What is the renin-angiotensin-aldosterone system
The principle of operation of the RAAS
It would seem that renin is an enzyme produced by the kidneys, angiotensinogen is a glycoprotein synthesized by the liver, and aldosterone is generally an adrenal hormone - what do they have in common. However, they form a single system, which is triggered by the production of renin in the juxtaglomerular cells of the kidneys.
There are several mechanisms for stimulating enzyme synthesis:
- Macular. It is triggered if the supply of sodium ions in the distal convoluted tubule decreases.
- Intrarenal baroreceptor. Juxtaglomerular cells are baroreceptors; they perceive stretching of the arteriolar walls and accordingly respond to a decrease in pressure by producing renin.
- Sympathetic. Juxtaglomerular cells are innervated by the sympathetic nervous system, and as soon as they receive a signal, they immediately begin to synthesize an enzyme that increases blood pressure. This is why arterial hypertension occurs during stress and psycho-emotional stress.
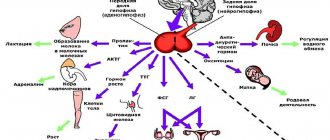
Renin then enters the blood. There it acts on the glycoprotein angiotensinogen, produced by the liver. Thus, angiotensinogen is converted to angiotensin I. Under the influence of angiotensin-converting enzyme (ACE), the dipeptide of angiotensin I is cleaved, and it becomes the most powerful vasoconstrictor - angiotensin II. In addition to the fact that it causes spasm of smooth muscles, inhibits the production of bradykinin, it stimulates the synthesis of aldosterone. This hormone produced by the adrenal glands:
- retains sodium ions and water;
- removes potassium;
- enhances the synthesis of ATPase by affecting DNA.
As soon as the sodium concentration in the blood normalizes, renin production stops. All reaction products disintegrate, the pressure normalizes, and vasodilators begin to be synthesized:
- bradykinin;
- kallidin.
The work of the renin-angiotensin-aldosterone system can be stimulated due to various pathologies. For example, with renal artery stenosis, the RAAS is triggered. Due to the production of the most effective vasoconstrictor angiotensin II, vasospasm occurs. And this leads to unnecessary hypertension. The pressure increases significantly, and blood microcirculation is accordingly disrupted. Fewer amounts of nutrients, vital microelements and oxygen are brought to the organs (without it, brain cells begin to die after 5 minutes).
Situations in which renin is released into the blood
There are several conditions in which the hormone enters the bloodstream:
- Reduced blood flow in the kidney tissue - during inflammatory processes (glomerulonephritis, etc.), diabetic nephropathy, kidney tumors.
- Decrease in circulating blood volume (with bleeding, repeated vomiting, diarrhea, burns).
- Falling blood pressure levels. The arteries of the kidneys contain baroreceptors that respond to changes in systemic pressure.
- Change in sodium ion concentration. In the human body there are clusters of cells that respond to changes in the ionic composition of the blood by stimulating the production of renin. Salt is lost through excessive sweating and vomiting.
- Stress, psycho-emotional stress. The juxtaglomerular apparatus of the kidney is innervated by sympathetic nerves, which are activated by negative psychological influences.
In the blood, renin meets with a protein - angiotensinogen, which is produced by liver cells and takes a fragment from it. Angiotensin I is formed, which is a source of action for angiotensin-converting enzyme (ACE). The result is angiotensin II, which serves as the second link and is a powerful vasoconstrictor of the arterial system (narrows blood vessels).
Functions of the RAAS
As soon as the concentration of sodium ions in the distal tubules of the kidneys decreases, a signal from the sympathetic nervous system is sent to the juxtaglomerular cells, baroreceptors react to the dilation of the arteriolar wall, and the renin-angiotensin-aldosterone system immediately turns on. All reactions occur almost instantly, but even in such a short time the RAAS copes with its functions:
- maintains acid-base balance;
- regulates water-salt metabolism;
- affects the restoration of blood volume;
- enhances glomerular filtration rate.
The course of chemical reactions is affected by the acid-base balance. It is maintained in the body thanks to the work of the kidneys, buffer systems and lungs. If the sodium concentration in the blood decreases, the RAAS is activated. Under the influence of aldosterone, ions return to the blood and combine with anions, thereby creating an alkaline environment. Acids are excreted from the body in the form of ammonium salts (urea). This process helps retain essential minerals (sodium, potassium, magnesium) in the body and eliminate toxins.
As soon as under the influence of the RAAS in the blood, due to an increase in salts, the osmotic pressure increases, the production of vasopressin is stimulated, and the synthesis of aldosterone is influenced.
