, which made it possible to evaluate Ixel not only as a true antidepressant, but also as a drug that can have a positive impact on the quality of life of patients. Ixel was prescribed to 31 patients. Due to the fact that 1 patient stopped taking the drug after 3 days of therapy without explanation and did not show up for subsequent appointments, he was excluded from the study. Thus, the total number of patients receiving Xel is 30 patients. Of the 30 patients included in the study, 14 combined treatment with Ixel while maintaining their work, family, and social status (outpatients). More than half of the patients (53.3%) were patients with bipolar affective disorders with predominantly moderate current depressive episodes (30%). The second largest group consisted of people with a depressive episode (30%), in contrast to the first group, it was slightly dominated by people with a mild depressive episode (16.6%). The number of patients receiving Ixel also included patients with recurrent depressive disorder (16.6%). The criteria for assessing patients were based on the concepts of the International Classification of Diseases (10th revision) “Classification of Mental and Behavioral Disorders”, and therefore the specification of diagnostic criteria does not require more detailed justification. In the process of assessing the condition of the patients, we did not note any significant differences in their status. However, the syndromological characteristics require some clarification, which is essential for assessing the pharmacodynamics of Ixel. In all patients (n=30), the condition was determined by a decrease in mood to a distinct, previously unusual level, which was observed for most or the whole day for at least 2 weeks and did not significantly depend on external circumstances. Along with this, all patients noted a loss of interest and satisfaction from previously usually pleasant or everyday habitual activities, a decrease in motivation, energy, or increased fatigue with psychomotor impairment and the appearance of lethargy (n = 16). In addition, subjectively perceived and/or objectively determined decreases in concentration, uncertainty and/or indecision were noted. Unexpressed suicidal thoughts were noted in 9 patients, sleep disturbances (mainly pre- and intrasomnic disorders) - in 12, and decreased appetite - in 23 patients. In addition, against the background of predominantly asthenoadynamic disorders in the structure of the depressive state, a feeling of slight anxiety was revealed in 8 patients, which influenced the subsequent results of Ixel therapy and the occurrence of side effects. According to the severity of depressive disorders (severity of depression), their condition was considered within the framework of a mild depressive episode (46.7% of cases), as well as a moderate depressive episode (53.3% of cases). Results of using the drug “Ixel” The results of long-term (D60) use of the drug “Ixel” indicate its high therapeutic effectiveness. Analyzing the dynamics of the patients’ condition and the results of Ixel therapy, reflected in the Clinical Global Impression (GCI) scale, the following conclusions can be drawn ( Table 2
).
As can be seen from the data in table. 2
, “disease severity” decreased from 3.8 to 0.6 points over 60 days of therapy.
However, by the 20th day of treatment, we noted a statistically significant decrease in the severity of depressive disorders. Accordingly, these days, both objectively when assessing the condition of patients and when carrying out statistical calculations, a significant “general improvement” was noted, which underwent dynamics from 4.1 to 0.8 points over 60 days of therapy. In this regard, the patients’ condition was categorized as “great improvement” and/or “very great improvement.” Only 3 patients with moderate depression had results indicating “slight improvement.” The therapeutic effect in 78.1% of patients was assessed as “significant; significant improvement or complete remission.” In 21.9% of cases, the therapeutic effect did not go beyond “moderate; improvement; partial remission.” Despite the fact that SHOKV reflects the total data made up of the multi-directional effects of Ixel, we did not determine a significant difference between the effect of the studied drug on patients with different diagnostic criteria (bipolar affective disorder, depressive episode, recurrent depressive disorder), as well as patients whose depression was assessed as moderate and/or mild. The pharmacodynamic effects of Ixel were recorded and assessed using specialized unified rating scales, in particular the Montgomery-Asberg Depression Rating Scale (MADRS). As can be seen from the data in table.
3 , the reduction in the average total MADRS score begins from the first days of taking Ixel.
Already in D10 we can state a statistically significant decrease in the average total MADRS score. At the same time, it should be noted that the most intense reduction occurs in the first (D1–D10) days of therapy. This indicates the rapidity of the therapeutic effect of the drug. In addition to the rapid onset of the therapeutic effect, Ixel is also distinguished by its high therapeutic effectiveness. By the end of treatment (D60), the average total MADRS score decreased from 25.2 to 4.7. When analyzing data on the dynamics of individual psychopathological signs observed in patients, different rates of normalization of individual signs taken into account were noted. Lethargy and associated asthenic and adynamic disorders decreased most intensively (D10 – p<0.005). Subsequently (D20 – p<0.001), an intense positive effect of ixel on a whole group of disorders was noted: visible and described sadness; internal tension; sleep disturbance; inability to feel; pessimistic and suicidal thoughts; lack of concentration. Such a harmonious effect on the reduction of individual depressive disorders indicates the complex integrative mechanisms underlying the intimate action of Ixel. In the first days of treatment (D1–D3), in a number of cases, increased internal tension and deterioration in sleep were noted, which required drug correction (see below). More detailed results were obtained when assessing the effectiveness of Ixel using the Hamilton Depression Rating Scale (HDRS). As can be seen from the data in table.
