Treatment of intracranial hypertension
Intracranial pressure cannot be ignored; physical discomfort is not as dangerous as the processes occurring inside the brain.
Constant disruption of the outflow of cerebrospinal fluid and, as a consequence, compression of certain areas of the brain over time can cause tissue necrosis and damage to stem structures, as well as the development of epilepsy, blindness, stroke and other equally serious diseases. Therapy for the treatment of hypertension is always comprehensive, it includes following a diet with limited intake of salt and fluid, and taking antibacterial drugs. Acupuncture, physiotherapeutic procedures, exercise therapy, and manual techniques provide good results. If necessary, surgical removal of tumor-like formations and similar methods are carried out.
In the absence of hematomas, tumors, aneurysms and other serious pathologies, it is advisable to add diuretics to the main treatment. With the help of diuretics, excess fluid is removed through the kidneys, the level of cerebrospinal fluid decreases and the pressure gradually returns to normal.
As a rule, therapy is aimed at eliminating the causes of increased, compared to normal, pressure, and not at reducing it as such. With the right approach, the condition normalizes spontaneously, the pressure equalizes.
Emergency reduction of intracranial pressure with the help of medications is indicated when there is a threat of severe complications; medical care is provided only in an inpatient setting.
It should be remembered that nootropics and drugs whose action is aimed at improving blood circulation in the brain are ineffective with high intracranial pressure, so their use is inappropriate.
In addition to basic treatment methods, you can use traditional medicine recipes, but only after agreement with your doctor.
Physiological norm and determination of intracranial pressure
The human skull is a cavity in which the brain is located. To protect it from injury, as well as to maintain its normal operation, there are sections filled with liquid. First of all, the liquid fraction is represented by blood, which is located in the vessels. There is also cerebrospinal fluid (cerebrospinal fluid) present here. It is synthesized in special choroid plexuses and enters the skull through the spinal canal, then is located in the ventricles of the brain and is removed through the venous sinuses. This fluid is necessary for the transport of oxygen and nutrients that are used by brain cells to maintain performance.
Intracranial pressure is a complex value that consists of several factors:
- brain pressure (normally it occupies no more than 85% of the skull space);
- blood - up to 8%;
- spinal cerebrospinal fluid - up to 7%.
Blood and cerebrospinal fluid are in constant motion. If blood circulates through the vascular bed, then spinal fluid moves through the ventricles of the brain and along the spinal canal. These fractions are continuously synthesized, enter the cranium and move further along the vascular bed. When they are in the skull, they put pressure on the inside of the blood vessels and ventricles of the brain. For this reason, intracranial pressure is present in every person, and its value can change every minute. An increase or decrease in this indicator may indicate both pathology and normal physiological processes in the human body.
Causes of the disease
The internal cavity of the skull is a closed space. If cerebrospinal fluid accumulates excessively in this area, there is nowhere for the tissue to move. Areas of the brain are compressed, displaced relative to their original position, and blood vessels are compressed, which leads to critical changes in living fibers and cessation of normal blood flow. Internal pressure is considered normal from 7.5 to 15 mmHg. Exceeding the specified values by up to 30 mm RS can lead to death.
The following factors lead to the development of ICH:
- congenital developmental anomalies;
- extensive infection, previous meningitis;
- tumor formations in the brain;
- stroke;
- delay in normal fluid outflow (hydrocephalus);
- penetration of the encephalitis virus into tissue;
- post-traumatic hematomas;
- internal hemorrhages;
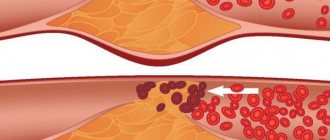
- high level of blood clotting;
- diseases in the cervical spine;
- large body weight;
- intoxication with alcohol or medications.
Causes of blood pressure abnormalities
In the CIS countries, increased intracranial pressure is a common diagnosis. It is prescribed for various disorders of the central nervous system in adults and children, and a simple set of therapeutic procedures allows you to quickly normalize the condition and maintain it in the future. However, changes in ICP levels are actually a symptom of a number of dangerous diseases that cannot be treated at home. When making a diagnosis, it is important to pay attention to the patient’s complaints, collect a complete picture and determine whether the pressure inside the skull is really pathologically reduced or increased and threatens human health. In most cases, if ICP is indeed elevated, the patient has a number of additional clinical signs that can be used to identify serious disorders of nervous activity.
