What are basophils, functions
In the KLA, the indicator is present in the leukogram. Basophils are blood cells from the group of granulocytes. Produced by the bone marrow, they are a type of white blood cell. Viability is maintained from seven to twelve days.
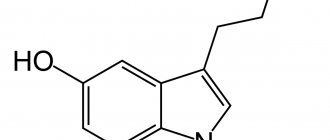
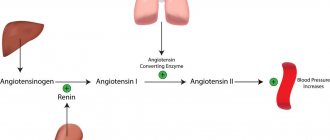
Establishing the level of basophils helps to identify pathological inflammation or the presence of allergic reactions. The resulting focus of inflammation attracts basophils as part of other leukocytes. They are then transformed into heparinocytes, which are involved in the production of histamine, as well as serotonin and heparin. Histamine is designed to combat hypersensitivity, and heparin reduces the ability of blood to clot. Serotonin expands the vascular lumen and increases the ability of the vascular membranes to absorb and release substances.
The cells contain prostaglandins, the purpose of which is to prevent the action of the irritant and neutralize it. At this time, a person feels hyperthermia, becomes weak, and has a fever.
The main purpose of basophils is to take part in immediate and delayed hypersensitivity reactions. The cells are the first to reach the source of inflammation and signal the presence of foreign agents. If the inflammation process lasts longer than three days, more and more basophils are produced in the body.
Main functions:
- trigger the blood clotting reaction;
- participate in the creation of new blood vessels;
- participate in triggering allergic reactions;
- help increase capillary permeability;
- protect the body from infections and parasitic infestations.
A normal indicator is the presence of no more than 1% basophils in the blood. A reduced amount (basopenia) and an increased amount (basophilia) are grounds to suspect an inflammatory process or blood pathology.
Basophils
Basophils have been interpreted in recent years as a small but powerful subpopulation of leukocytes capable of linking innate and adaptive immunity. They can be activated through IgE-dependent and IgE-independent mechanisms to release preformed mediators and to produce Th2 cytokines. In addition to their role in protective immunity to helminths, basophils are major participants in allergic reactions such as anaphylaxis and immediate hypersensitivity reactions, late phase hypersensitivity reactions, and delayed hypersensitivity reactions. In addition, basophils are involved in the pathogenesis of autoimmune diseases such as lupus nephritis and rheumatoid arthritis, as well as the modulation of immune responses to bacterial infections, and their increase is a feature of myelogenous leukemias. Various signals for basophil activation, degranulation, transendothelial migration and immune regulation demonstrate the important role of basophils in the development of the Th2 microenvironment.
Historically, basophils have been mainly associated with immediate hypersensitivity reactions based on the expression of high-affinity IgE receptor (FcƐRI) on their cell surface and the release of histamine and other atopic mediators upon cross-linking of FcƐRI (Chirumbolo S., 2012; Siracusa M, Artis D., 2010) . However, this perception of limited functionality of basophils is changing dramatically, reflecting their expression of numerous cell surface receptors that, when ligated, are capable of transcriptionally activating basophils to produce cytokines that stimulate and regulate adaptive Th2 immune responses, making them important for late phase hypersensitivity and hypersensitivity responses delayed action, as well as immediate hypersensitivity reactions (Dvorak A., et.al., 1976; Wang H., et.al., 2010; Sabato V., et.al., 2012).
There is also evidence that basophils may be important in the pathogenesis of autoimmune diseases (Charles N., 2010; et.al., Warde N., 2010) and physiological responses of the immune system to infection (Anyan W., et.al., 2010 ; Pelleau S., et.al. 2012) and myeloid leukemia. Thus, basophils are becoming a recognized potential target for use in the therapy of atopy, autoimmunity and myeloid leukemia /
Derived from CD34+ myeloid hematopoietic progenitors in the bone marrow, basophils are phenotypically and functionally distinct from other leukocytes, including mast cells. Although basophils and mast cells share many characteristics, mast cells are found in tissues, whereas basophils are found in the circulation and can be recruited to tissues. The key difference from mast cells is the lack of expression of CD117 (c-kit) by basophils and the high expression of CD123 (IL-3Rα) by basophils (Valent P., et.al., 1989). In vitro mast cell formation occurs when CD34+ cells are cultured with stem cell factor (SCF, a ligand for CD117) and IL-6. While in vitro, basophil withdrawal occurs when CD34+ cells are cultured with IL-3 in the absence of SCF. Under natural conditions, basophils enter the blood circulation with a mature phenotype and survive for approximately 5 days (Sokol C., Medzhitov R., 2010). Consequently, the turnover rate of basophils is high, and progenitor cells are constantly cued to differentiate into basophils to maintain homeostatic surveillance in the periphery.