- When the concentration of sodium chloride decreases under the influence of hormones, sodium is retained in the body and water is excreted. This way the body retains the required amount of salts.
- As soon as the concentration of sodium chloride increases, the RAAS stops working. In the renal glomeruli, excess salts are removed from the body.
In this way, water-salt metabolism is regulated and thereby supported:
- required blood volume;
- normal sodium concentration.
In addition to vasopressin and aldosterone, angiotensin also regulates water-salt balance. When the amount of water in the blood decreases, it constricts the walls of blood vessels to temporarily maintain normal blood pressure (if the blood volume is insufficient, hypotension occurs) and provide all organs with the necessary substances. It also affects the thirst center located in the 3rd ventricle of the brain, which makes you want to drink. As soon as the necessary fluid and salts enter the body, renin ceases to be produced. At this point, the work of the RAAS temporarily stops.
If there is a malfunction of the renin-angiotensin-aldosterone system in the body, for example, due to:
- hormone-producing adrenal tumor;
- renal artery stenosis;
- inflammatory kidney diseases;
- renal failure;
- kidney tumors and other pathologies.
This will lead to constantly elevated blood pressure.
In addition, angiotensin II has a direct effect on the central nervous system; an impulse occurs that literally commands the smooth muscles to contract. The walls of blood vessels contract, the heart rate increases, and blood pressure rises.
The study of the mechanism of action of the RAAS led to the invention of effective antihypertensive drugs:
- angiotensin receptor blockers;
- ACE inhibitors.
All these medications affect individual elements of the chain of renin production, angiotensin conversion, and aldosterone synthesis. Naturally, they negatively affect the functioning of the system and help lower blood pressure.
Renin-angiotensin system and its activation
Renin-angiotensin system (RAS)
- a multicomponent enzyme-hormonal system that plays a key role in regulating pressure in the vascular system and fluid volume in the body
Circulating renin-angiotensin system
- a corresponding system that plays a key role in regulating pressure in the vascular system and fluid volume in the body
Tissue renin-angiotensin system
- a similar system, the components of which are contained and enzymatically transformed in tissues.
The activation of the renin-angiotensin system begins with an increase in the secretion of renin by the juxtaglomerular cells of the afferent arterioles of the kidneys, which is stimulated by:
a) a decrease in blood pressure in the above afferent arterioles;
b) a decrease in the concentration of Na+ ions in the distal tubules; c) sympathetic stimulation of the kidneys, mediated through β1 receptors; d) vasodilatory prostaglandins (prostacyclin, PgE2). The “end point” of the functioning of the renin-angiotensin system is the interaction of angiotensin II with its tissue receptors, as a result of which the physiological effects of the renin-angiotensin system are realized.
Schematic diagram of the functioning of the renin-angiotensin system
GENERAL SCHEME OF WATER-SALT BALANCE
The system for regulating water-salt balance has two compensating components: 1) the digestive tract, which can approximately correct disturbances in the water-salt balance due to thirst and salt appetite; 2) kidneys, capable of providing adequate retention or excretion of water and salts to maintain balance. In Fig. Figure 1 shows a diagram of the main routes of entry and release of water and salts. The main channel for the entry of water and salts into the blood plasma and other body fluids is the gastrointestinal tract. Per day consumption is approximately 2.5 liters of water and 7 g of sodium chloride. To this you can add 0.3 liters of metabolic water, released as a result of oxidative metabolism, and 30 g of urea, the final product of protein metabolism, which enter the blood plasma through the intercellular sector. The three main fluid sectors of the body are dynamically exchanging pools. The interstitial and intracellular sectors are able to quickly respond to changes in the volume and composition of blood plasma. The amount of water and sodium in the extracellular fluid under normal conditions is maintained within narrow limits due to the dynamic equilibrium between their loss and gain. Of the four ways of excreting fluid and salts, the kidneys are the most significant: per day, the kidneys excrete approximately 1.5 liters of water, 6.2 g of sodium chloride and almost all urea. Some water loss occurs through evaporation from the mucous membranes of the respiratory tract and from the skin (imperceptible losses). Water and salts are also lost through sweat and feces. Extrarenal losses are approximately 1.3 L per day. If there is a discrepancy between intake and excretion, the volume and/or composition of body fluids is disrupted. And in this sense, almost all channels of entry and exit, with the exception of the renal ones, can be a source of disturbances in the system of regulation of water-salt metabolism.