Increased intracranial pressure
Increased intracranial pressure is a dangerous phenomenon. It accompanies diseases that threaten the patient’s life. These include:
- inflammatory diseases of the membranes of the brain, including those of infectious origin (meningitis);
- serious poisoning with toxins - in this case there is an increase in the amount of blood in the vessels of the brain and its stagnation;
- traumatic injuries of brain tissue (closed craniocerebral injuries);
- various neoplasms in the cranial cavity;
- hematomas located between the membranes of the brain;
- hydrocephalus is a dangerous disease characterized by impaired outflow of spinal fluid and its accumulation in the ventricles of the brain;
- severe metabolic disorders (advanced forms of diabetes).
In children under the age of 10-11 years, any signs of intracranial hypertension are often associated with birth injuries. Indeed, this factor in history can provoke cerebral hypoxia and various neurological disorders. However, it is important to exclude the possibility of developing hydrocephalus - this disease manifests itself at an early age and is characterized by a rapid increase in the volume of the head. Since the anatomical norm may differ in children (a large head is not a cause for concern), the diagnosis is made based on frequent measurements of head circumference and analysis of the rate of its growth. Signs of increased intracranial pressure in adults are a reason to undergo an examination and exclude the possibility of neoplasms in the cranial cavity.
Reduced pressure
Decreased intracranial pressure is a less dangerous condition. This indicator decreases in certain situations that can be corrected by a set of procedures or by taking medications. No surgical intervention will be required. The reasons for its decrease include:
- production of spinal fluid in insufficient quantities or acceleration of its reabsorption into the blood;
- increasing the permeability of the barrier, which ensures the exchange of fluid between the cells of the central nervous system and the bloodstream;
- decreased tone of blood vessels;
- diseases of the spinal column, especially the cervical region affects the indicator of intracranial pressure;
- any conditions that are accompanied by pathological dehydration of the body: poisoning, taking diuretics, allergic reactions and others.
In some diseases, there is a decrease in the rate of blood circulation through the vessels of the brain. They can also be a consequence of birth injuries, vascular pathologies, and congenital abnormalities of the brain structure. If not treated promptly, this condition can also cause dangerous complications.
Symptoms in adults
Intracranial hypertension manifests itself through a sequence of symptoms.
This is a progressive deterioration of neurological status not associated with other pathology. Men and women experience general cerebral symptoms - nausea, vomiting and headache. In severe cases, there may be impairment of consciousness from stupor to coma. There is a disturbance in the movement of the eyeballs in the form of strabismus, dilated pupils and a decreased reaction to light.
The presence of one of the listed symptoms does not indicate increased intracranial pressure. However, this is a reason for a more detailed examination. It is necessary to evaluate the clinical picture as a whole, and also take into account the results of additional diagnostic methods.
Signs of pathology
Changes in intracranial pressure affect the general condition of the patient. This is often preceded by injuries or blows to the head, complications during childbirth, and diseases of the meninges. In this case, the patient cannot lead a normal lifestyle, and the symptoms of increased or decreased ICP are not relieved by taking medications. Such patients are treated in a hospital setting. It is also impossible not to notice pathological changes in this indicator in children. In addition, in the absence of a reason, the pressure cannot increase or decrease and stop at a critical level for the child - serious reasons are required for this.
The physiological basis of painful sensations with an increase or decrease in pressure, as well as other symptoms, is an insufficient supply of blood to the brain and various disorders of its circulation. If fluid is retained in the vessels and cerebral ventricles, the tissues are under constant pressure, which can provoke gradual necrosis (death) of cells. Hypoxia (insufficient oxygen supply) and nutrient deficiency are also observed - this causes disturbances in brain activity or loss of reflexes, depending on the location of the damaged area of brain tissue.
With high blood pressure
High blood pressure is manifested by a pronounced set of symptoms that affect all vital processes. They may be combined with additional clinical signs characteristic of a particular disease. The symptom complex indicating increased ICP includes:
- painful sensations in the head, which are pressing in nature and spread to all areas, often occur immediately after waking up and intensify during the day;
- sleep disorders, insomnia;
- ineffectiveness of standard drugs against headaches;
- nausea and vomiting, decreased heart rate;
- a sharp decrease in vision, inability to focus on small objects for a long time, deterioration of memory and concentration.