Basophils can be morphologically distinguished from other circulating leukocytes by the metachromatic staining of their cytoplasmic granules with Wright Giemsa or Toluidine blue. Basophils can be phenotypically identified by multiparameter flow cytometry or immunohistochemistry as FCƐRI+, CD123+, and CD303− (excluding plasmacytoid dendritic cells). Basophils also express low levels of CD203c, which increases with basophil activation and may correspond to partial degranulation (Sabato V., et.al., 2012). ]. CD203c is a type II glycosylated transmembrane molecule that belongs to the ecto-nucleotide pyrophosphatase phosphodiesterase (E-NPP3) enzyme family. Basophil activation also induces CD69 expression, while basophil degranulation correlates with CD63 expression, as a consequence of the fusion of the cytoplasmic granule membrane with the cell surface plasma membrane, which is called “anaphylactic degranulation” (Bieneman A., et.al., 2005; Kleine- Tebbe J., et.al., 2006; MacGlashan D., 2019; Crivellato E., et.al., 2011). CD69 is a member of the animal C-type lectin superfamily that functions as a signal transducing receptor and is expressed on virtually all activated hematopoietic cells. CD63 is a tetraspanin family 53 glycoprotein expressed in the cytoplasmic granule membranes of basophils as well as other granulocytes. Exocytosis results in the fusion of the granular membrane with the cell membrane and hence the expression of CD63 on the cell surface, where it functions to interact with integrins.
Basophils were initially noted for their rapid release of histamine and synthesis of leukotriene C4 (LTC4) following cross-linking of IgE bound to their FcƐRI, and subsequently for their synthesis of IL-4 and IL-13 in response to FcƐRI cross-linking. Basophils contain approximately 1 pg of histamine/cell and can synthesize more IL-4 and IL-13/cell than other leukocytes. Thus, basophils have the ability to link innate and adaptive immunity, including the ability to induce and propagate Th2 immune responses. The complexity of basophil activation is also supported by their sensitivity to IgE-independent mechanisms including ligation of toll-like receptors (TLRs) 2 and 4, IL-3R, IL-5R, IL-18R, IL33R (ST2), C5aR, leukocyte inhibitory receptors (LIR ), chemokine receptor (CCR) 2, CCR3, chemoattractant receptor Th2 homologous (CRTH2), granulocyte-macrophage colony-stimulating factor receptor (GM-CSFR, CD116), CD32 (FcγRII), CD62L and CD40L. Basophilic degranulation is largely limited by signals induced by Fc-RI cross-linking or anaphylatoxin C5a, and to a lesser extent by IL-3. Other IgE-independent stimuli promote the production of predominantly Th2 cytokines (IL-4, IL-13 and, to a lesser extent, IL-5), but these stimuli alone do not induce basophil degranulation.
IL-3
In addition to its role in promoting basophil differentiation, IL-3 is a physiologically important enhancer of basophil sensitivity to agonist factors and basophil effector functions. In particular, in the presence of IL-3, basophil degranulation and Th2 cytokine synthesis are enhanced in response to Fc-RI cross-linking. The role of IL-3 in basophilic biology cannot be overstated. It is important for many functions during the basophil life cycle and serves to stimulate signaling, growth and transmitter release, and often has enhanced effects when combined with other stimuli. For example, IL-3 is synergistic with IL-33 in stimulating basophil Th2 cytokine synthesis (Pecaric-Petkovic T., et.al., 2009).
Literature
- Anyan WK, Kumagi T, Shimogawara RF, et al. Schistosome eggs have a direct role in the induction of basophils capable of a high level of IL-4 production: Comparative study of single- and bisexual infection of Schistosoma mansoni in vivo. Tropical Medicine and Health. 2010;38(1):13–22
- Bieneman AP, Chichester KL, Chen YH, Schroeder JT. Toll-like receptor 2 ligands activate human basophils for both IgE-dependent and IgE-independent secretion. J Allergy Clin Immunol. 2005;115:295–30
- Charles N, Hardwick D, Daugas E, et al. Basophils and the T helper 2 environment can promote the development of lupus nephritis. Nat Med. 2010;16(6):701–707. This was the first report potentially linking basophils to the pathogenesis of autoimmune lupus nephritis.