4 , the total HDRS score decreased from 26.3 to 3.5 during the Ixel treatment period. Thus, the therapeutic effectiveness of this drug after D60 is 86.7%.
These data further confirm the previously obtained idea of the high therapeutic activity of Ixel, as well as the speed of onset of the therapeutic effect (D10 - p<0.001). A detailed analysis of the dynamics of the patients' condition using HDRS allows us to conclude that Ixel has an activating effect. This is evidenced by the intensive reduction of inhibition (D10 – p<0.005), as well as the rapid normalization of the patients’ performance (D10 – p<0.001). An indirect criterion for the activating effect of Ixel can be a short-term and slight increase in agitation, mental anxiety and early insomnia (D3). These symptoms were easily relieved by the administration of hypnotics and daytime tranquilizers (see below). Subsequently, dissomnia disorders underwent intensive reverse reduction and almost all groups of sleep disorders (pre-, intra- and post-somnia disorders) were not observed after D20. Equally intense was the positive dynamics of suicidal tendencies, feelings of guilt, lethargy, agitation and general somatic symptoms. When using Ixel, an uneven reverse dynamics of the severity of somatic anxiety was noted. At D30, 2 patients experienced an increase in gastrointestinal disorders, which required a reduction in the dose of the drug. In all likelihood, this is due to the serotonergic effect of Ixel. The activating effect of Ixel was one of the factors in the normalization of sexual disorders (libido in men and women; normalization of the menstrual cycle in women). In parallel with the improvement in the general condition of patients, due primarily to the normalization of depressed mood and self-esteem of patients, an improvement in appetite and an increase in low body weight were noted. The least favorable results were obtained in the treatment of hypochondria. This is explained by the fact that 3 patients (persons with anxious and suspicious character traits in premorbid), regardless of their condition (phase-remission), treated their health with a certain degree of supervaluation, constantly listening to the sensations in the body, and were actively searching for new drugs and methods treatment. In general, the data on HDRS practically do not differ from the results obtained using MADRS, and confirm previously made conclusions about the speed of therapeutic action and the high effectiveness of the drug “Ixel”.
Adverse events (AEs) and side effects (AEs)
With long-term (D60) use of Ixel, a number of AEs and AEs were noted. A total of 12 AEs were identified in 8 (26.7%) patients. In the first days of therapy, an increase in anxiety was noted in 3 patients, which in 2 patients was accompanied by sleep disturbances (primarily presomnia disorders), as well as the appearance and/or intensification of irritability. Increased feelings of anxiety and irritability were relieved by the prescription of tranquilizers, which were discontinued after 2 weeks; dyssomnic disorders normalized after the administration of Imovan, which the patients took for 7–10 days. On D10 and D20, a slight increase in blood pressure (both systolic and diastolic) was noted, and on D30, 3 patients developed a feeling of nausea. In all 5 cases, the method of leveling AEs was to reduce the dose of Ixel to 100 mg/day. It should be noted that Ixel not only causes a small number of AEs, but the severity of these events in all patients was assessed as mild.
Discussion
A long-term (D60) study of the drug “Ixel” in capsules of 25 and 50 mg in 30 patients, as well as subsequent analysis of the results obtained, indicate its high therapeutic effectiveness.
Patients with depressive disorders that could be classified as moderate (average total MADRS score of 25.2 and HDRS of 26.3) received Ixel in doses of 50–150 mg per day. Based on the mechanism of action of Ixel (potentiation of serotonin-noradrenergic structures of the brain and the absence of an effect on a number of postsynaptic receptors), it was possible to assume possible pharmacodynamic features of the action of this drug. In the dynamics of treatment with Ixel, first of all, its general activating effect is revealed, including its effect on the psychomotor sphere. This therapeutic effect is associated with the noradrenergic properties of the antidepressant under study. The general activating effect of Ixel also caused the appearance of a number of AEs in the first days of therapy ( Table 5
).
