Side effects
Below is information on the frequency of adverse events when using the drug Klimara® (MedDRA - Medical Dictionary of Regulatory Activity). The information is based on clinical trial data. The most common adverse reactions reported during clinical trials were skin irritation at the application site and breast pain (>10%). Local symptoms at the application site are generally mild and include redness, itching, burning and vesicular formation.
From the gastrointestinal tract: often (≥1/100 and <1/10) - abdominal pain, bloating, nausea.
General and local reactions: often (≥1/100 and <1/10) - swelling at the site of application of the patch.
From the musculoskeletal system, connective tissue: uncommon (≥1/1000 and <1/100) - muscle cramps
From the nervous system: often (≥1/100 and <1/10) - headache, dizziness; uncommon (≥1/1000 and <1/100) - migraine.
From the reproductive system, mammary glands: often (≥1/100 and <1/10) - engorgement of the mammary glands, changes in the nature of breakthrough bleeding and spotting from the vagina; uncommon (≥1/1000 and <1/100) - enlargement of the mammary glands.
Other: often (≥1/100 and <1/10) - changes in body weight.
Other adverse events have been reported with estrogen replacement therapy, but their connection with the use of Klimara® can neither be refuted nor proven.
Congenital hereditary genetic diseases: worsening symptoms of concomitant porphyria.
From the gastrointestinal tract: vomiting.
From the liver: cholestatic jaundice.
Mental disorders: changes in libido.
From the reproductive system, mammary glands: changes in the size of uterine leiomyomas, changes in cervical secretion in volume.
Skin and subcutaneous tissues: chloasma or melasma, which may persist after discontinuation of the drug, allergic contact dermatitis, post-inflammatory itching, generalized exanthema.
In women with hereditary forms of angioedema, exogenous estrogens can cause or worsen the symptoms of angioedema (see "Special Instructions").
Climara®
HRT drugs are used only to treat symptoms caused by estrogen deficiency that affect the patient’s quality of life. Therapy should be continued only if the benefit outweighs the risk of using the drug. If any of the conditions/risk factors listed below are currently present or worsening, the potential risks and expected benefits of treatment with Climara should be considered in each individual case before starting or continuing HRT.
The possibility of an increased synergistic risk of thrombosis in women with a combination of several risk factors, or a higher severity of one of the risk factors, should be considered. In such cases, the increased risk may be greater than the total risk taking all factors into account. HRT should not be prescribed if the risk assessment exceeds the estimated benefit of therapy.
Venous thromboembolism
A number of epidemiological studies have found a slight increase in the incidence of venous thromboembolism (VTE), such as deep vein thrombosis or pulmonary embolism, in women receiving Climara®. The risk/benefit ratio must be carefully weighed if Climara® is recommended to women with risk factors for VTE.
Risk factors for VTE include a personal or family history of VTE (the development of VTE in direct relatives at a relatively young age may indicate a genetic predisposition), systemic lupus erythematosus, cancer, and severe obesity. The risk of VTE also increases with age. There is no consensus regarding the possible role of varicose veins in the development of VTE.
In case of prolonged immobilization, extended surgery, extensive trauma, surgery on the lower extremities or pelvic area, neurosurgical operations, the drug is stopped, and the drug is resumed only after the woman has completely recovered her motor activity. In case of planned surgery, it is recommended to stop taking the drug 4-6 weeks before the planned surgery.
Treatment should be stopped immediately if symptoms of thromboembolism are present or suspected.
The use of HRT drugs, both combined and those containing only estrogens, is associated with a 1.5-fold increase in the risk of stroke. The risk of developing this complication increases with age.
Arterial thromboembolism
Randomized controlled trials with long-term use of combined CCE and MPA did not provide evidence of a beneficial effect on the cardiovascular system. Large-scale clinical trials of this compound found a possible increase in the risk of coronary heart disease (CHD) in the first year of use, followed by a lack of benefit. One large clinical trial using CBE alone found a potential reduction in the incidence of CHD among women aged 50–59 years, but no overall benefit in the overall study population.