- Dvorak AM, Mihm MC, Dvorak HF. Degranulation of basophilic leukocytes in allergic contact dermatitis reactions in man. J Immunol. 1976;116:687–695
- Chirumbolo S. State-of-the-art review about basophil research in immunology and allergy: is the time right to treat these cells with the respect they deserve? Blood Transfus. 2012;10:148–164.
- Crivellato E, Beatrice N, Ribatti D. The history of the controversial relationship between mast cells and basophils. Immunology Letters. 2011;141(1):10–17
- Kleine-Tebbe J, Erdmann S, Knol EF, et al. Diagnostic tests based on human basophils: potentials, pitfalls and perspectives. Int Arch Allergy Immunol. 2006;141:79–90.
- MacGlashan D. Jr. Expression of CD203c and CD63 in human basophils: relationship to differential regulation of piecemeal and anaphylactic degranulation processes. Clin Exp Allergy. 2010;40:1365–1377.
- Pecaric-Petkovic T, Didichenko SA, Kaempfer S, et al. Human basophils and eosinophils are the direct target leukocytes of the novel IL-1 family member IL-33. Blood. 2009;113:1526–1534
- Pelleau S, Diop S, Dia Badiane M, et al. Enhanced basophil reactivities during severe malaria and their relationship with the plasmodial histamine releasing factor PfTCTP. Infect Immune. 2012;80(8):2963–2970.
- Sabato V, Verweij MM, Bridts CH, et al. CD300a is expressed on human basophils and seems to inhibit IgE/FcƐ RI-dependent anaphylactic degranulation Clinical Cytometry. 2012;82B:132–138.
- Siracusa MC, Artis D. Basophil Functions During Type 2 Inflammation: Initiators, Regulators and Effectors. The Open Allergy Journal. 2010;3:46–51
- Sokol CL, Medzhitov R. Emerging functions of basophils in protective and allergic immune responses. Mucosal Immunology. 2010;3(2):129–137. This review explained the role of basophils in promoting Th2 immune responses
- Valent P, Schmidt G, Mayer P, et al. Interleukin-3 is a differentiation factor for human basophils. Blood. 1989;73(7):1763–1769
- Wang H, Fang Y, Barrenas F, et al. Allergen challenge of peripheral blood mononuclear cells from patients with seasonal allergic rhinitis increases IL-17RB, which regulates basophil apoptosis and degranulation Clinical & Experimental Allergy. Clinical et experimental allergy. 2010;40:1194–1202
- Warde N. Activated basophils exacerbate lupus nephritis by amplifying production of autoreactive IgE. Nat Rev Rheumatol. 2010;6(8):438.
When is it necessary to determine basophils in the blood?
A blood test to determine the level of basophils is carried out:
- during routine medical examinations;
- during examination before hospitalization for surgery;
- for the purpose of diagnosing infectious diseases, inflammatory phenomena, blood pathologies;
- to monitor the correctness of treatment.
The results are interpreted within the limits of the leukocyte formula; blood is not taken separately for basophils in laboratories.
Based on the level of this type of leukocyte, the doctor receives information about the presence/absence of an inflammatory process, the occurrence of allergic reactions, and may suspect a malignant blood disease. The result must be interpreted by a doctor: hematologist, infectious disease specialist, internist or pediatrician.
Functions
Cytoplasmic granules contain proteins and enzymes that determine the functions of basophils. Such bioactive substances include histamine, heparin, serotonin and others.
The main one is histamine. Thanks to it, smooth muscles contract and vascular permeability increases. This leads to the formation of tissue edema, decreased blood pressure, increased blood viscosity, and promotes the process of phagocytosis.
Basophils are easy to detect in a blood smear
Heparin is considered the second most important bioactive substance. It is a histamine antagonist that leads to blood thinning.
Serotonin dilates blood vessels, stimulates platelet activity, and increases vascular permeability.
The chemotactic eosinophilic factor found in basophils is involved in attracting eosinophils to the area of inflammation.
On the surface of the basophilic granulocyte there is immunoglobulin E. When it comes into contact with the allergen, basophils degranulate, resulting in the release of active substances from the granules.
