Ketoprofen 50 mg/ml 2 ml N10 solution for injection
pharmachologic effect
Pharmacodynamics
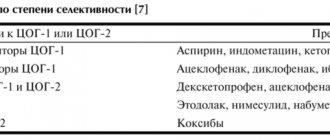
Ketoprofen is a non-steroidal anti-inflammatory drug. Ketoprofen has anti-inflammatory, analgesic and antipyretic effects. Ketoprofen blocks the action of the enzyme cyclooxygenase 1 and 2 (COX-1 and COX-2) and, partially, lipoxygenase, which leads to suppression of prostaglandin synthesis (including in the central nervous system, most likely in the hypothalamus). Stabilizes liposomal membranes in vitro and in vivo; at high concentrations in vitro, ketoprofen inhibits the synthesis of bradykinin and leukotrienes. Ketoprofen does not have a negative effect on the condition of articular cartilage. Pharmacokinetics: Absorption With intravenous administration of ketoprofen, the average plasma concentration after 5 minutes from the start of the infusion and up to 4 minutes after its cessation is 26.4 ± 5.4 mcg/ml. Bioavailability is 90%. With a single intramuscular injection of 100 mg of ketoprofen, the drug is detected in the blood plasma 15 minutes after the start of the infusion, and the peak concentration (1.3 μg/ml) is reached after 2 hours. The bioavailability of the drug increases linearly with increasing dose. Distribution Ketoprofen is 99% bound to blood plasma proteins, mainly to the albumin fraction. The volume of distribution in tissues is 0.1-0.2 l/kg. Ketoprofen penetrates into the synovial fluid, and with intravenous administration of 100 mg after 3 hours, its concentration reaches 1.5 μg/ml, which is 50% of the concentration in blood plasma (about 3 μg/ml). After 9 hours, the concentration in the synovial fluid is 0.8 μg/ml, and in the blood plasma - 0.3 μg/ml, which means that ketoprofen penetrates the synovial fluid more slowly and is removed from it more slowly. Steady-state plasma concentrations of ketoprofen are determined even 24 hours after its administration. After a single intramuscular injection of 100 mg of ketoprofen, the drug is detected in the cerebrospinal fluid, as well as in the blood serum, after 15 minutes. Metabolism Ketoprofen undergoes intensive metabolism with the participation of microsomal liver enzymes. It binds to glucuronic acid and is excreted from the body as a glucuronide. There are no active metabolites of ketoprofen. Elimination The half-life (T1/2) of ketoprofen is 2 hours. Up to 80% of ketoprofen is excreted by the kidneys within 24 hours, mainly (> 90%) in the form of ketoprofen glucuronide, and about 10% through the intestines. In patients with renal failure, ketoprofen is excreted more slowly, its T1/2 increases by 1 hour. In patients with liver failure, T1/2 increases, so accumulation of ketoprofen in tissues is possible. In elderly patients, the metabolism and elimination of ketoprofen is slower, which is of clinical significance only for patients with severe renal impairment.
Indications
Symptomatic treatment of pain syndrome, incl. in inflammatory processes of various origins: rheumatoid arthritis; seronegative arthritis: ankylosing spondylitis (Bechterew's disease), psoriatic arthritis, reactive arthritis (Reiter's syndrome); gout, pseudogout; degenerative diseases of the musculoskeletal system, incl. osteoarthritis; mild, moderate and severe pain syndrome with headaches, migraines, tendinitis, bursitis, myalgia, neuralgia, radiculitis; post-traumatic and postoperative pain syndrome, incl. accompanied by inflammation and fever; pain syndrome in cancer; algodismenorrhea. The drug is intended for symptomatic therapy, reducing pain and inflammation at the time of use, and does not affect the progression of the disease.