Endometrial cancer
With long-term estrogen therapy, the risk of developing endometrial hyperplasia or cancer increases. Studies have confirmed that additional administration of gestagens reduces the risk of endometrial hyperplasia and/or cancer.
Mammary cancer
Clinical trials and observational studies have found an increase in the relative risk of developing breast cancer in women using HRT for several years. This may be due to earlier diagnosis, accelerated growth of an existing tumor during HRT, or a combination of both factors.
The increased risk of breast cancer has been suggested based on the results of more than 50 epidemiological studies (risk ranges from 1 to 2).
Two large randomized trials of CBE alone or chronically combined with MPA yielded estimated risk ratios of 0.77 (95% confidence interval: 0.59–1.01) or 1.24 (95% confidence interval: 1. 01-1.54) after approximately 6 years of HRT use. It is unknown whether this increased risk also applies to other HRT drugs.
The relative risk increases with duration of use but may be absent or reduced with estrogen-only treatment. This increase is comparable to the increase in the risk of breast cancer in women with each year of delay in the onset of natural menopause, as well as with obesity and alcohol abuse. The increased risk gradually decreases to normal levels over the first few years after stopping use of Climara®.
HRT increases mammographic breast density, which in some cases may make it difficult to detect cancer on x-rays.
Ovarian cancer
Ovarian cancer is less common in the population than breast cancer.
A meta-analysis of 52 epidemiological studies suggests a slight increase in the relative risk of ovarian cancer in women treated with hormone replacement therapy compared with women who have never received such treatment (prospective studies: RR 1.20, 95% CI 1.15-1 .26; all studies: RR 1.14, 95% CI 1.10-1.19). Women continuing to take hormone replacement therapy had a slightly increased risk of developing ovarian cancer (RR 1.43, 95% CI 1.31–1.56).
Other studies, including those from the Women's Health Initiative (WHI), suggest that combination HRT may be associated with a similar or slightly lower risk.
Moreover, the effect of duration of exposure to therapy has not been clearly established, but the risk may be more significant with long-term use (over several years).
Liver tumor
During the use of sex hormones, which include the drug Klimara®, in rare cases, benign, and even more rarely, malignant liver tumors were observed. In some cases, these tumors have resulted in life-threatening intra-abdominal bleeding. If there is pain in the upper abdomen, an enlarged liver, or signs of intra-abdominal bleeding, the differential diagnosis should take into account the possibility of a liver tumor.
Cholelithiasis
It is known that estrogens increase the lithogenicity of bile. Some women are predisposed to developing gallstones when treated with estrogen.
Dementia
There is limited clinical trial data on a possible increased risk of dementia in women starting CEE-containing medications aged 65 years or older. As observed in studies, the risk may be reduced if HRT preparations containing CEE are started in early menopause.
Other states
Treatment should be stopped immediately if migraine-like or frequent and unusually severe headaches appear for the first time, as well as if other symptoms appear that are possible precursors of an ischemic stroke.
If, despite changing the application site as recommended, recurrent persistent skin irritation (eg, persistent erythema or itching at the application site) is noted, discontinuation of transdermal treatment should be considered.
The relationship between HRT and the development of clinically significant arterial hypertension has not been established. A slight increase in blood pressure has been described in women receiving HRT, but clinically significant increases are rare. In individual cases, if persistent clinically significant arterial hypertension develops during HRT treatment, discontinuation of the drug may be considered.
Sex hormones may be poorly metabolized in patients with reduced liver function. Although there is no first pass hepatic metabolism with transdermal HRT, HRT should be used with caution in these patients.
In case of recurrence of cholestatic jaundice or cholestatic itching, which was observed for the first time during pregnancy or previous treatment with sex hormones, it is necessary to immediately stop using the drug Klimara®.
