Seroquel
Seroquel (quetiapine) is a new-generation antipsychotic drug for the treatment of schizophrenia and other psychoses. In terms of their therapeutic effects, antipsychotics are similar to each other: the main differences between drugs in this group are related to the spectrum and severity of side effects. Traditional antipsychotics cause a whole range of undesirable side reactions, the greatest clinical significance of which are extrapyramidal symptoms, which, in turn, increase the risk of developing depressive conditions, reduce compliance (patient adherence to treatment), and contribute to the formation of suicidal behavior. Other adverse reactions characteristic of standard antipsychotic therapy include sexual dysfunction, cardiovascular disorders, and weight gain. This, as well as the presence of patients resistant to the effects of traditional antipsychotics, necessitated the development of new antipsychotic drugs. An example of such a drug is Seroquel, which has proven its advantages over previous generations of antipsychotics in preclinical and clinical studies. One of its most obvious advantages is the fact that it is only minimally capable of causing the development of dystonia, which determines a low risk of extrapyramidal symptoms. The drug has proven its effectiveness in eliminating both positive (hallucinations, delusions) and negative (apathy, decreased volitional qualities) symptoms of schizophrenia. In terms of effectiveness, Seroquel is not inferior to traditional antipsychotics such as haloperidol and chlorpromazine, while having better tolerability. The key advantages of Seroquel are the absence of the risk of developing extrapyramidal symptoms and hyperprolactinemia.
The incidence of other adverse reactions with the drug is no higher than with previous generations of antipsychotics. The active component of Seroquel, quetiapine, is well absorbed from the digestive tract. The presence of food content in the latter has virtually no effect on bioavailability, which makes it possible to take Seroquel regardless of meals. The drug is not used in pediatric practice. In clinical studies, some side effects occurred more frequently in children and adolescents than in adult patients. The frequency of use of Seroquel is twice a day. The effective dose in elderly patients is usually less than in younger patients. For patients suffering from kidney disease, no dosage adjustment is required. Patients suffering from liver diseases take the drug under regular supervision. At the initial stage of pharmacotherapy, drowsiness usually occurs, which disappears with further use of the drug, and an increase in body weight is also noted. When combining Seroquel with other drugs that affect the central nervous system, extreme caution should be exercised. While taking the drug, you should refrain from drinking alcohol. Patients with suicidal behavior should take the drug under constant medical supervision until remission occurs. Abrupt interruption of the medication course is fraught with an increased risk of suicidal events. If severe drowsiness occurs during the first two weeks of treatment, you should be regularly monitored by a doctor. During treatment, it is recommended to refrain from activities associated with increased attention and concentration (driving a car, working with potentially dangerous mechanisms).
Psychiatry Psychiatry and psychopharmacotherapy named after. P.B. Gannushkina No. 08 2003
The introduction of new antipsychotics into widespread practice has brought to the fore old problems of neuroleptic therapy. One of them is the dose-dependent effect (N.B. Zharkova, 2002; L. Arvanitis et al., 1997; G. Chrouinard et al., 1993), which allows expanding the clinical indications for their use and using these drugs not only for therapy acute schizophrenia, but also for the treatment of sluggish (low-progressive) forms of this disease. A wide range of doses used in the treatment of typical antipsychotics (from ultra-low, for example 0.5 mg/day trifluperazine, to “extraordinary” - more than 80 mg/day haloperidol), as well as the ability to achieve various psychopharmacological effects by changing dosages (from psychostimulant, anxiolytic, antidepressant to antipsychotic) are the main feature of this class of psychotropic drugs, distinguishing them from antidepressants, tranquilizers, nootropics and psychostimulants. It is no coincidence that in American psychiatry the main characteristic of antipsychotics is not the spectrum of their clinical action, but the so-called aminazine coefficients, the concept of which is based on the presence of a dose-dependent effect in these drugs. The possibility of using small and medium doses of antipsychotics for sluggish (low-progressive) schizophrenia has been well studied in Russian psychiatry (S.N. Mosolov et al., 1998; A.B. Smulevich, 1999). Their use for senesto-hypochondriacal, obsessive-phobic, hystero-hypochondriacal