The pronounced thymoanaleptic effect of Ixel, revealed during therapy, is the result of potentiation of serotonergic structures of the brain. It should be noted that there was a fairly uniform decrease in all depressive disorders, which indicates the harmonious effect of Ixel on the complex integrative processes that underlie the pathogenetic mechanisms of depression. This, in all likelihood, determines the speed of onset of the therapeutic effect identified when taking Ixel. A small number of AEs are most likely determined by the lack of affinity of Ixel for cholinergic (muscarinic), adrenergic, histaminergic H, as well as dopaminergic D1 and D2 and benzodiazepine receptors. This determines not only the low frequency and severity (degree) of AEs, but also the absence of a sedative effect in Ixel.
conclusions
Ixel (milnacipran) in capsules of 25 and 50 mg is an effective, well-tolerated antidepressant with a mild activating effect, without sedation. The remaining conclusions are formulated in the article “Ixel (milnacipran): generalized results of a clinical study of a selective serotonin and norepinephrine reuptake inhibitor (SNRI) in Russia” with our participation.
Ixel, 56 pcs., 50 mg, capsules
When drugs that affect the reuptake of serotonin are combined with drugs that suppress its metabolism (including MAO inhibitors and antipsychotics), the development of serotonin syndrome is possible. Serotonin syndrome or malignant neuroleptic syndrome (manifested by increased nervous excitability, the development of hallucinations, coma, tachycardia, blood pressure lability, hyperthermia, hyperreflexia, impaired coordination of movements, nausea, vomiting, diarrhea) poses a potential danger to the patient’s life.
Ixel can be prescribed no earlier than 2 weeks after discontinuation of MAO inhibitors. The time interval from the moment you stop taking Ixel before starting therapy with MAO inhibitors should be at least 1 week.
Ixel should be used with extreme caution in patients with prostatic hyperplasia, a history of epileptic seizures, as well as in patients with arterial hypertension or hypertrophic cardiomyopathy (especially obstructive).
In children, adolescents and people under 24 years of age, when prescribing antidepressants, the risk of suicidal thoughts and suicidal behavior increases, and therefore, when prescribing milnacipran to this category of people, the risk of suicide should be weighed against the benefits of their use.
In short-term studies, the risk of suicide did not increase in patients over 24 years of age, and even decreased slightly in those over 65 years of age. During treatment with antidepressants, all patients should be monitored for early detection of disturbances or changes in behavior, as well as suicidality.
Drugs that inhibit the reuptake of norepinephrine and serotonin (including milnacipran) can cause increased blood pressure and increased heart rate. However, it should be noted that the severity of these phenomena when taking recommended doses is usually insignificant, is not felt by patients and usually does not require drug correction. Studies on the effect of milnacipran on blood pressure in patients with concomitant uncontrolled arterial hypertension, as well as on heart rate in patients with rhythm disturbances, have not yet been conducted. However, before starting treatment, during dose selection and during treatment, monitoring of blood pressure and heart rate levels is required. For persons suffering from arterial hypertension or other cardiovascular diseases, it is advisable to select effective therapy before prescribing milnacipran.
Cases of increased liver transaminase activity (up to 3 times higher than ULN) in patients taking milnacipran have been described. There was no clinically significant increase in bilirubin. There are isolated reports in the literature about the development of toxic hepatitis in patients while taking milnacipran, however, according to these reports, a clear cause-and-effect relationship cannot currently be traced (there were simultaneous use of other drugs and previous concomitant diseases of the hepatobiliary organs.
If signs of liver damage appear while taking milnacipran, its use should be discontinued. It is undesirable to prescribe milnacipran to persons who abuse alcohol and/or have concomitant liver diseases.
During treatment, it is not recommended to drink alcohol (milnacipran can potentially enhance the negative effects of ethanol on the liver).
With abrupt withdrawal of milnacipran, the following are possible: mood swings, agitation, weakness, paresthesia, anxiety, headache, drowsiness, emotional lability, convulsive syndrome. The severity of these phenomena is usually insignificant, but if they develop, the rate of drug withdrawal should be reduced.
Prescribing milnacipran to patients with a history of mania and/or hypomania should be done with caution due to the potential for exacerbation of these conditions.
Based on the mechanism of action, milnacipran can potentially cause (intensify) disturbances in the outflow of urine (primarily in patients with concomitant prostatic hypertrophy and prostatitis), which certainly requires appropriate monitoring.
Milnacipran, causing pupil dilation, can contribute to an increase in IOP (should be taken into account in patients with initially high ophthalmotonus against a background of poorly controlled angle-closure glaucoma).