Some patients under the influence of Klimara® may develop undesirable manifestations of estrogen stimulation, such as abnormal uterine bleeding. Frequent or persistent pathological uterine bleeding during treatment is an indication for endometrial examination to exclude an organic disease.
Under the influence of estrogen, uterine fibroids can increase in size. In this case, treatment should be stopped.
It is recommended to discontinue treatment if endometriosis relapses during treatment with Klimara®.
If prolactinoma is suspected, this disease should be excluded before starting treatment. If prolactinoma is detected, the patient should be under close medical supervision (including periodic assessment of prolactin concentrations).
In some cases, chloasma may occur, especially in women with a history of chloasma during pregnancy. While using Klimara®, women with a tendency to develop chloasma should avoid prolonged exposure to the sun or exposure to ultraviolet radiation.
The following conditions may occur or be aggravated by the use of Climara®. Although their relationship with the use of Klimara® has not been proven, women with the following conditions should be under medical supervision when undergoing HRT: epilepsy, benign breast diseases, bronchial asthma, migraine, otosclerosis, systemic lupus erythematosus, chorea minor.
In women with hereditary forms of angioedema, exogenous estrogens may cause or worsen symptoms of angioedema.
Medical examinations
Before starting or resuming taking the drug Klimara®, you should familiarize yourself in detail with the patient’s medical history and conduct a general medical and gynecological examination. The frequency and nature of such examinations should be based on existing standards of medical practice with the necessary consideration of the individual characteristics of each patient (but not less than once every 6 months) and should include measurement of blood pressure, assessment of the condition of the mammary glands, abdominal and pelvic organs, including cytological examination of the cervical epithelium.
In the presence of prolactinoma, periodic determination of prolactin concentration is required.
Directions for use and doses
Cutaneously.
Treatment of symptoms of menopausal syndrome. Treatment begins with the smallest dose of the Klimara® patch. If necessary, you can use a higher dose patch. Once the dose is adjusted, the lowest effective patch dose should be used to relieve symptoms.
Prevention of osteoporosis. Treatment to prevent postmenopausal bone loss should be started immediately after menopause. Long-term treatment based on an individual approach is recommended. Treatment should be carried out either continuously or cyclically.
When switching from long-term continuous or cyclic therapy: treatment should begin the day after the end of the previous treatment regimen. Estrogen-only therapy is used if a woman has had a hysterectomy. In women with an intact uterus, a progestogen should be added to treatment with Klimara® for 10–14 days each month. When using a patch that releases more than 50 mcg of hormone/day, no protective effect on the endometrium was detected with the addition of progestogens.
The patch should be permanently applied weekly, each used patch should be removed after 7 days, after which a fresh patch should be applied to another location. Patches may also be recommended for cyclic treatment. In this case, the patch is applied weekly for 3 consecutive weeks, followed by a 7-day interval without patching until the next course of treatment.
Menstrual-like bleeding normally develops 2–3 days after stopping the use of gestagens.
Method of attaching the patch. After removing the protective film, the Klimara® patch is attached with the adhesive side to a clean, dry area of skin along the spine or to the buttocks. Klimara® should not be attached in or near the mammary glands. The area chosen for fixing the patch should not be greasy, damaged or irritated; it is also necessary to avoid the waist area, because When rubbed by tight clothing, the patch may come off. Avoid applying the patch to areas of the skin where the patch could become dislodged when sitting. The patch must be attached immediately after opening the package and removing the protective film. The patch should be firmly pressed with the palm of your hand to the place of fixation for approximately 10 s. You need to make sure there is good contact with the skin, especially around the edges. If the patch does not fit tightly, you should press on it for better adhesion. The application site should be changed with an interval of at least 1 week between applications. If the patch is attached correctly, the patient can bathe or shower as usual. However, the patch may come off from the skin when exposed to very hot water or in a sauna.