and other disorders made it possible not only after a few weeks of therapy to reduce psychopathological symptoms and increase sensitivity to other groups of psychotropic drugs, but also to immediately achieve a nonspecific effect - the occurrence of tranquilization/sedation phenomena. The new atypical antipsychotic seroquel (quetiapine), with a wide range of recommended doses (50–750 mg), widely used in psychiatric clinics, provides a good opportunity to study the dose-dependent effects of atypical antipsychotics. Many clinical studies have confirmed its high effectiveness in the treatment of psychotic conditions in schizophrenia, the ability to reduce positive and negative disorders, have a positive effect on cognitive functions, and good tolerability (Yu.A. Aleksandrovsky et al., 2000; Ph.Meats, 1999). The effective doses of quetiapine recommended in these cases are in the range of 300–750 mg/day. Meanwhile, it was noted that, along with the antipsychotic drug, it clearly exhibits a tranquilo-sedative effect; the positive results of some studies of seroquel in agitated depression, schizophrenia with symptoms of aggression/excitement confirm this (V.V. Kalinin, 2001; J. Bobes et al., 2001; J. Hellewell, J. Goldstein, 1998). At the same time, the issue of distinguishing the anxiolytic and sedative components in the spectrum of its psychopharmacological activity was not considered. Meanwhile, these two effects, one of which (anxiolytic) is assessed as therapeutic, and the other (sedative) as a side effect, reflect the discrepancy between the dichotomous concepts of therapeutic-side and desirable-undesirable. Thus, the sedative effect can be regarded as desirable in the treatment of severe psychotic states with symptoms of agitation, agitated depression and considered as a side effect during long-term maintenance neuroleptic therapy or in the treatment of low-progressive schizophrenia and borderline mental disorders. The purpose of this study was to study the effectiveness/tolerability and impact on cognitive function of the atypical antipsychotic seroquel (quetiapine) in patients with low-grade schizophrenia with a predominance of generalized anxiety. Patients with sluggish neurosis-like schizophrenia were selected for the study, whose condition was determined by generalized anxiety symptoms (GAD) within the framework of senesto-hypochondriacal disorders or anticipatory anxiety in agoraphobia. All patients were undergoing inpatient and outpatient treatment in the Department of Borderline Psychiatry of the State Scientific Center for SSP named after. V.P. Serbsky on the basis of PKB No. 12. Patients with severe somatic and neurological pathologies were excluded from the study. The age of patients was limited to 18–45 years to exclude negative effects on cognitive function due to advanced age. The simultaneous use of other psychotropic drugs (neuroleptics, antidepressants, anxiolytics, hypnotics) was excluded. If extrapyramidal symptoms occurred, anticholinergic drugs were prescribed. Research methods included clinical and psychopathological examination, as well as assessment of the dynamics of disease severity and overall effectiveness of therapy on the CGI scale, positive, negative and general pathological disorders on the PANSS scale, anxiety disorders on the HAM-A scale, and side symptoms on the UKU scale. All patients were discontinued from all psychotropic medications before the start of the study. The wash-out period depended on the half-life of the specific drug being discontinued. Patients examined before starting Seroquel therapy (background) began taking the drug at a dose of 25 mg/day at night for one week, after which a second examination was carried out. Subsequently, in the absence of a therapeutic effect, the dose of the drug was increased by 25-50 mg (over 1-2 days) until positive treatment results were achieved - the third examination (dosage regimen - 2 times a day). 2 months after this, under the condition of monotherapy with stable doses of the drug, the last (fourth) examination was carried out. The study design is presented in Table. 1
.
Research results
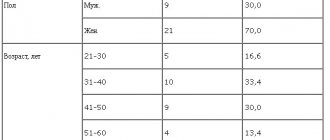
The study included 20 patients who had suffered from indolent neurosis-like schizophrenia for 3–10 years (average 5.6 years);
their average age was 34.3±9.1 years. Generalized anxiety in 13 of them was observed within the framework of the senesto-hypochondriacal state, in 7 – anxiety of anticipation in agoraphobia. 19 patients completed the study completely. One patient with a senestohypochondriacal condition refused to take seroquel at a dose of 25 mg on the 5th day of therapy due to increased anxiety, the appearance of tachycardia, and restlessness. These symptoms decreased when the drug was discontinued. The distribution of patients according to the level of doses of seroquel received by the end of the study is presented in table.