Contraindications
Hypersensitivity to ketoprofen or other components of the drug, as well as salicylates or other non-steroidal anti-inflammatory drugs (NSAIDs); complete or incomplete combination of bronchial asthma, recurrent polyposis of the nose and paranasal sinuses and intolerance to acetylsalicylic acid or other NSAIDs (including a history); peptic ulcer of the stomach or duodenum in the acute stage; ulcerative colitis, Crohn's disease; hemophilia and other bleeding disorders; children's age (up to 15 years); severe liver failure; severe renal failure: severe renal failure (creatinine clearance (CC) less than 30 ml/min), confirmed hyperkalemia, progressive kidney disease; decompensated heart failure; postoperative period after coronary artery bypass surgery; gastrointestinal, cerebrovascular and other bleeding (or suspected bleeding); chronic dyspepsia; III trimester of pregnancy; breastfeeding period.
special instructions
With long-term use of NSAIDs, it is necessary to periodically evaluate a clinical blood test, as well as monitor renal and liver function, especially in elderly patients (over 65 years), and conduct a stool test for occult blood. It is necessary to be careful and monitor blood pressure more often when using ketoprofen to treat patients suffering from arterial hypertension and cardiovascular diseases that lead to fluid retention in the body. If visual disturbances occur, treatment should be stopped immediately. Like other NSAIDs, ketoprofen can mask the symptoms of infectious and inflammatory diseases. If you notice signs of infection or deterioration in health while using the drug, you should immediately consult a doctor. If there is a history of contraindications from the gastrointestinal tract (bleeding, perforation, peptic ulcer), long-term therapy and the use of high dosages of ketoprofen, the patient should be under close medical supervision. Because of the important role of prostaglandins in maintaining renal blood flow, special caution should be exercised when prescribing ketoprofen to patients with cardiac or renal failure, as well as when treating elderly patients taking diuretics and patients who have a decrease in circulating blood volume for any reason ( for example, after surgery). The use of ketoprofen can affect female fertility, therefore, patients with infertility (including those undergoing examination) are not recommended to use the drug.
Compound
1 ml of the drug contains:
Active substance:
Ketoprofen 50 mg
Excipients:
Propylene glycol 400 mg Ethanol 95% 100 mg (calculated as an anhydrous substance) Benzyl alcohol 20 mg Sodium hydroxide solution 10 M to pH 6.0 - 7.5 Water for injection up to 1 ml.
Directions for use and doses
Intravenously, intramuscularly. To reduce the frequency of adverse reactions, it is recommended to use the minimum effective dose of the drug. The maximum daily dose is 200 mg. It is necessary to carefully evaluate the ratio of expected benefits and risks before starting to take ketoprofen at a dose of 200 mg/day. Intramuscular administration: 100 mg (1 ampoule) 1-2 times a day. Intravenous infusion of ketoprofen should be carried out only in a hospital setting. The duration of the infusion should be from 0.5 to 1 hour. The intravenous route of administration should be used for no more than 48 hours. Short intravenous infusion: from 100 (to 200) mg (1-2 ampoules) of ketoprofen, diluted in 100 ml of 0.9% solution sodium chloride, administered over 0.5-1 hour. Long-term intravenous infusion: from 100 (to 200) mg (1-2 ampoules) of ketoprofen, diluted in 500 ml of infusion solution (0.9% sodium chloride solution, lactated Ringer's solution , 5% dextrose solution), administered over 8 hours; re-administration is possible after 8 hours. The maximum daily dose is 200 mg. Ketoprofen can be combined with centrally acting analgesics; it can be mixed with opioids (eg morphine) in the same vial and is pharmaceutically incompatible with tramadol solution due to precipitation. Parenteral administration of the drug can be combined with the use of oral forms (tablets, capsules) or rectal suppositories
Side effects
According to the World Health Organization (WHO), adverse effects are classified according to their frequency as follows: very common (>= 1/10), common (>= 1/100, < 1/10), uncommon (>= 1/10). 1000, <1/100), rare (>= 1/10000, <1/1000) and very rare (<1/10000); frequency unknown (the frequency of events cannot be determined from the available data).
From the hematopoietic and lymphatic systems
Rarely: hemorrhagic anemia, hemolytic anemia, leukopenia. Frequency unknown: agranulocytosis, thrombocytopenia, bone marrow dysfunction.
From the immune system
Frequency unknown: anaphylactic reactions (including anaphylactic shock).