Untimely replacement or loss of the patch. If the patch comes off before the end of the 7-day course of treatment, you can try to glue it again. If necessary, you can apply a new patch for the remaining days of the 7-day application interval.
If the patient forgot to change the patch on time, the replacement should be made as soon as possible after the fact of omission has been established. A new patch should be used after the normal 7-day treatment period has ended.
Klimara
The estrogenic drug 17-beta-estradiol is identical to endogenous estradiol (formed in the body of women, from the first menstruation until menopause) produced by the ovaries. In the cells of the organs to which the action of hormones is directed, estrogens form a complex with specific receptors (found in various organs - in the uterus, vagina, urethra, mammary gland, liver, hypothalamus, pituitary gland), the receptor-ligand complex interacts with estrogen-effector elements genome and specific intracellular proteins that induce the synthesis of mRNA, proteins and the release of cytokines and growth factors.
Has a feminizing effect on the body. Stimulates the development of the uterus, fallopian tubes, vagina, stroma and ducts of the mammary glands, pigmentation in the area of the nipples and genitals, the formation of secondary sexual characteristics of the female type, the growth and closure of the epiphyses of long tubular bones. Promotes timely endometrial rejection and regular bleeding, in high concentrations causes endometrial hyperplasia, suppresses lactation, inhibits bone resorption, stimulates the synthesis of a number of transport proteins (thyroxine-binding globulin, transcortin, transferrin, sex hormone binding protein), fibrinogen. It has a procoagulant effect, increases the synthesis of vitamin K-dependent blood coagulation factors (II, VII, IX, X) in the liver, reduces the concentration of antithrombin III.
Increases blood concentrations of T4, Fe, Cu2+, etc. Has an anti-atherosclerotic effect, increases the concentration of HDL, reduces LDL and cholesterol (TG concentration increases). Modulates the sensitivity of receptors to progesterone and sympathetic regulation of smooth muscle tone, stimulates the transition of intravascular fluid into tissues and causes compensatory retention of Na+ and water. In large doses, it prevents the degradation of endogenous catecholamines by competing for active catechol-O-methyltransferase receptors.
After menopause, only a small amount of estradiol is produced in the body (from estrone found in the liver and adipose tissue). A decrease in the concentration of estradiol produced in the ovaries is accompanied in many women by vasomotor and thermoregulatory instability (“flushes” of blood to the facial skin), sleep disorders, as well as progressive atrophy of the genitourinary system.
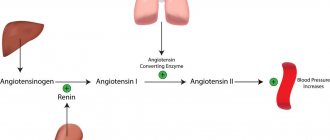
Osteoporosis (mainly of the spine) develops due to estrogen deficiency. It is known that oral administration of estrogens causes an increase in protein synthesis (including renin), which leads to an increase in blood pressure.
Estradiol in the form of a TTC drug is a patch attached to an area of skin. The control membrane ensures a gradual and continuous release of estradiol (the active ingredient of the drug) from the reservoir with the active substance through the adhesive layer onto the skin. Due to the lack of a “first pass” effect through the liver, TTC provides high efficacy when using lower doses of the drug. TTS of the active substance of the drug delivers estradiol unchanged into the bloodstream and maintains its concentration in plasma during therapy at a constant level, adequate to the level in the early or middle phase of the follicle.
Precautionary measures
Before starting use, it is necessary to conduct a complete general medical and gynecological examination (including examination of the mammary glands, cervical smear cytology), and exclude pregnancy. The patch should not be placed on the breast or waist area. If the patch is applied correctly, you can take a bath or shower, but keep in mind that the patch may come off in hot water. It is necessary to inform your doctor about the presence of diabetes mellitus, hypertension, varicose veins, otosclerosis, multiple sclerosis, epilepsy, porphyria, tetany, minor chorea, heart failure, liver or kidney dysfunction, migraine, as well as about the simultaneous use of barbiturates, phenylbutazone, hydantoin , rifampicin, the appearance of irregular bleeding or unusually heavy bleeding in the period between the use of the drug, discomfort in the epigastric region.