LIQUID SECTORS OF THE BODY,
THEIR VOLUME AND COMPOSITION
The structure and dimensions of the fluid sectors of the body, that is, spaces filled with fluid and separated by cell membranes, have now been quite well studied [1]. The total volume of body fluids, which in mammals accounts for approximately 60% of body weight, is distributed between two large sectors: intracellular (40% of body weight) and extracellular (20% of body weight). The extracellular sector includes the volume of fluid located in the interstitial (intercellular) space and fluid circulating in the vascular bed. A small volume is also made up of the so-called transcellular fluid, located in regional cavities (cerebrospinal, intraocular, intraarticular, pleural, etc.). Extracellular and intracellular fluids differ significantly in composition and concentration of individual components, but the total total concentration of osmotically active substances is approximately the same (Table 1). The movement of water from one sector to another occurs even with small deviations in the total osmotic concentration. Since most dissolved substances and water molecules pass quite easily through the capillary epithelium, rapid mixing of all components (except protein) occurs between the blood plasma and the interstitial fluid. Many factors, such as intake, loss or limitation of water intake, increased salt intake or, conversely, its deficiency, shift in metabolic rate, etc., can change the volume and composition of body fluids. The deviation of these parameters from a certain normal level includes mechanisms that correct disturbances of water-salt homeostasis.
baroceptors, mechanoreceptors, pressoreceptors, sensitive nerve endings in blood vessels that perceive changes in blood pressure and reflexively regulate its level; come into a state of excitation when the walls of blood vessels are stretched.
Volume receptors. sensitive nerve endings in various organs and blood vessels that respond to stretching of their walls. volume receptors of the vascular bed, responding to changes in the volume of blood circulating in the vascular system.
tissue osmoreceptors, which signal changes in osmotic pressure in tissues. The feeling of thirst when osmoreceptors are stimulated is a true type of thirst.
Regulation of water and electrolyte balance. To maintain homeostasis, the release of water and electrolytes must exactly match their intake. If intake exceeds excretion, the amount of this substance in the body will increase. If less substance enters than is excreted, then its amount will decrease.
The renin-angiotensin-aldosterone system regulates sodium reabsorption by the kidney.
The renin-angiotensin-aldosterone system (RAAS) includes the following elements [1]. Renin, a proteolytic enzyme secreted by the kidneys into the blood, cleaves off a short peptide of 10 amino acids, the so-called angiotensin I, from a fragment of plasma a2-globulin. Under the action of a converting enzyme in the lungs, inactive angiotensin I is converted into an active form, angiotensin II. This low molecular weight (8 amino acids) peptide is a physiologically highly active substance that has multiple effects, among which the most significant are stimulation of the synthesis and secretion of the hormone aldosterone from the zona glomerulosa of the adrenal cortex and a powerful vasoconstrictor effect. Inactivation of angiotensin II with its conversion into angiotensin III is carried out by the blood plasma angiotensinase system. Aldosterone released from the adrenal glands stimulates the reabsorption of sodium in the renal tubules and leads to the retention of this ion in the body. The key link in the chain is the secretion of renin by the kidney. The enzyme has been isolated from animals and humans in purified form. Renin is produced in special cells of the wall of the afferent arteriole of the glomerulus in the so-called juxtaglomerular apparatus (JGA), directly adjacent to the glomerulus. The design of this apparatus is such that renin-producing cells are sensitive both to changes in blood pressure in the afferent arteriole and to the intensity of sodium transport by the cells of the distal tubule when the sodium concentration in the tubular fluid changes. To date, the pathways of renin biosynthesis have been well studied both in animals of various species and in humans. The structure of the genes producing renin has been deciphered. Some of them have been synthesized using genetic engineering, including the human renin gene. Cloned antibodies have been obtained for it and are already used for diagnostic purposes.
The regulated parameters in the RAAS are volume and pressure in various intravascular compartments. In this case, the sequence of events can be represented as follows. When the volume of circulating blood decreases, regardless of the reasons for this, the blood supply to the renal artery system is limited and at the same time the degree of stretching of the wall of the afferent arterioles of the glomerulus, in which renin-producing cells are localized, decreases. Reducing wall tension stimulates renin secretion. A decrease in circulatory volume is also a stimulus for the correction of blood pressure from the baroreceptor zones of the aortic arch and the carotid artery zone, which results in increased activity of the centers of the sympathetic nervous system, including an increase in the tone of the sympathetic fibers innervating the JGA. An increase in renin activity in the blood leads to increased formation of angiotensin II, which, on the one hand, increases vascular tone and contributes to an increase in blood pressure, and on the other hand, stimulates the release of aldosterone into the blood by the adrenal glands.