From the nervous system
Common: insomnia, depression, asthenia. Uncommon: headache, dizziness, drowsiness. Rarely: paresthesia, confusion or loss of consciousness, peripheral polyneuropathy. Frequency unknown: convulsions, taste disturbances, emotional lability.
From the senses
Rarely: blurred vision, tinnitus, conjunctivitis, dry eye mucosa, eye pain, hearing loss. Frequency unknown: optic neuritis.
From the cardiovascular system
Uncommon: tachycardia. Frequency unknown: heart failure, increased blood pressure, vasodilation.
From the respiratory system
Rarely: exacerbation of bronchial asthma, nosebleeds, laryngeal edema. Frequency unknown: bronchospasm (especially in patients with hypersensitivity to NSAIDs), rhinitis.
From the gastrointestinal tract (GIT)
Common: nausea, vomiting, dyspepsia, abdominal pain, NSAID gastropathy. Uncommon: constipation, diarrhea, bloating, gastritis. Rarely: peptic ulcer, stomatitis. Very rare: exacerbation of ulcerative colitis, Crohn's disease, gingival, gastrointestinal, hemorrhoidal bleeding, melena, perforation of the gastrointestinal tract. Frequency unknown: gastrointestinal discomfort, stomach pain.
From the liver and biliary tract
Rarely: hepatitis, increased activity of liver enzymes and bilirubin.
From the skin
Uncommon: skin rash, itching. Not known: photosensitivity, alopecia, urticaria, exacerbation of chronic urticaria, angioedema, erythema, bullous rash including Stevens-Johnson syndrome, toxic epidermal necrolysis, purpura.
From the urinary system
Rarely: cystitis, urethritis, hematuria. Very rare: acute renal failure, interstitial nephritis, nephrotic syndrome, abnormal values of renal function tests. Frequency unknown: fluid retention in the body and consequently weight gain, hyperkalemia. Other Uncommon: peripheral edema, fatigue. Rarely: hemoptysis, menometrorrhagia, shortness of breath, thirst, muscle twitching.
Drug interactions
Undesirable combinations of drugs The combined use of ketoprofen with other NSAIDs (including selective cyclooxygenase-2 inhibitors), salicylates in high doses is not recommended, due to an increased risk of gastrointestinal bleeding and ulceration of the gastrointestinal mucosa. Simultaneous use with anticoagulants (heparin, warfarin), antiplatelet agents (ticlopidine, clopidogrel) increases the risk of bleeding. If the use of such a combination is unavoidable, the patient's condition should be carefully monitored. When used simultaneously with lithium preparations, it is possible to increase the concentration of lithium in the blood plasma up to toxic values. The concentration of lithium in the blood plasma should be carefully monitored and the dose of lithium preparations should be promptly adjusted during and after treatment with NSAIDs. Increases the hematological toxicity of methotrexate, especially when used in high doses (more than 15 mg per week). The time interval between stopping or starting therapy with ketoprofen and taking methotrexate should be at least 12 hours. Combinations that must be used with caution During therapy with ketoprofen, patients taking diuretics, especially when dehydration develops, have a higher risk of developing renal failure due to a decrease in renal blood flow caused by inhibition of prostaglandin synthesis. Before starting to use ketoprofen in such patients, rehydration measures should be carried out. After starting treatment, it is necessary to monitor kidney function. Combined use of the drug with angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers in patients with impaired renal function (with dehydration, elderly patients) can lead to worsening deterioration of renal function, incl. to the development of acute renal failure. During the first weeks of simultaneous use of ketoprofen and methotrexate at a dose not exceeding 15 mg/week, blood tests should be monitored weekly. In elderly patients or if there are any signs of renal impairment, the study should be performed more frequently. Combinations that need to be taken into account Ketoprofen may weaken the effect of antihypertensive drugs (beta blockers, angiotensin-converting enzyme inhibitors, diuretics). Concomitant use with selective serotonin reuptake inhibitors (SSRIs) increases the risk of gastrointestinal bleeding. Concomitant use with thrombolytics increases the risk of bleeding. Concomitant use with potassium salts, potassium-sparing diuretics, ACE inhibitors, angiotensin II receptor blockers, NSAIDs, low molecular weight heparins, cyclosporine, tacrolimus and trimethoprim increases the risk of developing hyperkalemia. When used simultaneously with cyclosporine and tacrolimus, there may be a risk of additive nephrotoxicity, especially in elderly patients. The use of several antiplatelet drugs (tirofiban, eptifibarid, abciximab, iloprost) increases the risk of bleeding. Increases the plasma concentration of cardiac glycosides, slow calcium channel blockers, cyclosporine, methotrexate and digoxin. Ketoprofen may enhance the effect of oral hypoglycemic and some anticonvulsants (phenytoin). Concomitant use with probenecid significantly reduces the plasma clearance of ketoprofen. Nonsteroidal anti-inflammatory drugs may reduce the effectiveness of mifepristone. Taking NSAIDs should be started no earlier than 8-12 days after stopping mifepristone. Pharmaceutically incompatible with tramadol solution due to precipitation.