During treatment, it should be taken into account that long-term use of estrogen alone during menopause can lead to endometrial hyperplasia and increase the risk of developing endometrial cancer. To reduce the risk of developing endometrial cancer, additional intake of progestogen is necessary (usually for 10-12 days a month), which leads to the transition of the uterine mucosa into the secretory phase with its rejection and subsequent menstrual-like bleeding after stopping the administration of progestogen.
Klimara transdermal therapeutic system 3.9 mg/12.5 sq. cm No. 4
special instructions
If any of the conditions/risk factors listed below are currently present or worsening, the potential risks and expected benefits of treatment with Climara should be considered in each individual case before starting or continuing HRT.
- Venous thromboembolism A number of epidemiological studies have found a slight increase in the incidence of venous thromboembolism (VTE), for example, deep vein thrombosis or pulmonary embolism in women receiving Climara. The risk/benefit ratio must be carefully weighed if Climara is recommended in women with risk factors for VTE. Risk factors for VTE include a personal or family history of VTE (the development of VTE in direct relatives at a relatively young age may indicate a genetic predisposition), as well as severe obesity. The risk of VTE also increases with age. There is no consensus regarding the possible role of varicose veins in the development of VTE. The risk of VTE temporarily increases with prolonged immobilization, major surgery, or major trauma. Depending on the etiology of the disease and the duration of immobilization, temporary discontinuation of the use of Klimara should be considered. Treatment should be stopped immediately if symptoms of thromboembolism are present or suspected. — Arterial thromboembolism Randomized controlled trials with long-term use of combined conjugated equine estrogens (CEE) and medroxyprogesterone acetate (MPA) did not provide evidence of a beneficial effect on the cardiovascular system. Large-scale clinical trials of this compound found a possible increase in the risk of coronary heart disease (CHD) in the first year of use, followed by a lack of benefit. One large clinical trial using CLE alone found a potential reduction in the incidence of CAD among women aged 50–59 years, but no overall benefit in the overall study population. As a secondary outcome, two large clinical trials using CLE as monotherapy or in combination with MPA found a 30-40% increase in the risk of stroke. It is unknown whether this increased risk applies to HRT products containing other types of estrogens and progestogens or to non-oral routes of administration. — Endometrial cancer Long-term estrogen therapy increases the risk of developing endometrial hyperplasia or cancer. Studies have confirmed that additional administration of gestagens reduces the risk of endometrial hyperplasia and/or cancer. - Breast cancer Clinical trials and observational studies have found an increase in the relative risk of developing breast cancer in women who have used HRT for several years. This may be due to earlier diagnosis, accelerated growth of an existing tumor during HRT, or a combination of both factors. The increased risk of breast cancer has been suggested based on the results of more than 50 epidemiological studies (risk ranges from 1 to 2). Two large randomized trials of CLE alone or chronically combined with MPA yielded estimated risk ratios of 0.77 (95% confidence interval: 0.59–1.01) or 1.24 (95% confidence interval: 1. 01-1.54) after approximately 6 years of HRT use. It is unknown whether this increased risk also applies to other HRT products. The relative risk increases with duration of use but may be absent or reduced with estrogen-only treatment. This increase is comparable to the increase in the risk of breast cancer in women with each year of delay in the onset of natural menopause, as well as with obesity and alcohol abuse. The increased risk gradually decreases to normal levels over the first few years after stopping use of Climara. HRT increases mammographic breast density, which in some cases may make it difficult to detect cancer on x-rays. — Ovarian cancer During an epidemiological study, a slight increase in the risk of developing ovarian cancer was noted in women using estrogen replacement therapy for a long time (more than 10 years). At the same time, a meta-analysis of 15 studies did not reveal an increased risk when using the drug Klimara®. Thus, data on the effect of Klimara® on the risk of ovarian cancer are currently controversial. — Liver tumor During the use of sex hormones, which include the drug