2 .
As follows from table. 2
, more than 60% of patients took Seroquel in doses of 50–75 mg/day, most often in a dose of 75 mg/day (36.8%).
Only in 21.1% of patients the drug dose reached 100 mg/day and in 10.5% – 300 mg/day. Only one patient took 25 mg/day of Seroquel. The severity of the disease on the CGI-S scale before the start of therapy in 83.3% of patients was characterized as moderate, and in 16.7% as significant, while by the end of treatment the condition of the majority of patients (83.3%) was assessed as borderline or mild. Only in 16.7% of patients the disease corresponded to “moderate severity”. The overall effectiveness of the treatment, assessed on the CGI-I scale, is presented in Table.
3 . At the end of the study, high rates of treatment success were noted. This was confirmed by the fact that all patients showed an improvement of varying degrees of severity.
Thus, “pronounced” and “moderate” positive effects were observed in 84.2%, and “minimal” – in 15.8% of patients. No positive dynamics during treatment or minimal deterioration was noted in any patient. As the results of the study showed, the degree of effectiveness of therapy did not correlate with the characteristics of the clinical condition of patients with low-grade schizophrenia and did not depend on the psychopathological structure of their condition ( Table 4
). Complete remission was achieved in 50% of patients with senestohypochondriacal syndrome and 42.9% with anticipatory anxiety in agoraphobia. Partial remission was observed in 33.3% of patients with senestohypochondriacal syndrome and in 42.9% with anticipatory anxiety in agoraphobia, and minimal effect was observed in 16.7 and 14.2% of cases, respectively.
Therapeutic dynamics of the severity of psychopathological symptoms was carried out using the PANSS scale ( Table 5
).
A statistically significant reduction (p=0.0001) was observed when assessing the total score of this scale (by 17.3%). The reduction was subject to both general pathological (by 21.7%) (p = 0.0001) (mainly due to a decrease in the level of anxiety, somatic concern, tension) and negative (by 20.3%) (p = 0.0008 ) symptoms. The dynamics on the scale of positive syndromes did not reach the level of statistical significance due to the absence of acute psychotic disorders in patients with sluggish schizophrenia - delusions, hallucinations, ideas of grandeur, etc. Their existing disorders, classified as positive on the PANSS scale, consisted of disturbances in thinking in the form of reasoning, slipping, and thoroughness. Detection of the tranquilizing effect of the study drug was possible due to compliance with the inclusion criteria (the predominance of generalized anxiety in the clinical condition of patients) and the use of the appropriate assessment tool (HAM-A scale). In all patients ( Table 6
) there was a reduction in anxiety symptoms (from 17.30 to 9.66 points).
A tendency towards its decrease was observed already from the first week of therapy at all, even small (25 mg), doses of the drug, but significant changes in this indicator were noted only towards the end of therapy and amounted to 27% at doses of 25–100 mg and 20% at doses of 150 –300 mg (see figure).
A decrease in the level of anxiety in patients with GAD as part of low-grade schizophrenia indicated a clear anxiolytic component of the drug’s action, which manifested itself already in the first week of therapy. At the same time, there was a tendency to a slight decrease in the severity of the anxiolytic effect with increasing dosages of the drug. Features of the tranquilizing component of seroquel, depending on its dose, were discovered when assessing the effect of therapy on cognitive functions. The results of the psychophysiological study are presented in table. 7
.
As can be seen from table. 7
, with the use of seroquel in the dose range of 25–100 mg, a clear optimization was observed when assessing attention functions.