For headaches that occur as a result of serious pathologies of intracranial pressure, the patient remains in bed. During physical activity, attacks of dizziness, loss of consciousness, and memory loss may occur. Also, peripheral vision disorders periodically appear, the appearance of dark spots and “floaters” in the field of vision is a consequence of permanent fluid pressure on the optic nerve. With exacerbation, the situation worsens, normal reflex responses to stimuli may partially disappear.
In children, behavioral problems and hyperactivity are often associated with increased intracranial pressure. However, these diagnoses may not be related. Increased ICP in infants is indicated by symptoms such as bulging fontanel, rapid increase in head circumference, and divergence of the bones of the skull. Another alarming symptom is the overgrowth of the fontanel too slowly. If these signs appear in combination with general apathy or excitability, poor sleep, lack of innate reflexes, this may indicate pathological fluid pressure inside the skull.
At low pressure
Reduced intracranial pressure can also be determined by clinical signs. The symptoms are not as pronounced as when this indicator increases, but also affect the patient’s well-being and performance. If the pressure inside the skull is not normal, this leads to the following consequences:
- headaches, which are especially worse when raising the head;
- frequent mood swings, lethargy, apathy, irritability;
- simultaneous decrease in blood pressure if the syndrome is caused by a general lack of fluid in the body;
- headaches, dizziness, fainting may occur after minor physical exertion;
- decreased visual acuity, appearance of dark spots before the eyes;
- nausea, abdominal pain;
- Possible pain in the heart area that spreads to the chest.
First aid for a sharp decrease in intracranial pressure is to take the correct position. Lying on your back with your head down makes the outflow of fluid difficult, so the pressure is partially restored. This factor may also have diagnostic significance - when you raise your head and sit or stand, the pain intensifies, and lying on your back it decreases slightly.
Measurement principles
The principles of measuring intracranial pressure differ significantly from measuring blood pressure. To date, there are no devices for quickly measuring ICP. Since the structural elements located in the cranium occupy a certain volume of the cranial cavity, determined by its parameters, therefore it cannot change. Due to the fact that the volume of the cranial cavity cannot be changed, the ratio of brain structures is constant.
Measuring intracranial pressure is difficult because there are not enough indirect parameters by which to determine the pressure in the cranium. Depending on the diagnosis, age and functional state of the body, visual examination methods or modern research methods are used to diagnose patients, which make it possible to use equipment to determine the reasons that provoked changes in brain pressure. Invasive techniques through surgery are used to establish clear pressure values.
Diagnostic methods
It is impossible to measure intracranial pressure at home. The only thing a patient can do to help himself is to detect the symptoms in time and consult a doctor for a detailed diagnosis. It is worth understanding that the procedures for measuring ICP are complex and require special equipment and sufficiently qualified medical personnel. All these conditions are available at the Clinical Institute of the Brain, which specializes in the diagnosis and treatment of pathologies of nervous activity.
The only way to accurately determine intracranial pressure is to puncture the cerebrospinal fluid. The technique is invasive and is used only in complex cases. To do this, it is necessary to make a puncture in the lumbar region (into the spinal cord canal) or the ventricles of the brain. The cerebrospinal fluid that is constantly circulating in these spaces will begin to flow out, and its pressure can be measured. The value is measured in mm of water column, and its norm is from 60 to 200 mm. These data are indicative if the patient is in a supine position.
There are also additional diagnostic techniques that allow you to assess the condition of the brain, its ventricles and vascular bed without invasive intervention. These include:
- Ultrasound of the brain - the procedure is performed only for children who have not had fusion of the fontanelle, and in adults it is impossible due to the density of the bones of the skull;
- CT or MRI of the brain - analysis can be done at any age, while the data is quite informative and allows you to obtain a complete three-dimensional image of any area under study;
- echoencephalography is a type of ultrasound examination that can be used to determine the degree of filling and pulsation of the cerebral arteries.