Klimara®, in rare cases benign, and even more rarely, malignant liver tumors were observed. In some cases, these tumors have resulted in life-threatening intra-abdominal bleeding. If there is pain in the upper abdomen, an enlarged liver, or signs of intra-abdominal bleeding, the differential diagnosis should take into account the possibility of a liver tumor. — Gallstone disease It is known that estrogens increase the lithogenicity of bile. Some women are predisposed to developing gallstones when treated with estrogen. — Dementia There is limited clinical trial evidence of a possible increased risk of dementia in women starting CLE-containing medications aged 65 years or older. As observed in studies, the risk may be reduced if CLE-containing HRT medications are started in early menopause. It is not known whether this applies to other HRT medications. - Other conditions Treatment should be stopped immediately if migraine-like or frequent and unusually severe headaches appear for the first time, as well as if other symptoms appear that are possible precursors of an ischemic stroke. If, despite changing the application site as recommended, recurrent persistent skin irritation (eg, persistent erythema or itching at the application site) is noted, discontinuation of transdermal treatment should be considered. The relationship between HRT and the development of clinically significant arterial hypertension has not been established. A slight increase in blood pressure has been described in women receiving HRT, but clinically significant increases are rare. In individual cases, with the development of persistent clinically significant arterial hypertension during HRT treatment, discontinuation of the drug may be considered. Sex steroids may be poorly metabolized in patients with reduced liver function. Although there is no first pass hepatic metabolism with transdermal HRT, HRT should be used with caution in these patients. In case of recurrence of cholestatic jaundice or cholestatic itching, which was observed for the first time during pregnancy or previous treatment with sex hormones, it is necessary to immediately stop using the drug Klimara®. Some patients under the influence of Klimara® may develop undesirable manifestations of estrogen stimulation, such as abnormal uterine bleeding. Frequent or persistent pathological uterine bleeding during treatment is an indication for endometrial examination to exclude an organic disease. Under the influence of estrogen, uterine fibroids can increase in size. In this case, treatment should be stopped. It is recommended to discontinue treatment if endometriosis relapses during treatment with Klimara®. If prolactinoma is suspected, this disease should be excluded before starting treatment. If prolactinoma is detected, the patient should be under close medical supervision (including periodic assessment of prolactin concentrations). In some cases, chloasma may occur, especially in women with a history of chloasma during pregnancy. While using Klimara®, women with a tendency to develop chloasma should avoid prolonged exposure to the sun or exposure to ultraviolet radiation. The following conditions may occur or be aggravated by the use of Climara®. Although their relationship with the use of Klimara® has not been proven, women with the following conditions should be under medical supervision when undergoing HRT: epilepsy, benign breast diseases, bronchial asthma, migraine, porphyria, otosclerosis, systemic lupus erythematosus, chorea minor. In women with hereditary forms of angioedema, exogenous estrogens may cause or worsen symptoms of angioedema. Medical examinations Before starting or resuming taking Climara®, you should review the patient's medical history in detail and conduct a physical and gynecological examination. The frequency and nature of such examinations should be based on existing standards of medical practice with the necessary consideration of the individual characteristics of each patient (but not less than once every 6 months) and should include measurement of blood pressure, assessment of the condition of the mammary glands, abdominal and pelvic organs, including cytological examination of the cervical epithelium. In the presence of prolactinoma, periodic determination of prolactin concentration is required. Impact on the results of laboratory parameters Taking sex steroids can affect the biochemical parameters of the liver, thyroid gland, adrenal glands and kidneys, the plasma content of transport proteins, such as globulin that binds sex hormones and lipid/lipoprotein fractions, indicators of carbohydrate metabolism, coagulation and fibrinolysis . Klimara® does not have a negative effect on glucose tolerance.