When performing the “correction test” test, an improvement in the volume and productivity of attention was noted (an increase in the number of correct answers and a reduction in the proportion of erroneous answers). The positive dynamics were also different in relation to the reaction time indicator, which was manifested in a reduction in the latent period of the sensorimotor reaction of choice. The improvement in memory functions turned out to be statistically unreliable - an increase in the total number of answers and a decrease in the proportion of erroneously reproduced answers. Such a dissociation between the restoration of attention functions and the lack of a clear improvement in memory indicators is typical for tranquilizers belonging to the type of selective anxiolytics, a characteristic feature of which is the presence of an anxiolytic effect in the absence of a sedative component of their action. Thus, the tranquilizing effect of small doses of quetiapine reflected the properties of selective anxiolytics. The positive effect of Seroquel on attention functions described above is of independent significance. The ability to selectively respond to significant environmental circumstances, filter them out and not react to distracting or irrelevant factors is the leading ability of a person’s target behavior, closely related to the processes of his adaptation. Thus, restoration of attention functions when using Seroquel in doses of 25–100 mg in patients with low-grade schizophrenia can be considered as one of the fundamental cognitive processes that implement the adaptive activity of such patients. The effect on basic cognitive functions of Seroquel monotherapy in doses of 150–300 mg turned out to be different. A vectorial decrease in productivity and memory and attention, a decrease in reaction time reflected the appearance of a tranquilosedative component in the spectrum of psychotropic activity of the drug. This dose-dependent two-stage nature of the tranquilizing effect of seroquel, characterizing it in small doses as a selective anxiolytic, and in medium doses as a sedative anxiolytic, is the main feature of the spectrum of psychopharmacological activity of the drug. The number/range of side effects when using Seroquel also turned out to be dose-dependent ( Table 8
).
In table the number of side effects increases more than 2 times when the dosage of the drug increases from 25–100 to 150–300 mg (from 1.3 to 2.8 per patient). The spectrum of side effects of the drug was characterized mainly by effects affecting the mental sphere (see Table 8
). Moreover, if during therapy with small doses (25–100 mg) the adverse events were increased anxiety and worsening sleep, which reflected the activating effect of the drug, then when the dose was increased to 150–300 mg, patients more often complained of drowsiness, asthenia, increased sleep duration, which characterize its sedative property. The second place in frequency of occurrence was occupied by autonomic disorders: orthostatic disorders, dry mouth, nausea, tachycardia, which were characterized by mild severity, went away on their own and did not depend on the dose level of the drug. Less frequently, and only with therapy with small doses of the drug, so-called other side effects occurred, among which headaches predominated. Neurological (extrapyramidal) side effects were the rarest and did not depend on the dose of seroquel. They were represented by two cases of short-term small-scale tremor that did not require additional anticholinergic therapy due to self-reduction. Thus, a study of the use of seroquel in low-grade schizophrenia with a predominance of GAD within the framework of senesto-hypochondriacal states and anxiety of expectations in agoraphobia showed the effectiveness of its dosage from 25 to 300 mg. However, most often (in more than 60% of patients) positive therapeutic results were achieved with treatment at doses of 75–100 mg/day. An increase in the seroquel dose to 300 mg was required in 10.5% of cases. Positive therapeutic dynamics were achieved due to the reduction of general psychopathological and negative symptoms, as well as anxiety disorders, which indicated a clear anxiolytic effect of the drug. The anxiolytic effect was observed in the early stages of therapy (week 1) across the entire dose range of the drug. The conducted psychophysiological study revealed a dose-dependent two-stage pattern in the anxiolytic effect of seroquel. Improvement in cognitive functions (attention) when using the drug in doses of 25–100 mg reflected its properties as a selective anxiolytic, while increasing its dosage to 150–300 mg indicated the appearance, along with a tranquilizing sedative component, in the spectrum of its psychopharmacological activity. This was also evidenced by the analysis of dose-dependent side effects of the drug. During therapy with doses of 25–100 mg, activation phenomena occurred, and with 150–300 mg, moderate sedation occurred. The incidence of other types of side effects (neurological, autonomic) did not depend on the dose level of the drug and did not require drug correction (including the prescription of anticholinergic drugs). The study allows us to conclude that it is advisable to use Seroquel in patients with low-grade schizophrenia with a predominance of anxiety disorders and to optimize the method of prescribing the drug to such patients. Seroquel doses in the range of 75–100 mg in this group of patients at the initial stage of treatment are an adequate choice, reducing the time to achieve the effectiveness of therapy.