Overdose
In case of an overdose of ketoprofen, headache, nausea, vomiting, abdominal pain, vomiting of blood, melena, impaired consciousness, respiratory depression, convulsions, impaired renal function and renal failure may occur. In case of overdose, gastric lavage and the use of activated carbon are indicated. Treatment - symptomatic and supportive therapy; the effect of ketoprofen on the gastrointestinal tract can be weakened with the help of drugs that reduce the secretion of gastric glands (for example, proton pump inhibitors) and prostaglandins; monitoring of respiratory and cardiovascular activity; no specific antidote has been found, hemodialysis is ineffective.
Storage conditions
At a temperature not higher than 25 °C. Keep out of the reach of children.
Best before date
2 years
Ketoprofen, 50 mg/ml, solution for intravenous and intramuscular administration, 2 ml, 10 pcs.
Undesirable drug combinations
The combined use of ketoprofen with other NSAIDs (including selective cyclooxygenase-2 inhibitors), salicylates in high doses is not recommended, due to the increased risk of gastrointestinal bleeding and ulceration of the gastrointestinal mucosa. Simultaneous use with anticoagulants (heparin, warfarin), antiplatelet agents (ticlopidine, clopidogrel) increases the risk of bleeding. If the use of such a combination is unavoidable, the patient's condition should be carefully monitored.
When used simultaneously with lithium preparations, it is possible to increase the concentration of lithium in the blood plasma up to toxic values. The concentration of lithium in the blood plasma should be carefully monitored and the dose of lithium preparations should be promptly adjusted during and after treatment with NSAIDs.
Increases the hematological toxicity of methotrexate, especially when used in high doses (more than 15 mg per week). The time interval between stopping or starting therapy with ketoprofen and taking methotrexate should be at least 12 hours.
Combinations to use with caution
During therapy with ketoprofen, patients taking diuretics, especially when dehydration develops, have a higher risk of developing renal failure due to a decrease in renal blood flow caused by inhibition of prostaglandin synthesis. Before starting to use ketoprofen in such patients, rehydration measures should be carried out. After starting treatment, it is necessary to monitor kidney function.
Combined use of the drug with angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers in patients with impaired renal function (with dehydration, elderly patients) can lead to worsening deterioration of renal function, incl. to the development of acute renal failure.
During the first weeks of simultaneous use of ketoprofen and methotrexate at a dose not exceeding 15 mg per week, blood tests should be monitored weekly. In elderly patients or if there are any signs of renal impairment, the study should be performed more frequently.
Combinations to take into account
Ketoprofen may weaken the effect of antihypertensive drugs (beta blockers, ACE inhibitors, diuretics).
Concomitant use with selective serotonin reuptake inhibitors (SSRIs) increases the risk of gastrointestinal bleeding.
Concomitant use with thrombolytics increases the risk of bleeding.
Concomitant use with potassium salts, potassium-sparing diuretics, ACE inhibitors, angiotensin II receptor blockers, NSAIDs, low molecular weight heparins, cyclosporine, tacrolimus and trimethoprim increases the risk of developing hyperkalemia.