Aldosterone belongs to the group of corticoids, derivatives of cholesterol. Angiotensin II controls the conversion of cholesterol to pregnenolone in the zona glomerulosa, the rate-limiting step in the chain of corticosteroid biosynthesis. Aldosterone regulates extracellular fluid volume by selectively influencing sodium transport in the kidney and colon. In addition, it regulates potassium metabolism and acid-base balance, and the intensity of its secretion increases with increasing potassium concentration in the blood and with a shift in blood pH to the acidic side. The principle scheme of the mechanism of action of aldosterone has now been quite well studied, although many unclear events still remain. Penetrating into the cell, the steroid interacts with specific cytosolic proteins - receptors. The resulting complex penetrates the nucleus and induces the synthesis of certain mRNAs, which serve as a template for the biosynthesis of certain proteins. One of the main aldosterone-inducing proteins in renal tubular cells is Na-K-ATPase, which directly determines sodium transport [1]. Since increased sodium reabsorption is accompanied by the retention of a corresponding amount of water, this leads to restoration of the volume of fluid circulating in the circulatory system and interstitial sector.
It has now been shown that, in addition to the mechanisms described above, renin secretion is regulated (or modulated) simultaneously by many factors: the chemoreceptor mechanism of the macula densa, the extracellular concentration of many organic and inorganic substances, including potassium and magnesium ions, a complex of hormones and biologically active substances, such , like vasopressin, prostaglandin, etc. It has been established that negative feedback plays a significant role in the regulation of JGA - inhibition of renin secretion by angiotensins I and II formed in the blood, which increases the stability and efficiency of this system. Many relationships remain unclear, and many questions arise in solving the problem of RAAS regulation. However, the general direction of the reactions is such that a decrease in the volume of extracellular body fluids due to sodium deficiency, a decrease in circulating blood volume, or a decrease in blood pressure (hypotension) causes increased secretion of renin by the kidneys and activation of the entire system that stimulates sodium reabsorption.
Effects of angiotensin II
Goal: increase blood pressure.
- Promotes the synthesis of aldosterone in the zona glomerulosa of the adrenal cortex.
- It affects the center of hunger and thirst in the brain, causing a “salt” appetite. Human behavior becomes motivated to search for water and salty food.
- It affects the sympathetic nerves, promoting the release of norepinephrine, which is also a vasoconstrictor, but less weak in action.
- It affects blood vessels, causing them to spasm.
- Participates in the development of chronic heart failure: promotes proliferation, fibrosis of blood vessels and myocardium.
- Reduces glomerular filtration rate.
- Inhibits the production of bradykinin.
Aldosterone is the third component that acts on the terminal tubules of the kidneys and promotes the release of potassium and magnesium ions from the body and the reabsorption (reabsorption) of sodium, chlorine, and water. Due to this, the volume of circulating fluid increases, blood pressure rises, and renal blood flow increases. Receptors for aldosterone are found not only in the kidneys, but also in the heart and blood vessels.
When the body reaches homeostasis, vasodilators (substances that dilate blood vessels) - bradykinin and kallidin - begin to be produced. And the components of the RAAS are destroyed in the liver.
Highly effective groups of drugs that were synthesized through the study of the RAAS
- "Prily." ACE inhibitors (blockers). Angiotensin I does not convert to angiotensin II. No vasoconstriction - no increase in blood pressure. Drugs: Amprilan, Enalapril, Captopril, etc. ACE inhibitors significantly improve the quality of life of patients with diabetes, ensuring the prevention of renal failure. The drugs are taken in a minimal dosage, which does not cause a decrease in pressure, but only improves local blood flow and glomerular filtration. Medicines are indispensable for renal failure, chronic heart disease and serve as one of the means of treating hypertension (if there are no contraindications).
- "Sartans". Angiotensin II receptor blockers. The vessels do not react to it and do not contract. Drugs: Losartan, Eprosartan, etc.
The opposite of the renin-angiotensin-aldosterone system is the kinin system. Therefore, blocking the RAAS leads to an increase in the components of the kinin system (bradykinin, etc.) in the blood, which has a beneficial effect on heart tissue and vascular walls. The myocardium does not experience starvation, because bradykinin increases local blood flow and stimulates the production of natural vasodilators in the cells of the renal medulla and microcytes of the collecting ducts - prostaglandins E and I2. They neutralize the pressor effect of angiotensin II. The vessels are not spasmed, which ensures adequate blood supply to the organs and tissues of the body, blood is not retained and the formation of atherosclerotic plaques and blood clots is reduced. Kinins have a beneficial effect on the kidneys and increase diuresis (daily urine output).