SIDE EFFECTS OF TRANQUILIZERS
(ANTI ANXIETY DRUGS).
Development of addiction and formation of drug dependence
Signs: the first sign of addiction to the drug is the desire to increase the dose of the drug used, since the previous amount of the drug ceases to give the desired effect and no longer relieves unpleasant symptoms. Subsequently, the dependence manifests itself in the inability to “get off” the drug: when trying to stop the drug, a “withdrawal syndrome” occurs: anxiety, low mood, irritability, heaviness in the head, insomnia, severe weakness, loss of appetite, tremors in the hands, palpitations, increased blood pressure . Leg cramps and even grand mal seizures and daytime urinary incontinence may occur.
Drugs that cause addiction and dependence:
Most often: Relanium (Seduxen, Sibazon), lorazepam (Lorafen), alprazolam
Reliably less common: Elenium, clonazepam, tazepam (nozepam)
What to do if you become addicted to the drug? It is very difficult to stop taking a tranquilizer on your own if you have developed an addiction due to the duration of the “withdrawal syndrome” (about three weeks), the gradual increase in symptoms by the end of the first week of abstinence, and the possible development of dangerous complications (epileptic seizures). It is most advisable to reduce the dose of the drug very slowly under the supervision of a doctor who, in addition to observation, will be able to select therapy aimed at accelerating the elimination of the drug from the body and relieving unpleasant and painful symptoms.
Attention! Signs of the formation of drug dependence appear within 1 - 1.5 months after starting to take the above drugs (especially Relanium, Lorafen and Alprazolam). Most often, dependence on tranquilizers occurs during self-medication, so it is strongly NOT recommended to prescribe these drugs to yourself without the participation of a doctor.
Deterioration of memory and attention, impaired coordination of movements, increased effects of alcohol
Signs: These side effects are united by the concept of “behavioral toxicity” of tranquilizers. A person feels less efficient, it is difficult for him to concentrate for a long time, it is difficult for him to think quickly and find answers in a conversation, he may immediately forget the facts that are told to him. There is a feeling of insufficient “inclusion” in the situation. There may be motor clumsiness and lack of coordination of movements.
Drugs that most often cause such symptoms: diazepam, clonazepam, lorazepam, nitrazepam, phenazepam, elenium (Librium), estazolam
Attention! Alcohol intake is prohibited during the treatment period. You should refrain from activities related to operating machinery and vehicles.
Excessive sedation
Signs: drowsiness, lethargy, difficulty waking up in the morning.
Drugs that most often cause these symptoms: flunitrazepam (Rohypnol), nitrazepam (radedorm), clonazepam, phenazepam, lorazepam, diazepam (Relanium, Seduxen)
Muscle relaxation
Signs: general weakness, or weakness in certain muscle groups (for example, in the arms), relaxation in the body, reluctance to move again.
Drugs that most often cause these symptoms: diazepam (Relanium, Seduxen), clonazepam, phenazepam, nitrazepam, lorazepam
Paradoxical reactions
Signs: instead of calming and relieving anxiety, opposite reactions to taking a tranquilizer may occur: increased anxiety, motor restlessness, fussiness, irritability and even aggression. Such reactions are rare and depend on the individual characteristics of the patient’s body.
“Paradoxical” reactions have not yet found definitive confirmation of their connection with the use of certain tranquilizers. However, there is evidence that triazolam, for example, quite often contributes to the appearance of pronounced aggressive behavior. In isolated cases, paradoxical reactions in the form of anxiety and sleep disturbances were noted in patients taking buspirone.
Drugs that do not cause excessive sedation, muscle relaxation and impairment of memory and attention: oxazepam (tazepam, nozepam), grandaxin, stresam, buspirone, atarax, afobazole, mezapam (rudotel), clorazepate.