When used simultaneously with cyclosporine and tacrolimus, there may be a risk of additive nephrotoxicity, especially in elderly patients.
The use of several antiplatelet drugs (tirofiban, eptifibatide, abciximab, iloprost) increases the risk of bleeding.
Increases the plasma concentration of cardiac glycosides, slow calcium channel blockers, cyclosporine, methotrexate and digoxin.
Ketoprofen may enhance the effect of oral hypoglycemic and some anticonvulsants (phenytoin).
Concomitant use with probenecid significantly reduces the plasma clearance of ketoprofen.
Nonsteroidal anti-inflammatory drugs may reduce the effectiveness of mifepristone. NSAIDs should be started no earlier than 8–12 days after mifepristone is discontinued.
Pharmaceutically incompatible with tramadol solution due to precipitation.
Ketoprofen, solution 50 mg/ml, ampoules 2 ml, 10 pcs.
The combined use of ketoprofen with other NSAIDs (including selective COX-2 inhibitors and salicylates in high doses) is not recommended due to the increased risk of gastrointestinal bleeding and ulceration of the gastrointestinal mucosa.
Simultaneous use with anticoagulants (heparin, warfarin), antiplatelet agents (ticlopidine, clopidogrel) increases the risk of bleeding. If the use of such a combination is unavoidable, the patient's condition should be carefully monitored.
When used simultaneously with lithium preparations, it is possible to increase the concentration of lithium in the blood plasma up to toxic values. The concentration of lithium in the blood plasma should be carefully monitored and the dose of lithium preparations should be promptly adjusted during and after the use of NSAIDs.
Ketoprofen increases the hematological toxicity of methotrexate, especially when used in high doses (more than 15 mg/week). The time interval between stopping or starting therapy with ketoprofen and taking methotrexate should be at least 12 hours.
During therapy with ketoprofen, patients taking diuretics, especially if dehydration develops, have a higher risk of developing renal failure due to a decrease in renal blood flow caused by inhibition of prostaglandin synthesis. Before starting to use ketoprofen in such patients, rehydration measures should be carried out. After starting treatment, it is necessary to monitor kidney function.
The combined use of ketoprofen with ACE inhibitors and angiotensin II receptor antagonists (ARA II) in patients with impaired renal function (with dehydration, in elderly patients) can lead to worsening impaired renal function, including the development of acute renal failure.
During the first weeks of simultaneous use of ketoprofen and methotrexate at a dose not exceeding 15 mg/week, blood tests should be monitored weekly. In elderly patients or if there are any signs of renal impairment, the study should be performed more frequently.
Ketoprofen may weaken the hypotensive effect of antihypertensive drugs (beta-blockers, ACE inhibitors, diuretics).
Concomitant use of ketoprofen with selective serotonin reuptake inhibitors (SSRIs) increases the risk of gastrointestinal bleeding.
Concomitant use with thrombolytics increases the risk of bleeding.
The simultaneous use of ketoprofen with potassium salts, potassium-sparing diuretics, ACE inhibitors, ARB II, NSAIDs, low molecular weight heparins, cyclosporine, tacrolimus and trimethoprim increases the risk of developing hyperkalemia.
When used simultaneously with cyclosporine and tacrolimus, there may be a risk of additive nephrotoxicity, especially in elderly patients.
The simultaneous use of several antiplatelet drugs (tirofiban, eptifibatide, abciximab, iloprost) increases the risk of bleeding.
Ketoprofen increases the plasma concentration of cardiac glycosides, slow calcium channel blockers, cyclosporine, methotrexate and digoxin.
The combined use of ketoprofen with corticosteroids and ethanol increases the risk of developing adverse events from the gastrointestinal tract.
Ketoprofen may enhance the effect of oral hypoglycemic and some anticonvulsants (phenytoin).
Concomitant use with probenecid significantly reduces the plasma clearance of ketoprofen.
NSAIDs may reduce the effectiveness of mifepristone. Taking NSAIDs should be started no earlier than 8-12 days after stopping mifepristone.
Ketoprofen is pharmaceutically incompatible with tramadol solution due to precipitation.