These cells are able to migrate from the blood into tissues and move into them. Tissue basophils and basophils in the blood perform the following functions:
- maintain blood flow in small vessels;
- promote the movement of other leukocytes into the tissue through the capillary wall to the location of the harmful agent;
- responsible for the growth of new capillaries and tissue trophism;
- actively fight helminths;
- protect the skin, mucous membrane and intestines when infected with ticks and helminths;
- block insect poisons in tissues and prevent them from spreading;
- take part in the development of allergic reactions;
- capable of phagocytosis, although this is not their main function;
- cleanse tissues of bioactive substances, synthesize and accumulate them in granules, then remove them.
Normal indicators
The blood test form contains two indicators: relative, which shows the proportion of cells in the total number of leukocytes (BA%) and absolute, showing the number of basophils (BA#).
Each laboratory indicates its own normal ranges on the form, since indicators differ among clinics due to the specific equipment used for laboratory tests.
The number of basophils does not depend on gender, age, or time of day. Normally, the relative indicator is: 0-1%, absolute: 0-0.09*109/l. The absolute value gives a more complete picture of health. Sometimes it may be necessary to manually determine cell counts under a microscope.
The interpretation of the tests is carried out by the doctor as a whole, so based on only one indicator it is impossible to establish an accurate diagnosis.
Functions of basophils
Basophils take an active part in immune reactions, in particular in the reaction of inflammation, allergy or anaphylaxis. When an allergen, toxin or antigen is detected, the basophil releases from its granules all biologically active substances that block the action of substances dangerous to the body and, in parallel, trigger a whole cascade of inflammatory reactions aimed at improving access of other immune cells to the pathological focus.
Thus, basophils, firstly, neutralize the spread of toxins throughout the body, and secondly, create conditions for the work of other immunocompetent cells (for example, lymphocytes).
Why basophils may be elevated
Basophilia is diagnosed when the number of cells exceeds 0.2*109 /l. The use of drugs with estrogen hormones, as well as the use of thyreostatic drugs, can distort the picture. An increase in the rate is observed at the beginning of the menstrual cycle in women.
Basophils are increased:
- for chronic diseases of the gastrointestinal tract: inflammation of the gastric mucosa, enterocolitis, ulcerative inflammation of the large intestine, ulcerative lesions of the stomach and duodenum;
- at the stage of weakening of acute symptoms of an infectious disease;
- for blood diseases: acute form of leukemia, chronic myeloid leukemia, anemia, polycythemia, hemophilia, lymphogranulomatosis;
- for allergies and diabetes;
- with a decrease in the hormonal activity of the thyroid gland - hypothyroidism;
- oncology of the lymphatic system, blood cancer, lung cancer;
- due to prolonged exposure to low doses of radiation.
The main reasons for the increase in the indicator are a violation of immune defense and active invasion of the pathogen. In an adult, basophils may be elevated after removal of the spleen.
A child's concentration may increase:
- due to taking medications that cause allergies;
- due to a hidden inflammatory process;
- due to a recent vaccination or mosquito bite that gives rise to allergies;
- due to the introduction of foreign proteins.
To exclude pathology, a repeat analysis is recommended a week after the cessation of the above reasons. If the indicators are high again, a comprehensive examination is prescribed to identify the exact cause.
How to reduce?
Reducing elevated basophils is, first of all, a comprehensive examination and diagnosis, since this condition is most often a symptom of the disease. Treatment of the primary pathology will normalize the level of granulocytes.
Only a doctor should prescribe treatment to reduce the level of basophils in the blood
If basophils are elevated, it is possible that the body lacks iron and vitamin B12. In this case, iron supplements and pure vitamins for injection may be prescribed. Vitamin B12 normalizes brain function and takes part in the formation of new blood cells.
Some foods serve as sources of iron and B12, which are recommended to be eaten when basophils are reduced. As a rule, this is food of animal origin. A lot of iron is found in the following foods:
- veal and beef liver;
- red meat;
- liver;
- fish;
- oysters
It is not enough to simply eat foods rich in iron; it must be absorbed by the body. To do this, it is recommended to drink dry wine (white) and orange juice, which promote its absorption.
To compensate for the lack of B12, you need to eat meat products, eggs, and milk. This vitamin is found in soy milk and yeast, although it is much less there than in the above.