If you are taking mood stabilizers (mood correctors)
Mood correctors
– drugs that have the ability to influence both pathologically depressed and pathologically elevated mood. The ability to regulate mood is manifested in the elimination of severe affective disorders, and then in the stabilization of mood at a certain average level. Thus, the main indication for prescribing mood stabilizers is the presence of depressive and manic attacks that recur quite often.
Most mood correctors (except lithium) are also anticonvulsants used in the treatment of epilepsy.
In addition, mood stabilizers are successfully used in the treatment of:
- personality disorders accompanied by explosiveness, conflict, irritability, aggression
— depression in patients with alcoholism
- migraine
Normotimics include:
- lithium salts (preparations sedalit, micalit, litosan, contemnol, quilonum retard)
- valproic acid (drugs Depakine, Konvulex, Encorate, Apilepsin, Konvulsofin, Dipromal, Orphyril, Everiden)
- carbamazepine (synonyms: finlepsin, tegretol, actinerval, gene-karpaz, zagretol, zeptol, carbadak, carbalepsin, carbapin, karbasan, carbatol, carzepin-200, mazepin, novo-carbamaz, stazepin, storilat, timonil, finzepin, epial)
SIDE EFFECTS OF NORMOTIMICS.
Side effects of lithium drugs (sedalite, micalite, litosan, etc.)
At the initial stage of preventive therapy with lithium salts, mild side effects may appear in the form of increased fatigue, disorders of the digestive system (nausea, vomiting, diarrhea), and occasional mild hand tremors. At acceptable concentrations of lithium in the blood (within 0.5 - 0.8 mEq/L), these phenomena do not require a dose reduction and usually disappear as the body adapts to the drug.
With a relative duration of treatment (over several months and years), the following may appear:
- diffuse enlargement of the thyroid gland
- noticeable weight gain
- minor swelling
- temporary deterioration in vision clarity.
In these cases, it is sometimes necessary to slightly reduce the dose or switch from using a long-acting (long-acting) drug to taking short-acting drugs in the same dose 2-3 times a day.
The main complication that can occur with long-term use of lithium drugs is intoxication with lithium salts.
Early signs of lithium overdose: increased thirst and trembling fingers. Then lethargy, weakness, and drowsiness appear. Then vomiting and diarrhea occur, swelling increases, speech difficulties and heart rhythm disturbances appear.
At the first signs of intoxication, you must immediately stop taking the drug and consult a psychiatrist, who will prescribe treatment aimed at accelerating the elimination of lithium from the body and relieving symptoms of intoxication.
Provoking factors that increase the concentration of lithium in the blood: a diet with limited salt and liquid, combination with indomethacin, some antibiotics (ampicillin, tetracycline)
Attention! Treatment with lithium preparations is carried out with regular monitoring of the concentration of lithium in the blood plasma:
- in the acute period (treatment aimed at “breaking off” a painful attack): the concentration of lithium in the blood is monitored daily, and it should not exceed 1.2 - 1.4 meq/l
- selection of a daily dose for prophylactic use (treatment is aimed at preventing repeated attacks of depression or manic states) requires determining the concentration of lithium in the blood, first once a week during the first month, then 1 - 2 times a month, after 7 months of therapy - once at 3 – 4 months. The lithium concentration that provides a preventive effect should be in the range of 0.5 – 0.8 mEq/L
Side effects of valproic acid drugs (convulex, depakine, encorate, etc.)
The most common side effects of valproic acid therapy are gastrointestinal disorders: nausea, diarrhea, loss of appetite.
Possible excessive sedative effect in the form of drowsiness, slowing down of thought processes.
Also possible: tremor (shaking of hands), loss of coordination of movements.
When using long-acting drugs used once a day (for example, Depakine Chrono), side effects occur more often, it is possible that appetite may increase rather than decrease, and hair loss is sometimes observed.
To prevent these phenomena, it is advisable to combine valproic acid with a daily intake of multivitamins with a set of microelements, including, in particular, selenium and zinc.
Side effects of carbamazepine (finlepsin, tegretol)
When carrying out carbamazepine therapy, side effects are expressed in headaches, dizziness, loss of coordination of movements, drowsiness, dermatitis or skin itching, sometimes double vision, blurred vision.