It is impossible to diagnose increased intracranial pressure based on the clinical picture alone. However, all this data must be provided to the doctor during the initial examination. Based on them, specialists from the Clinical Institute of the Brain will prescribe all the necessary diagnostic stages, which will allow a full assessment of the patient’s condition.
Possible complications
If measures are not taken in time and the blood pressure level is not normalized, as the disease progresses, the symptoms will only worsen, causing serious complications. These include:
- damage to the cerebellum with partial or complete loss of coordination in space;
- disorders of speech and mental functions;
- arrhythmia, tachycardia, surges in blood pressure due to compression of the brain stem;
- loss of vision;
- the appearance of epileptic convulsive seizures, during which the patient’s breathing is depressed, the risk of cerebral edema and transition to a coma increases;
- paralysis.
Now it has become clear why intracranial pressure that is not subject to adequate treatment is dangerous. The benign form of intracranial hypertension occurs much more easily and without dangerous consequences; it is more often observed in women aged 20–40 years, taking oral contraceptives and being obese. The disease manifests itself as unsteadiness of gait, dizziness, morning sickness and signs of migraine.
When hormonal medications are discontinued and lifestyle is adjusted, it happens that the symptoms of the pathology may go away on their own. But it’s better not to hope that in a particular case the problem is caused by a benign form of hypertension; it’s worth starting to fight it right away.
Treatment and prognosis
Therapeutic measures are prescribed based on diagnostic results. First of all, it is important to get rid of the cause that provokes excessive fluid pressure on the skull. If this phenomenon is caused by traumatic brain injury, the patient is advised to rest completely, take gentle nutrition, and take anti-inflammatory drugs. In some cases, surgical intervention is necessary (in the presence of hematomas between the membranes of the brain, as well as in the presence of injuries that require surgical treatment). Surgery is also prescribed when various tumors are detected in brain tissue that is prone to rapid growth.
A separate set of measures is carried out when diagnosing hydrofecal in a child. To remove excess fluid, a shunt is installed, through which it flows into the abdominal cavity, and the pressure is normalized. The operation is repeated as the child grows, and the patient is constantly monitored. In some children, the need for artificial fluid removal gradually disappears.
Drug therapy for ICP pathologies is secondary. However, drugs are prescribed to eliminate symptoms and make the patient feel better. The following medications may be helpful:
- hormonal anti-inflammatory drugs;
- neuroprotectors and substances for stimulating blood circulation in the brain - the effectiveness of this group has not been proven, despite its widespread use;
- loop diuretics (diuretics) - medications that stimulate the excretion of excess fluid;
- osmodiuretics - including reducing the production of cerebrospinal fluid.
The Clinical Brain Institute specializes in the diagnosis and treatment of diseases of the central nervous system. Increased intracranial pressure is not a separate disease, but a symptom that indicates a number of pathologies. Experienced specialists will accurately determine the cause of such a violation, as well as its severity and possible consequences. It is worth understanding that only timely seeking medical help can guarantee successful treatment and a return to your normal lifestyle without headaches.
What to do if the above symptoms appear?
If there are signs of the disease, you should consult a neurologist. To treat a pathological condition, it is necessary to find out its exact cause. That is why the doctor prescribes a set of diagnostic procedures:
- Fundus examination. Allows you to identify swelling of the optic nerve - one of the main signs of intracranial hypertension.
- Echoencephalography is an ultrasound procedure for examining brain tissue. Such diagnostics will help confirm or refute the presence of a tumor, cyst, hemorrhage, or other pathological changes in tissue structure. This diagnostic method does not require preparation, changes in daily routine or nutrition.
- X-ray of the skull. Prescribed for suspected birth defects, fractures or bone displacement. This method also identifies possible tumors that are causing compression.
- CT or MRI of the head. The most accurate and informative diagnostic methods. They allow you to thoroughly assess the condition of bones, soft tissues, and blood vessels. As a rule, the doctor prescribes such a diagnosis after echoencephalography, if it shows the presence of a pathological process.
- Ultrasound of the vessels supplying the brain. It is necessary to identify possible anomalies, tortuosities, and thromboses.
- Angiography. Allows you to visualize large and small vessels and detect areas of affected arteries.
The purpose of the above procedures is to determine the cause of the malaise. Based on the examination results, the specialist prescribes additional diagnostics or decides on treatment.