As with other mood stabilizers, side effects such as nausea and vomiting are possible.
However, in most cases, carbamazepine is well tolerated, even with long-term use.
If you take nootropics (meals that improve nutrition and brain function)
Nootropics
– medications that stimulate mental activity, improve memory, and accelerate learning processes.
Application: decreased general activity, asthenic conditions of various origins, brain lesions (vascular, traumatic, alcoholic, infectious), conditions after strokes, coma, dementia, in pediatric practice: with intellectual disability, developmental delay, attention deficit hyperactivity disorder (ADHD) ), tics, enuresis.
Noothorps are always used in the treatment of alcoholism.
Effects of nootropics (present in different drugs in different amounts):
— Psychostimulating (increasing the activity of the sphere of impulses) – used in states of decreased activity, inactivity and apathy, intellectual inhibition
— Antiasthenic (reduction of weakness, increased physical and mental exhaustion)
— Increasing the level of wakefulness of consciousness - used in states of depressed or darkened consciousness
— Adaptogenic – increasing the resistance of the body and psyche to various harmful environmental factors, including intoxications
— Nootropic (strengthening the functions of thinking, memory)
— Antiepileptic (for some drugs)
— Antiparkinsonian (used not only for Parkinson’s disease, but also to relieve the unpleasant side effects of antipsychotic therapy - see above)
— Vegetotropic (stabilization of the autonomic nervous system)
Table of synonyms for nootropic drugs.
| International name of the drug | Names of this drug that are found in pharmacies (the most commonly found dosage forms in pharmacy chains are highlighted) |
| Drugs with a predominant stimulating, activating effect (cannot be taken at night as it may impair sleep) | |
| Meclofenoxate | Acefen, Centrophenoxine, Cerutil |
| Phenylpiracetam | Fenotropil |
| Ethylthiobenzimidazole | Bemitil |
| Pyritinol | Encephabol, Pyriditol, Cerebol, Enerball |
| Piracetam | Nootropil, Piracetam, Lucetam, Memotropil, Oykamid, Cerebril, Stamin, Escotropil, Piratropil |
| Piracetam + cinnarizine | Fezam, Combitropil, NooKam, Omaron, Piracezin |
| Piracetam + Vinpocetine | Vinpotropil |
| Deanol aceglumate | Demanol, Noocleril |
| Gamma-aminobutyric acid | Aminalon |
| Glutamic acid | L-Glutamine, Calcium glutamate, Epilapton, Acidogen, Glutan |
| Hexobendine+Etamivan+Etophylline | Instenon |
| Ginkgo biloba | Tanakan, Bilobil, Gikoba, Ginkyo, Memoplant |
| Preparations with balanced action | |
| Methionyl-glutamyl-histidyl-phenylalanyl-prolyl-glycyl-proline | Semax |
| Cerebrolysin | Cerebrolysin |
| Choline alphoscerate | Gliatilin |
| Drugs with a predominant sedative, calming effect | |
| Ethylmethylhydroxypyridine succinate | Mexidol |
| Aminophenylbutyric acid | Phenibut |
| Nicotinoyl gamma-aminobutyric acid | Picamilon |
| Hopantenic acid | Pantogam |
| Sodium hydroxybutyrate | Sodium hydroxybutyrate |
| Glycine | Glycine |
SIDE EFFECTS OF NOOTROPICS
Nootropics are low-toxic drugs and are usually well tolerated by patients.
Side effects may include sleep disturbances and increased irritability. Such effects are inherent in nootropics with a predominant stimulating effect. These include (in descending order of stimulating effect): acephen, phenotropil, bemitil, encephabol, nootropil (piracetam), demanol, aminalon.
On the contrary, drugs with a predominance of a mild sedative (calming) effect do not cause increased irritability, anxiety and sleep disturbances, and even relieve these unpleasant symptoms. Nootropics with a predominant calming effect include phenibut, mexidol, picamilon, pantogam.
Other side effects of nootropics (occur quite rarely, are unstable and pass quickly): headache, nausea, stool disorders, fluctuations in blood pressure